The 90–90–90 targets are galvanizing global action and saving lives. Eastern and southern Africa leading the way in reducing new HIV infections by nearly 30% since 2010—Malawi, Mozambique, Uganda and Zimbabwe have reduced new HIV infection by nearly 40% or more since 2010. Concerted efforts still needed for children, adolescents, men and key populations, and in certain regions.
GENEVA/PARIS, 20 July 2017—UNAIDS has released a new report showing that for the first time the scales have tipped: more than half of all people living with HIV (53%) now have access to HIV treatment and AIDS-related deaths have almost halved since 2005. In 2016, 19.5 million of the 36.7 million people living with HIV had access to treatment, and AIDS-related deaths have fallen from 1.9 million in 2005 to 1 million in 2016. Provided that scale-up continues, this progress puts the world on track to reach the global target of 30 million people on treatment by 2020.
“We met the 2015 target of 15 million people on treatment and we are on track to double that number to 30 million and meet the 2020 target,” said Michel Sidibé, Executive Director of UNAIDS. “We will continue to scale up to reach everyone in need and honour our commitment of leaving no one behind.”
The region showing the most progress is eastern and southern Africa, which has been most affected by HIV and which accounts for more than half of all people living with HIV. Since 2010, AIDS-related deaths have declined by 42%. New HIV infections have declined by 29%, including a 56% drop in new HIV infections among children over the same period, a remarkable achievement resulting from HIV treatment and prevention efforts that is putting eastern and southern Africa on track towards ending its AIDS epidemic.
WHAT’S ON TRACK
90–90–90 progress
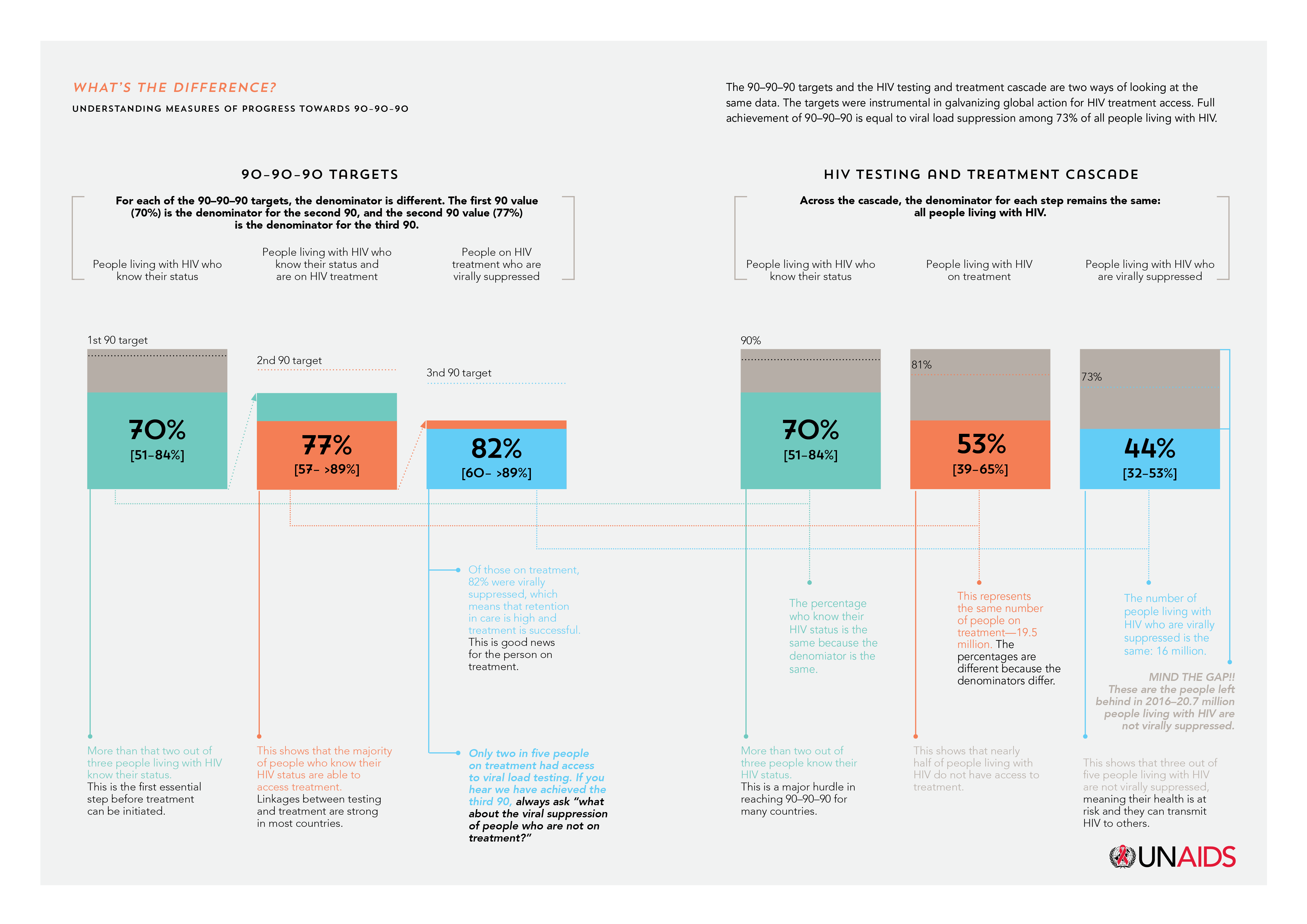
The report, Ending AIDS: progress towards the 90–90–90 targets, gives a detailed analysis of progress and challenges towards achieving the 90–90–90 targets. The targets were launched in 2014 to accelerate progress so that, by 2020, 90% of all people living with HIV know their HIV status, 90% of all people with diagnosed HIV are accessing sustained antiretroviral therapy and 90% of all people accessing antiretroviral therapy are virally suppressed.
