
Press Release
UNAIDS Board concludes with key decisions taken related to the colliding epidemics of HIV and COVID-19
23 December 2020 23 December 2020GENEVA, 23 December 2020— The virtual 47th meeting of the UNAIDS Programme Coordinating Board (PCB) has concluded with important decisions relating to the HIV response, the COVID-19 epidemic, and the ongoing transformation of UNAIDS.
In her opening remarks to the PCB, UNAIDS Executive Director, Winnie Byanyima, thanked the United States of America for chairing the meeting and for its continued leadership in the AIDS response. In her report to the PCB on the state of the HIV epidemic, Ms Byanyima described a mixed picture of progress for some and inequality, stalled or growing danger from HIV for others. With the UNAIDS 2020 targets unmet, she warned that COVID-19 threatened to blow the HIV response even further off-track and called on the world to tackle the long-term fragilities, inequalities and injustices which continue to drive the HIV epidemic.
“A second pandemic in COVID-19 now makes the situation immeasurably more complex,” said Ms Byanyima, “Our choices are stark: get back on track by tackling inequality rapidly and head on, with the expectation that progress for some can be realized by all, or watch as we slip further behind.”
In a special address, the United Nations Deputy Secretary-General, Amina Mohammed, said that people living with HIV, key populations and community-led organizations were critical to helping shape the future of the AIDS response. She urged the PCB to prioritize the adoption of the new UNAIDS strategy with its ambitious 2025 targets so that it could inform preparations for the United Nations General Assembly High-Level Meeting on Ending AIDS expected to be held in June 2021.
“We need political will and renewed commitment to adopt this strategy, to fully fund the global AIDS response, and to fully fund UNAIDS. Together let us make this decade of action also the decade we end AIDS,” said Ms Mohammed.
During the meeting, Ms Byanyima thanked Sweden and Germany for announcing significant financial contributions to support the work of UNAIDS, demonstrating their ongoing support for the organization. The PCB concluded with a thematic segment on cervical cancer and HIV with a special address from the First Lady of Namibia, Monica Geingos.
The PCB elected Namibia as its Chair for 2021, with Thailand to serve as vice-chair and the United States of America as rapporteur.
The report to the Board by the UNAIDS Executive Director and the PCB’s decisions can be found at unaids.org/en/whoweare/pcb/47.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaMichael Hollingdale
tel. +41 79 500 2119
hollingdalem@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org


Press Release
Fund to help key populations during COVID-19 launched
10 December 2020 10 December 2020GENEVA, 10 December 2020—UNAIDS announces the launch of its Solidarity Fund, which will support social entrepreneurs and micro-business owned by key populations facing special hardship during the COVID-19 pandemic.
“Key populations are among those disproportionally impacted by COVID-19,” said Winnie Byanyima, UNAIDS Executive Director. “COVID-19 has highlighted and exacerbated the profound and widening economic and social inequalities. We must act to support and protect the people who are most impacted by the pandemic.”
Experience from the COVID-19 and HIV pandemics, and from other diseases, such as Ebola, has shown that key populations are more likely to be impacted by food insecurity, face barriers to health care and access to medicines, and suffer losses of livelihood, unemployment, homelessness and domestic violence.
Launched today, Human Rights Day, the new Solidarity Fund will support social entrepreneurs and small-scale businesses owned by people living with HIV, women or members of key populations, including sex workers, transgender people, people who use drugs and gay men and other men who have sex with men, the people who so often have their human rights violated.
“The fund will help bridge the gap between aspirations and opportunities of people from my community. It places trust and gives us a chance to show our innovation and entrepreneurship with no limitations,” said Maite Schneider, the cofounder and Chief Executive Officer of TransEmpregos.
To be piloted initially in five countries—Brazil, Ghana, India, Madagascar and Uganda—with a US$ 250 000 budget from UNAIDS, the initiative will scale up to additional countries over the coming months, with a goal of raising an additional US$ 3 million to US$ 5 million in 2021–2022.
UNAIDS will closely work with community networks, national innovation ecosystems, the private sector and other partners to create tailored support, especially capacity development on social entrepreneurship and mentoring to enhance the sustainability of social ventures and impact for the wider community, with special attention given to young key populations.
