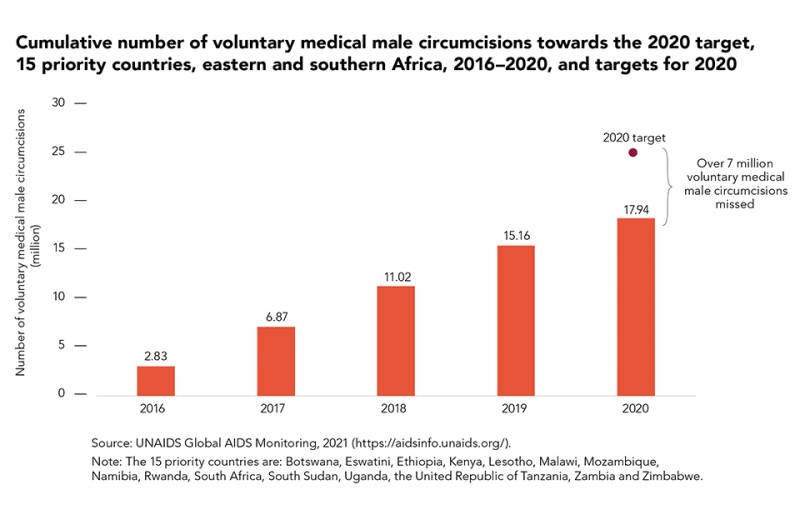
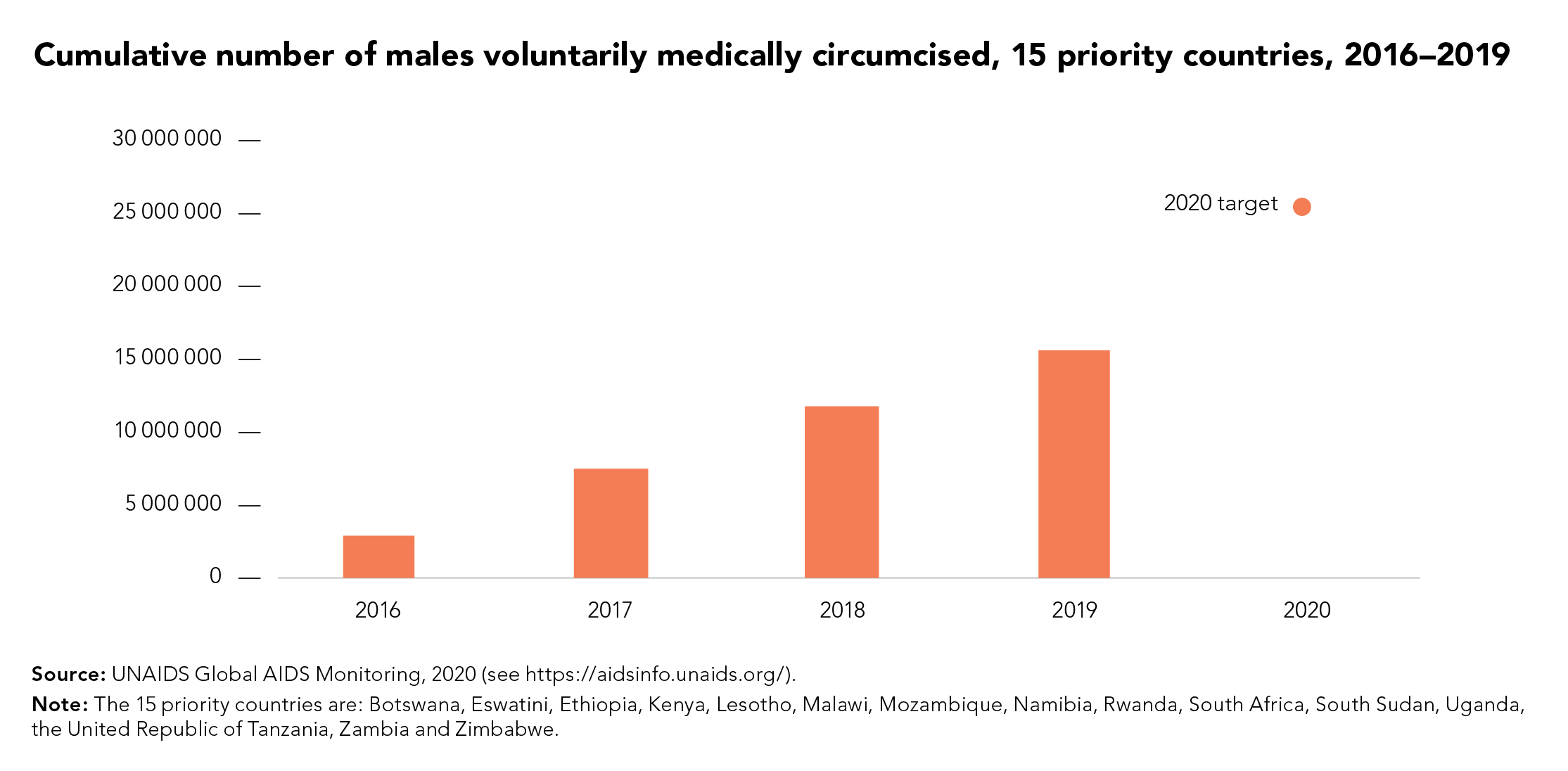
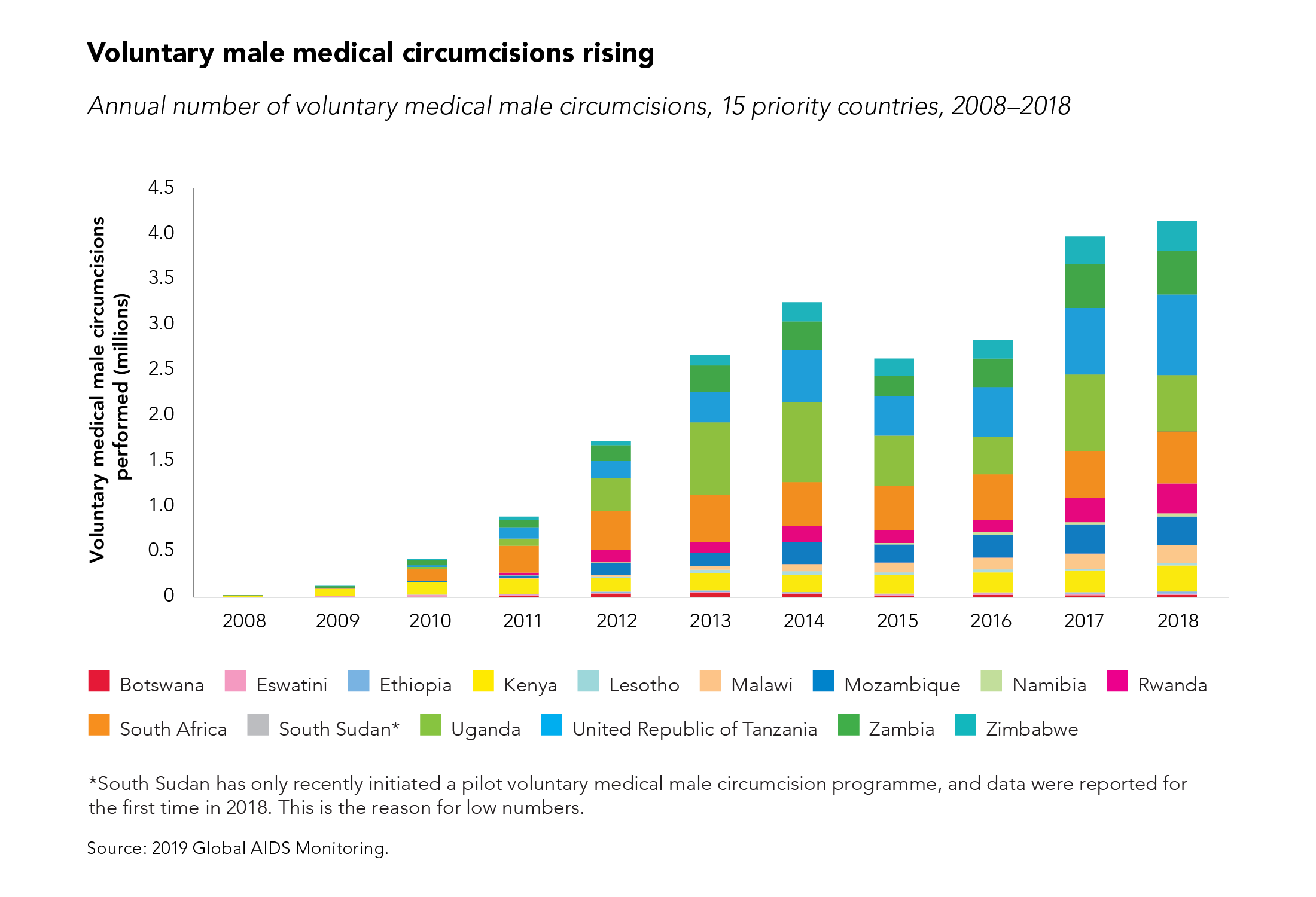
UNAIDS’ Global AIDS Update The Path that Ends AIDS underscores 2 main challenges faced by voluntary medical male circumcision (VMMC) programmes: diminished funding and low coverage among men in their twenties and older. Since VMMC was recommended by WHO and UNAIDS in 2007 as key to HIV prevention in high-prevalence settings, about 35 million men have accessed services across the 15 VMMC priority countries. While this shows good progress, the Global AIDS update highlights that VMMC coverage remains far from reaching the 90% global coverage target for impact in many subnational areas of priority countries. Additionally, funding has declined by almost half since 2020 from approximately US dollars 285 million to US dollars 147 million for the 15 countries funded by the United States President’s Emergency Plan for AIDS Relief (PEPFAR). But questions have arisen about VMMC’s cost-effectiveness under growing coverage of other biomedical interventions, such as antiretroviral treatment.