The report shows that in 2016 more than two thirds (70%) of people living with HIV now know their HIV status. Of the people who know their status, 77% were accessing treatment, and of the people accessing treatment, 82% were virally supressed, protecting their health and helping to prevent transmission of the virus.
Eastern and southern Africa, western and central Europe and North America and Latin America are on track to reach the 90–90–90 targets by 2020. In eastern and southern Africa, 76% of people living with HIV know their HIV status, 79% of people who know their HIV-positive status have access to antiretroviral therapy and 83% of people who are on treatment have undetectable levels of HIV—this equates to 50% of all people living with HIV in eastern and southern Africa with viral suppression. The Caribbean and Asia and the Pacific can also reach the 90–90–90 targets if programmes are further accelerated.
Seven countries have already achieved the 90–90–90 targets—Botswana, Cambodia, Denmark, Iceland, Singapore, Sweden and the United Kingdom of Great Britain and Northern Ireland—and many more are close to achieving it.
“Ending AIDS is possible - it is a shared engagement and aspiration. One that cities can lead while promoting inclusive societies for all,” said Anne Hidalgo, Mayor of Paris.
The most significant impact of 90–90–90 scale-up has been in reducing AIDS-related deaths, which have been reduced by almost half in the past 10 years. As a result, life expectancy has increased significantly in the most affected countries. In eastern and southern Africa, life expectancy increased by nearly 10 years from 2006 to 2016.
“Communities and families are thriving as AIDS is being pushed back,” said Mr Sidibé. “As we bring the epidemic under control, health outcomes are improving and nations are becoming stronger.”
90-90-90: more work to do
Progress against the 90–90–90 targets has, however, been poor in the Middle East and North Africa and in eastern Europe and central Asia, where AIDS-related deaths have risen by 48% and 38%, respectively. There are exceptions within these regions showing that when concerted efforts are made, results happen. For example, Algeria has increased HIV treatment access from 24% in 2010 to 76% in 2016, Morocco from 16% in 2010 to 48% in 2016 and Belarus from 29% in 2010 to 45% in 2016.
Globally, progress has been significant, but there is still more work to do. Around 30% of people living with HIV still do not know their HIV status, 17.1 million people living with HIV do not have access to antiretroviral therapy and more than half of all people living with HIV are not virally suppressed.
Eliminating new HIV infections among children
Global solidarity to stop new HIV infections among children has produced results. Around 76% of pregnant women living with HIV had access to antiretroviral medicines in 2016, up from 47% in 2010. New HIV infections among children globally have halved, from 300 000 [230 000–370 000] in 2010 to 160 000 [100 000–220 000] in 2016. Five-high burden countries—Botswana, Namibia, South Africa, Swaziland and Uganda—have already met the milestone of diagnosing and providing lifelong antiretroviral therapy to 95% of pregnant and breastfeeding women living with HIV.
New HIV infections are declining, but not fast enough
The report also shows that, globally, new HIV infections are declining, but not at the pace needed to meet global targets. Globally, new HIV infections declined by 16% from 2010 to 2016, to 1.8 million [1.6 million–2.1 million]. Declines were estimated in 69 countries, in the majority of which treatment scale-up has been implemented alongside an increase in the availability of combination HIV prevention services and in some countries condom use. However, alarming increases have been seen in new HIV infections in eastern Europe and central Asia.
Tuberculosis
Major gains in the global response to tuberculosis and HIV led to a 33% decline in tuberculosis deaths among people living with HIV. As of 2015, only 11% of the 10.4 million cases of tuberculosis globally were among people living with HIV. However, nearly 60% of tuberculosis cases among people living with HIV were not diagnosed or treated.
Community health workers needed
Ending AIDS shows that providing services closer to where people live and work will be a key factor in ending the AIDS epidemic. UNAIDS is championing an initiative recently backed by the African Union to recruit and train 2 million community health workers in Africa to further bolster the capacity of health systems to deliver health-care services across the region.