Among the partners is the venture development and investment platform Social Alpha, which will provide mentoring and entrepreneur support to the chosen beneficiaries. “We look forward to partner with communities and UNAIDS on the Solidarity Fund and leverage our experience in working with social entrepreneurs for solving complex social, economic and environmental challenges,” said Manoj Kumar, the Chief Executive Officer and founder of Social Alpha.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)





Press Release
UNAIDS calls on more to be done for paediatric HIV treatment in the Democratic Republic of the Congo
02 December 2020 02 December 2020On World AIDS Day, the UNAIDS Executive Director visited an HIV community village and a children’s hospital
Kinshasa, 2 December 2020—UNAIDS Executive Director Winnie Byanyima visited an HIV community village in Kinshasa as part of the World AIDS Day ceremonies in the capital of the Democratic Republic of the Congo. She commended the country on its vast experience in responding to pandemics such as Ebola after the country announced the end of the latest Ebola outbreak on 18 November.
“I thank the Congolese government, our friends from civil society and partners who together have enabled the country to respond to its many challenges, particularly HIV, Ebola and now COVID-19,” said Ms Byanyima.
Ms Byanyima stressed that more people in the country need life-saving HIV treatment and that more needs to be done to support women in particular. “Despite considerable progress, only 57% of people living with HIV are on antiretroviral therapy,” Ms Byanyima said. “Coverage of antiretroviral therapy is higher among men (72%) than among women (51%), a real sign of gender inequality.” She added that if women do not feel safe to disclose their HIV status or feel that they will be supported or accepted if they are living with HIV, they will not enrol onto HIV treatment.
Out of the 520 000 people living with HIV in the Democratic Republic of the Congo, more than 64% are women. There are 68 000 children under the age of 14 years who are living with HIV in the country, of whom only 25% are on treatment, which is why Ms Byanyima called on the country to accelerate paediatric care, including HIV services.
At the Kalembelembe Children’s Hospital she spoke to staff and adolescents who have grown up accessing care and support at its paediatric centre. The adolescents asked the Executive Director to continue to advocate for funding to maintain peer support groups for adolescents living with HIV, the elimination of user fees, the inclusion of all adolescents living with HIV in education and the elimination of legal barriers requiring parental consent for HIV testing for adolescents.
HIV in the Democratic Republic of the Congo, like in the rest of sub-Saharan Africa, particularly affects young women. Ms Byanyima reiterated that to end AIDS, the focus must be put on women and girls. “Every week, 4500 young women in sub-Saharan Africa are infected with HIV,” she said. “This is unacceptable, we need to make a radical difference in the response to HIV.”
Upon her arrival in Kinshasa, Ms Byanyima met with the Minister of Health, Eteni Longondo. She congratulated him on his leadership in responding to COVID-19 and shared her concerns about keeping HIV at the top of the agenda, despite the multitude of pressures of the three colliding pandemics of Ebola, HIV and COVID-19.
AIDS-related deaths in the Democratic Republic of the Congo have dropped by 61% in the past 10 years, from 37 000 in 2010 to 15 000 in 2019. HIV prevalence hovers around 1% among adults, but 23 000 people became newly infected with HIV last year.
Bold ambitious targets
UNAIDS’ new report, Prevailing against pandemics by putting people at the centre, calls on countries to make far greater investments in global pandemic responses and to adopt a new set of bold, ambitious but achievable HIV targets. If those targets are met, the world will be back on track to ending AIDS as a public health threat by 2030.
The global AIDS response was off track before the COVID-19 pandemic hit, but the rapid spread of the coronavirus has created additional setbacks. Modelling of the pandemic’s long-term impact on the HIV response shows that there could be an estimated 123 000 to 293 000 additional new HIV infections and 69 000 to 148 000 additional AIDS-related deaths between 2020 and 2022.
“The collective failure to invest sufficiently in comprehensive, rights-based, people-centred HIV responses has come at a terrible price,” said Winnie Byanyima, Executive Director of UNAIDS. “Implementing just the most politically palatable programmes will not turn the tide against COVID-19 or end AIDS. To get the global response back on track will require putting people first and tackling the inequalities on which epidemics thrive.”
Getting back on track
Although some countries in sub-Saharan Africa, such as Botswana and Eswatini, have done remarkably well and have achieved or even exceeded the HIV targets set for 2020, many more countries are falling way behind. The high-performing countries have created a path for others to follow. UNAIDS has worked with its partners to distil those lessons into a set of proposed targets for 2025 that take a people-centred approach.
The targets focus on a high coverage of HIV and reproductive and sexual health services together with the removal of punitive laws and policies and on reducing stigma and discrimination. They put people at the centre, especially the people most at risk and the marginalized—young women and girls, adolescents, sex workers, transgender people, people who inject drugs and gay men and other men who have sex with men.