“We need strong political leadership to scale up implementation of VMMC programmes; tackle the inequalities holding back progress; and ensure sufficient and sustainable funding” said Angeli Achrekar, UNAIDS Deputy Executive Director of Programmes. “Countries that are putting people and communities first in their policies and programmes are already leading the world on the journey to ending AIDS by 2030.”
Voluntary medical male circumcision is a simple, safe procedure that has proven to reduce the risk of HIV transmission by up to 60% in heterosexual men. But is it cost effective? For how long must policy makers continue to promote VMMC among adolescent boys and adult men across VMMC priority countries? This is what a group of researchers investigated.
Now published in The Lancet Global Health and using 5 existing mathematical HIV models, the researchers aimed to assess whether providing VMMC for the next 5 years would continue to be a cost-effective use of HIV programme resources in sub-Saharan Africa. The models applied assumptions based on HIV epidemiology in VMMC priority countries focusing on Malawi, South Africa, and Zimbabwe. The impact and cost-effectiveness were projected over 50 years to capture clients’ lifetime HIV exposure and infection.
Findings reveal that a continuation of VMMC was cost-effective even in regions with low HIV incidence; VMMC was cost-effective in 62% of settings with HIV incidence of less than 1 per 100 person-years in men aged 15–49 years, increasing to 95% with HIV incidence greater than 10 per 100 person-years They underscored VMMC’s importance in continuing to avert HIV infections and related healthcare costs over time.
While details of the results varied by country and model (see Box1), overall VMMC was shown to be highly cost-effective and even cost saving in nearly all countries and scenarios.
Box 1 Varying results across countries
- South Africa: All models found continuation of VMMC to be cost saving.
- Malawi: All models found continuation of VMMC to be cost-saving
- Zimbabwe: Mixed results. Continuation of VMMC was cost-saving in one model but was not as cost-effective in the other model.
- Across a range of country and regional scenarios for sub-Saharan Africa, cost-effectiveness of VMMC was dependent on HIV incidence. Even in setting scenarios with low HIV incidence, most epidemic scenarios suggested it would be cost-effective
|
The authors concluded that despite the scale-up of antiretroviral therapy and low HIV incidence in some settings, the continuation of VMMC for at least the next 5 years is cost-effective in almost all settings considered in this study.
“Clearly, intensified efforts and commitments are needed to scale up VMMC while at the same time sustaining these services to reach men and boys,'' said Dr Meg Doherty, Director of WHO’s Global HIV, Hepatitis and STI Programmes. “The new Global AIDS report shows a widening gap for men that is important to recognize and address efficiently and effectively for their own health and to reduce new infections.’’
These analyses support a call to action on intensified efforts to reach men and boys in general and for continued funding for VMMC programmes. The discussion on VMMC sustainability is crucial. UNAIDS and WHO are urging countries to intensify their efforts in scaling up VMMC to global coverage targets (90%), at the same time address programme sustainability.
In the 2025 HIV Prevention Roadmap, VMMC remains a core component of combination HIV prevention under the pillar of men and boys. It is not only cost-effective, but also, cost-saving in many settings. Accordingly, continued progress towards male circumcision coverage targets in all the VMMC priority countries must be accelerated