“When health services reach the doorsteps, the health of families and communities is transformed,” said Mr Sidibé. “Community health workers will become the backbone of strong and resilient health systems across Africa.”
"I am not alone living with HIV, there are millions of us and we are determined to put an end to AIDS," said Christine Kafando, community health worker and founder of Association Espoir pour Demain. "We have the will to do it and must continue our concerted efforts."
WHAT’S OFF TRACK?
Treatment for children living with HIV
Only 43% of children living with HIV have access to antiretroviral therapy, compared to 54% of adults. Ending AIDS also reveals that as many as two thirds of children under two years old are diagnosed late and start treatment with advanced immunodeficiency, resulting in a high mortality rate for children of this age group. More action is needed to diagnose and treat children living with HIV.
Young people are lagging behind
Young people (15–24 years) are lagging behind on multiple fronts—knowledge of HIV, HIV testing, treatment and prevention. Young people continue to be at great risk of HIV infection, especially young women in sub-Saharan Africa. New HIV infections among young women in sub-Saharan Africa are 44% higher than among young men of their age in the region. Around 610 000 new HIV infections occurred among young people aged 15–24 years; 59% of those new infections occurred among young women age 15–24 years.
In Malawi, Zambia and Zimbabwe, half of young people do not know their status and more than half do not have access to HIV treatment. Only 36% of young men and 30% of young women in sub-Saharan Africa had a basic knowledge of how to protect themselves from HIV. Population-based HIV Impact Assessments (PHIAs) conducted in Malawi, Zambia and Zimbabwe, and supported by the United States President’s Emergency Plan for AIDS Relief, found that less than 50% of young people living with HIV were aware of their HIV status, compared to 78% of adults aged 35–59 years.
Men not being reached
The report reveals that less than 50% of young men know how to protect themselves from HIV infection, that men are much less likely to know their HIV status or start treatment than women and that less than 50% of men living with HIV are accessing antiretroviral therapy. Many men who are diagnosed with HIV are diagnosed late and start treatment only when they fall ill, making them much more likely to die of AIDS-related illnesses than women. Deaths from AIDS-related illnesses were 27% lower among women than among men.
Key populations
Outside of sub-Saharan Africa, key populations and their sexual partners accounted for 80% of new HIV infections in 2015 and even in sub-Saharan Africa key populations account for 25% of new HIV infections. The report outlines that efforts to reach key populations with integrated HIV services are essential and that a combination approach is needed that includes harm reduction services.
Regions off track
Eastern Europe and central Asia is the only region in the world where new HIV infections and AIDS-related deaths are both rising. New HIV infections increased from 120 000 [100 000–130 000] in 2010 to 190 000 [160 000–220 000] in 2016. People who inject drugs accounted for 42% of new HIV infections in the region. In the Russian Federation, newly reported cases of HIV increased by 75% from 2010 to 2016. Several other countries in the region—including Albania, Armenia and Kazakhstan—also have rapidly growing epidemics.
Even though access to HIV treatment in eastern Europe and central Asia has more than doubled in the past six years, still only 28% of people living with HIV have access to antiretroviral therapy, despite two out of three people living with HIV knowing their HIV status. AIDS-related deaths have increased by 38%.
In the Middle East and North Africa, just over half of people living with HIV knew their HIV status, with less than half of those on HIV treatment. Only one out of five people living with HIV was virally suppressed.
UNAIDS has been working with Doctors Without Borders and the African Union on a catch-up plan for western and central Africa, which is lagging far behind the rest of the continent. Only 42% of the 6.1 million people living with HIV in the region knew their HIV status, just 35% were accessing HIV treatment and only one in four people living with HIV were virally suppressed in 2016.
“I would like to reiterate our support for the catch-up plan for western and central Africa, launched by UNAIDS and now joined by partners. The adoption of this plan by the heads of state of the African Union is an essential step for mobilization and the efficient implementation of this plan by the countries in the region.” said Michèle Boccoz, French AIDS Ambassador.
Resources for the AIDS response continue to flatline
Resources for the AIDS response remain flat. At the end of 2016, around US$ 19 billion was available in low- and middle-income countries, with domestic resources accounting for 57% of the global total. An estimated US$ 26 billion will be needed for the global response to HIV by 2020.
“We are maximizing the use of every dollar available, but we are still US$ 7 billion short,” said Mr Sidibé. “With more international assistance, increased domestic funding, innovative financing and effective programming can end the AIDS epidemic by 2030.”
|
In 2016 an estimated:
19.5 million people were accessing antiretroviral therapy
36.7 million [30.8 million–42.9 million] people globally were living with HIV
1.8 million [1.6 million–2.1 million] people became newly infected with HIV
1.0 million [830 000–1.2 million] people died from AIDS-related illnesses
|
Ending AIDS: progress towards the 90–90–90 targets can be downloaded from unaids.org. UNAIDS is the global leader and repository of AIDS-related programme data. The full data set can be accessed at http://aidsinfo.unaids.org/
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.