New HIV service delivery targets aim at achieving a 95% coverage for each sub-population of people living with and at increased risk of HIV. By taking a person-centred approach and focusing on the hotspots, countries will be better placed to control their epidemics.
The 2025 targets also require ensuring a conducive environment for an effective HIV response and include ambitious antidiscrimination targets so that less than 10% of countries have punitive laws and policies, less than 10% of people living with and affected by HIV experience stigma and discrimination and less than 10% experience gender inequality and violence.
Our work
Region/country

Press Release
UNAIDS calls on countries to step up global action and proposes bold new HIV targets for 2025
26 November 2020 26 November 2020As COVID-19 pushes the AIDS response even further off track and the 2020 targets are missed, UNAIDS is urging countries to learn from the lessons of underinvesting in health and to step up global action to end AIDS and other pandemics
GENEVA, 26 November 2020—In a new report, Prevailing against pandemics by putting people at the centre, UNAIDS is calling on countries to make far greater investments in global pandemic responses and adopt a new set of bold, ambitious but achievable HIV targets. If those targets are met, the world will be back on track to ending AIDS as a public health threat by 2030.
The global AIDS response was off track before the COVID-19 pandemic hit, but the rapid spread of the coronavirus has created additional setbacks. Modelling of the pandemic’s long-term impact on the HIV response shows that there could be an estimated 123 000 to 293 000 additional new HIV infections and 69 000 to 148 000 additional AIDS-related deaths between 2020 and 2022.
“The collective failure to invest sufficiently in comprehensive, rights-based, people-centred HIV responses has come at a terrible price,” said Winnie Byanyima, Executive Director of UNAIDS. “Implementing just the most politically palatable programmes will not turn the tide against COVID-19 or end AIDS. To get the global response back on track will require putting people first and tackling the inequalities on which epidemics thrive.”
New targets for getting back on track
Although some countries in sub-Saharan Africa, such as Botswana and Eswatini, have done remarkably well and have achieved or even exceeded the targets set for 2020, many more countries are falling way behind. The high-performing countries have created a path for others to follow. UNAIDS has worked with its partners to distil those lessons into a set of proposed targets for 2025 that take a people-centred approach.
The targets focus on a high coverage of HIV and reproductive and sexual health services together with the removal of punitive laws and policies and on reducing stigma and discrimination. They put people at the centre, especially the people most at risk and the marginalized—young women and girls, adolescents, sex workers, transgender people, people who inject drugs and gay men and other men who have sex with men.
New HIV service delivery targets aim at achieving a 95% coverage for each sub-population of people living with and at increased risk of HIV. By taking a person-centred approach and focusing on the hotspots, countries will be better placed to control their epidemics.
The 2025 targets also require ensuring a conducive environment for an effective HIV response and include ambitious antidiscrimination targets so that less than 10% of countries have punitive laws and policies, less than 10% of people living with and affected by HIV experience stigma and discrimination and less than 10% experience gender inequality and violence.
Prevailing against pandemics
Insufficient investment and action on HIV and other pandemics left the world exposed to COVID-19. Had health systems and social safety nets been even stronger, the world would have been better positioned to slow the spread of COVID-19 and withstand its impact. COVID-19 has shown that investments in health save lives but also provide a foundation for strong economies. Health and HIV programmes must be fully funded, both in times of plenty and in times of economic crisis.
“No country can defeat these pandemics on its own,” said Ms Byanyima. “A challenge of this magnitude can only be defeated by forging global solidarity, accepting a shared responsibility and mobilizing a response that leaves no one behind. We can do this by sharing the load and working together.”
There are bright spots: the leadership, infrastructure and lessons of the HIV response are being leveraged to fight COVID-19. The HIV response has helped to ensure the continuity of services in the face of extraordinary challenges. The response by communities against COVID-19 has shown what can be achieved by working together.
In addition, the world must learn from the mistakes of the HIV response, when millions in developing countries died waiting for treatment. Even today, more than 12 million people still do not have access to HIV treatment and 1.7 million people became infected with HIV in 2019 because they did not have access to essential HIV services.
Everyone has a right to health, which is why UNAIDS has been a leading advocate for a People’s Vaccine against COVID-19. Promising COVID-19 vaccines are emerging, but we must ensure that they are not the privilege of the rich. Therefore, UNAIDS and partners are calling on pharmaceutical companies to openly share their technology and know-how and to wave their intellectual property rights so that the world can produce successful vaccines at the huge scale and speed required to protect everyone.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)


Press Release
UNAIDS and the National Center for Global Health and Medicine in Japan bolster collaboration to end AIDS
26 November 2020 26 November 2020TOKYO/GENEVA, 26 November 2020—UNAIDS and the National Center for Global Health and Medicine (NCGM) in Japan are joining forces to end AIDS in Japan. The two organizations today signed a memorandum of understanding to promote the response to HIV and sexually transmitted infections ahead of and during the Olympic and Paralympic Games and to promote the Fast-Track cities initiative to end AIDS by 2030.
“This new partnership further strengthens the long-standing cooperation between UNAIDS and Japan,” said Winnie Byanyima, Executive Director of UNAIDS. “Japan’s strong leadership and commitment to global health, at a time when the world is fighting COVID-19, is highly commendable and we look forward to working together closely on responding to the colliding pandemics of HIV and COVID-19.”
Japan has been firmly engaged in the global AIDS response for many years. In 2000, Japan introduced infectious diseases on the agenda of the Group of Eight summit in Okinawa, paving the way for the establishment of the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund). Japan remains a strong supporter of the Global Fund and is one its leading donors.
“This partnership will enable communities and health-care providers to work together in the response to HIV, sexually transmitted infections and COVID-19,” said Shinichi Oka, the Director of the AIDS Clinical Center of NCGM.
Through the memorandum of understanding, UNAIDS and NCGM will promote awareness of HIV, including HIV prevention, during the Olympic and Paralympic Games, which are due to open in Tokyo in July 2021. The games, which usually draw millions of people, were scheduled to take place in 2020 but were postponed to 2021 due to COVID-19.
UNAIDS and NCGM will also be working together to promote the Fast-Track cities initiative, which supports cities and municipalities to take transformative action to ensure equitable access to HIV services and to reduce stigma and discrimination.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Region/country


Press Release
UNAIDS and UNFPA launch the fourth annual progress report of the Global HIV Prevention Coalition
23 November 2020 23 November 2020GENEVA, 23 November 2020—The latest progress report of the Global HIV Prevention Coalition shows that despite observed declines in new HIV infections among adults in several countries, overall progress in HIV prevention efforts remains variable and is too slow to reach the 2020 targets committed to at the 2016 United Nations High-Level Meeting on Ending AIDS.
“We can’t end AIDS if year after year people continue to become newly infected with HIV,” said Winnie Byanyima, Executive Director of UNAIDS. “This year is a milestone for taking stock of a decade of progress towards ending AIDS by 2030. Sadly, the world has come up short against the commitments made to drastically reduce new HIV infections.”
In 2016, United Nations Member States committed to reach a worldwide HIV prevention target of fewer than 500 000 new HIV infections among adults by 2020, a 75% reduction from 2010. By the end of 2019, the reduction was just 23%, with 1.7 million people becoming infected with HIV last year.
Launched in 2017, the Global HIV Prevention Coalition aims to bring fresh momentum and clarity to HIV prevention programmes in 28 focus countries—the 28 countries worldwide with the greatest burden of new HIV infections. The 28 coalition countries have identified and promoted priority programme approaches and interventions, rekindled political commitment for HIV prevention and guided and supported programme implementation.
Progress in reducing new HIV infections in coalition countries is varied. In Eswatini, for example, new HIV infections declined by 64% between 2010 and 2019. In Pakistan, on the other hand, there was a 74% increase. But in 26 coalition countries new HIV infections declined.
The report notes that there has been significant progress in implementing 10 strategic actions set out in the Global HIV Prevention 2020 Road Map, but a number of countries still have difficulties in changing underlying factors that hold back effective HIV prevention programmes, including shortfalls in financing, insufficient action on addressing the obstructive legal, policy and structural barriers that hinder programmes for key and vulnerable populations and the slow adoption of guidance on social contracting.
“To drastically reduce new HIV infections, we have to bridge the gaps and dismantle barriers that deny adolescent girls, young women and key populations access to quality, respectful sexual and reproductive health services. It’s time to end, once and for all, all forms of stigma, discrimination and marginalization that stand in their way,” said Natalia Kanem, Executive Director of the United Nations Population Fund.
The COVID-19 pandemic is an additional challenge to maintaining progress in HIV prevention this year. Of particular concern are disruptions in HIV prevention services such as voluntary medical male circumcision, interrupted access to prevention commodities, including safe injection supplies, the effects of lockdowns on educational and social support services and the interplay between economic downturns and heightened HIV risk behaviours and vulnerability. This year’s report therefore begins to document adaptations that countries are taking to mitigate the potential effects of the COVID-19 pandemic.
The progress report was launched at a virtual meeting of ministers of health from Global HIV Prevention Coalition focus countries at which members took stock of the progress to date, with the aim of charting a way forward for the next five years on the road to ending AIDS by 2030.
“HIV prevention will be at the core to the new global AIDS strategy for the next five years,” added Ms Byanyima. “Together with the United Nations Population Fund and the rest of the UNAIDS Joint Programme, we will support the Global HIV Prevention Coalition to reach our ultimate goal of zero new HIV infections.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Our work
Press centre
Download the printable version (PDF)

Press Release
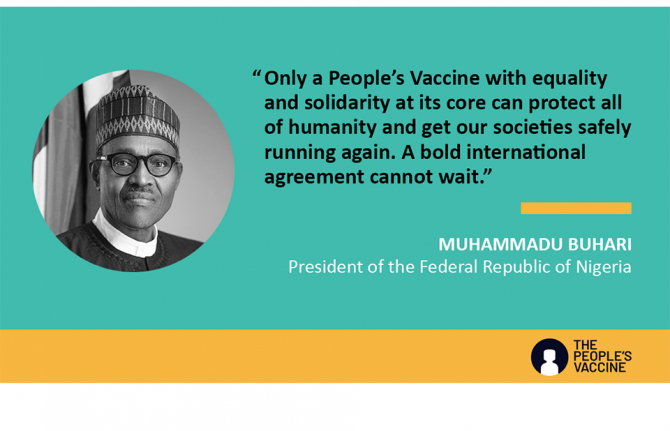
President of Nigeria unites behind the call for a People’s Vaccine for COVID-19
16 October 2020 16 October 2020GENEVA, 16 October 2020—The President of Nigeria, Muhammadu Buhari, has announced that Nigeria will be joining the urgent global call for a People’s Vaccine for COVID-19. The President endorsed the initiative and released an official public statement in favour of the campaign.
“Learning from the painful lessons from a history of unequal access in dealing with diseases such as HIV we must heed the warning that “those who do not remember the past are doomed to repeat it”,” said Mr Buhari. “Only a People’s Vaccine with equality and solidarity at its core can protect all of humanity and get our societies safely running again. A bold international agreement cannot wait.”
Nigeria is the most populous country in Africa, home to more than 200 million people, and has the third highest number of COVID-19 cases in Africa after South Africa and Ethiopia. In March 2020, Mr Buhari set up a multisectoral Presidential Task Force to combat the COVID-19 pandemic, which produced a mid-term report in July 2020 outlining a significant body of work undertaken to stop the spread of COVID-19.
However, the report also shows that the health infrastructure and equipment levels in Nigeria are not strong enough to support a sustained national response to COVID-19 and that if the pandemic were to spread exponentially Nigeria would struggle to mount an effective response. This demonstrates the urgent need for access to a vaccine for COVID-19 in Nigeria as soon as it becomes available.
“UNAIDS and other members of the People’s Vaccine Alliance are calling for a new approach that puts public health first by sharing knowledge and maximizing supply to make sure that no one is left behind,” said Winnie Byanyima, Executive Director of UNAIDS. “Anything short of that will lead to more deaths and economic chaos, forcing millions into destitution.”
The People’s Vaccine Alliance is a coalition of organizations and activists united under a common aim of campaigning for a People’s Vaccine for COVID-19. In support of actions taken by the World Health Organization (WHO), including the COVID-19 Technology Access Pool, the People’s Vaccine Alliance demands that all vaccines, treatments and tests be monopoly-free, mass produced, distributed fairly and made available to all people, in all countries, free of charge.
“The People’s Vaccine will go far in levelling the power dynamics that perpetuate inequality and fuel injustice and it will ensure that no one is left behind,” said Edward Kallon, United Nations Resident Coordinator and Humanitarian Coordinator in Nigeria. “Nobody should be denied a COVID-19 vaccine because of where they live or how much money they have—it has to be a global public good, available to all who need it, regardless of their situation.”
The People’s Vaccine Alliance is calling on pharmaceutical corporations and governments to:
- Prevent monopoly on vaccine production by making public funding for research and development conditional on research institutions and pharmaceutical companies sharing all information, data, biological material, know-how and intellectual property. The WHO COVID-19 Technology Access Pool provides the mechanism for such sharing.
- Prevent monopoly on vaccine supply by enabling as many manufacturers as possible, including in developing countries, to produce the vaccines.
- Implement fair allocation of the vaccine that prioritizes health workers and other at-risk groups in all countries. Vaccination programmes should include marginalized groups, including refugees, prisoners and people living in slums and other crowded housing conditions. Allocation between and within countries should be based on need and not ability to pay.
- Provide the vaccine free of charge at the point of use.
- Ensure the full participation of the governments of developing countries as well as global civil society in decision-making forums about the vaccines (and other COVID-19 technologies) and ensure transparency and accountability of all decisions.
To date, the People’s Vaccine has been endorsed by more than 140 leaders and advocates globally, including the President of South Africa and the Chairperson of the African Union Commission, the Presidents of Ghana and Senegal, the Prime Minister of Pakistan, the Director of the Africa Centres for Disease Control and Prevention and the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health.
The People’s Vaccine Alliance
The People’s Vaccine Alliance is a coalition of organisations and activists united under a common aim of campaigning for a People’s Vaccine’ for COVID-19 that is based on shared knowledge and is freely available for all. A global common good. It is coordinated by Oxfam and UNAIDS and its other members include: Free the Vaccine, Frontline AIDS, Global Justice Now, International Treatment Preparedness Coalition, Just Treatment, Nizami Ganjavi International Center, Open Society Foundations, STOPAIDS, SumOfUs, Wemos and Yunus Centre.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Our work
Press centre
Download the printable version (PDF)
Region/country

Press Release
UNAIDS issues guidance on reducing stigma and discrimination during COVID-19 responses
08 October 2020 08 October 2020GENEVA, 8 October 2020—Drawing on 40 years of experience from the AIDS response, UNAIDS is issuing new guidance on how to reduce stigma and discrimination in the context of COVID-19. The guidance is based on the latest evidence on what works to reduce HIV-related stigma and discrimination and applies it to COVID-19.
Since the start of the COVID-19 pandemic, numerous forms of stigma and discrimination have been reported, including xenophobia directed at people thought to be responsible for bringing COVID-19 into countries, attacks on health-care workers and verbal and physical abuse towards people who have recovered from COVID-19. Attacks on populations facing pre-existing stigma and discrimination, including people living with HIV, people from gender and sexual minorities, sex workers and migrants, have also been reported.
“In the wake of the fear and uncertainty that emerge during a pandemic, stigma and discrimination quickly follows,” said Winnie Byanyima, Executive Director of UNAIDS. “Stigma and discrimination is counterproductive. It exposes people to violence, harassment and isolation, stops people from accessing health services and prevents public health measures from effectively controlling pandemics.”
Addressing stigma and discrimination in the COVID-19 response provides countries with rights-based guidance through education, support, referrals and other interventions. It offers solutions across six specific areas: community, workplace, education, health care, justice and emergency/humanitarian settings.
As with the HIV epidemic, stigma and discrimination can significantly undermine responses to COVID-19. People who have internalized stigma or anticipate stigmatizing attitudes are more likely to avoid health-care services and are less likely to get tested or admit to symptoms, ultimately sending the pandemic underground.
“We know what works and what doesn’t, we know how to change beliefs and behaviour. For the last 30 years we have been successfully leading the HIV response, building valuable experience, knowledge and wisdom along the way,” said Alexandra Volgina, Programme Coordinator, Global Network of People Living with HIV. “We want to share these to change people’s lives for the better, and to make our distinctive contribution to overcoming the COVID-19 pandemic.”
Some countries have used existing criminal laws or new, COVID-19-specific laws, to criminalize alleged exposure or transmission of COVID-19, putting more people in overcrowded prisons, detention centres and other closed settings where COVID-19 is easily transmitted.
“There is no greater manifestation of stigma than when it is enshrined in law. The use of the criminal law or other unjustified and disproportionate repressive measures in relation to COVID-19 is having a devastating impact on the most vulnerable in society, including many people living with HIV, exacerbating inequalities and perpetuating stigma,” said Edwin J. Bernard, Executive Director of the HIV Justice Network. “Measures that are respectful of human rights and empowering of communities will be infinitely more effective than punishment and imprisonment. We hope that these evidence-based recommendations on reducing COVID-related stigma and discrimination will make a difference to those who need it most.”
Reports in the early days of COVID-19 include discrimination related to gender and gender-based violence, targeting of key populations, including sex workers, and arrests and beatings of lesbian, gay, bisexual, transgender and intersex people. In April 2020, following a number of reports of violence and stigma and discrimination arising from the implementation of COVID-19 measures, UNAIDS began to identify the actions needed to respond, and in August UNAIDS issued a report, Rights in a pandemic, that highlights many of the human rights abuses that took place early in the response to COVID-19.
The new guidance, Addressing stigma and discrimination in the COVID-19 response: applying the evidence of what works from HIV-related stigma and discrimination in six settings to the COVID-19 response, is part of efforts by UNAIDS and the Global Partnership to Eliminate All Forms of HIV-Related Stigma and Discrimination to accelerate progress on the goal of zero discrimination, in line with the political commitments that United Nations Member States made in the 2016 Political Declaration on Ending AIDS and in Sustainable Development Goal 3, ending AIDS as a public health threat by 2030.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Our work
Press centre
Download the printable version (PDF)

Press Release
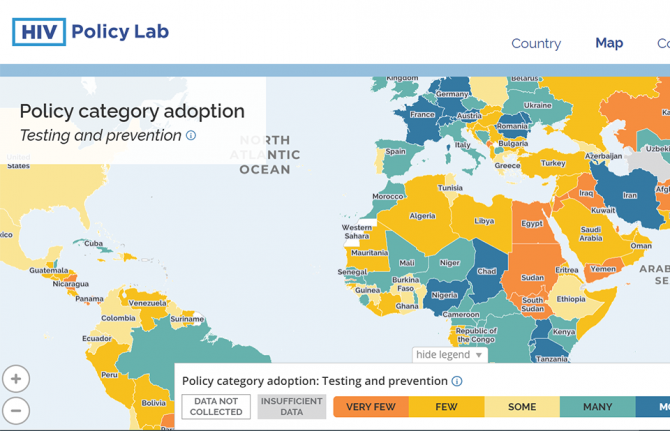
New HIV Policy Lab uses law and policy data in the HIV response
29 September 2020 29 September 2020WASHINGTON, D.C./GENEVA, 29 September 2020—Despite decades of scientific advance in the HIV response, progress remains uneven, with some countries rapidly reducing AIDS-related deaths and new HIV infections and others seeing increasing epidemics. Laws and policies are driving a significant part of that divergence.
Launched today, the HIV Policy Lab is a unique initiative to gather and monitor HIV-related laws and policies around the world.
“Laws and policies are life or death issues when it comes to HIV. They can ensure access to the best that science has to offer and help people to realize their rights and live well, or they can be barriers to people’s well-being. Like anything that matters, we need to measure the policy environment and work to transform it as a key part of the AIDS response,” said Winnie Byanyima, UNAIDS Executive Director.
The HIV Policy Lab is a data visualization and comparison tool that tracks national policy across 33 different indicators in 194 countries around the world, giving a measure of the policy environment. The goal is to improve transparency, the ability to understand and use the information easily and the ability to compare countries, supporting governments to learn from their neighbours, civil society to increase accountability and researchers to study the impact of laws and policies on the HIV pandemic.
According to Matthew Kavanagh, Director of the Global Health Policy & Politics Initiative at Georgetown University’s O’Neill Institute, “Policy is how governments take science to scale. If we want to improve how policy is used to improve health outcomes, it is essential to monitor and evaluate the policies that comprise it.”
“Reducing stigma and making care easier to access are fundamental for improving the lives of people living with HIV—and those are all consequences of policy choices. Tracking these choices is a key tool for improving them, and ensuring justice and equity for people living with HIV,” said Rico Gustav, Executive Director of the Global Network of People Living with HIV.
The HIV Policy Lab draws information from the National Commitments and Policy Instrument, legal documents, government reports and independent analyses to create data sets that can be compared across countries and across issues. The goal of the HIV Policy Lab is to help identify and address the gaps between evidence and policy and to build accountability for a more inclusive, effective, rights-based and science-based HIV policy response.
The HIV Policy Lab is a collaboration between Georgetown University and the O’Neill Institute for National and Global Health Law, UNAIDS, the Global Network of People Living with HIV and Talus Analytics.
About the Georgetown University O’Neill Institute for National and Global Health Law
The O’Neill Institute, housed at Georgetown University, was established to create innovative solutions to the most pressing national and international health concerns, with the essential vision that the law has been, and will remain, a fundamental tool for solving critical health problems. The Georgetown University Department of International Health is home to scholarship in public health, economics, political science, and medicine. Georgetown’s Global Health Initiative serves as a university-wide platform for developing concrete solutions to the health challenges facing families and communities throughout the world. Read more at oneillinstitute.org and connect with us on Twitter and Facebook.
About UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
About GNP+
GNP+ is the global network for and by people living with HIV. GNP+ works to improve the quality of life of all people living with HIV. GNP+ advocates for, and supports fair and equal access to treatment, care and support services for people living with HIV around the world. Learn more at gnpplus.net and connect with GNP+ on Facebook, Twitter and Instagram.
Contact
O’Neill InstituteLauren Dueck
Lauren.Dueck@Georgetown.edu
UNAIDS
Sophie Barton-Knott
bartonknotts@unaids.org
GNP+
Lesego Tlhwale
ltlhwale@gnpplus.net
Press centre
Download the printable version (PDF)


Press Release
As pandemic deaths pass 1 million, COVID survivors from 37 countries write to pharmaceutical bosses to demand a People's Vaccine
29 September 2020 29 September 2020GENEVA, 29 September 2020—Survivors of COVID-19 from 37 countries are among almost 1,000 people who have signed an open letter to pharmaceutical industry leaders calling for a ‘people's vaccine’ and treatments that are available to all – free from patents. The letter comes on the eve of a high-level side event about the pandemic at the UN General Assembly in New York tomorrow (30 September).
The signatories include 242 COVID-19 survivors from South Africa to Finland and New Zealand to Brazil. They also include 190 people in 46 countries who have lost relatives to the virus, and 572 signatories with underlying health conditions that mean they are more likely to develop severe forms of COVID-19 and have a greater risk of dying from it.
The letter says: “Some of us have lost loved ones to this killer disease. Some of us have come close to death ourselves. Some of us are continuing to live in fear that contracting this disease would be fatal for us. We see no justification why your profit or monopolies should mean anyone else should go through this.”
It describes pharmaceutical corporations as “carrying on with business as usual - defending monopolies while refusing to share research and know-how” and calls on industry leaders to “ensure COVID-19 vaccines and treatments reach everyone who needs them by preventing monopolies, ramping up production and sharing knowledge.”
Pharmaceutical monopolies will restrict the production of effective vaccines and treatments to a small number of manufacturers, preventing the mass production that is needed to meet global demand. The letter demands that corporations immediately license vaccine technology and intellectual property rights to the WHO COVID-19 Technology Access Pool (C-TAP).
One of the signatories, Dilafruz Gafurova, 43, from Tajikistan, said: “Me and my husband got sick with this disease. We could only rely on ourselves as hospitals were full … It was really difficult to get the right medicines. I am a mother of four children … I was afraid to leave them alone in this world if something bad could happen with me … The reason I am signing this letter is to help others to get [a] vaccine. Not all the people around the world can get this vaccine, as they simply cannot afford it. They hardly [have enough to meet] their daily needs.”
The letter was organised by the People's Vaccine Alliance, a global coalition of organisations and activists united under a common aim of campaigning for a people’s vaccine for COVID-19 that is based on shared knowledge and is freely available to everyone everywhere.
Tomorrow at the UN General Assembly, Bill Gates and UK Prime Minister Boris Johnson will be among other high-profile figures discussing vaccine access. So far rich nations have failed to exert pressure on pharmaceutical corporations to share technology to maximise the supply of successful vaccines and treatments worldwide.
Heidi Chow from Global Justice Now, a member of the People’s Vaccine Alliance said: “Pharmaceutical companies need to pay attention to the demands of people from around the world who have experienced the fear and devastation of COVID-19. The industry cannot block its ears to these voices but should respond immediately by ending their monopolies and commit to sharing manufacturing know-how. These actions are crucial to expand vaccine supplies so that all countries can affordably access effective vaccines.”
Winnie Byanyima, Executive Director of UNAIDS, said: "With AIDS we saw that when treatments were found the wealthier people in wealthier countries got back to health, while millions of people in developing countries were left to die. We must not repeat the same mistake when a vaccine for COVID-19 is found. The right to health is a human right—it should not depend on the money in your pocket or the colour of your skin to be vaccinated against this deadly virus. A vaccine should be a global public good and free of charge for all."
A COVID-19 VACCINE FOR ALL
The Alliance is also calling on governments to make public funding for research and development of COVID-19 diagnostics, vaccines and treatments conditional on pharmaceutical companies sharing their knowledge and technology free from patents. When an effective vaccine is available, the Alliance demands that doses are fairly distributed with priority given to health workers and other at-risk groups in all countries.
Notes to editors:
Read the full text of the letter
The high-level side events, titled Accelerating the end of the COVID-19 pandemic: taking new solutions to scale and making them equitably accessible, to save lives, protect health systems and restart the global economy, will take place on 30 September at the 75th session of the UN General Assembly in New York. Among the participants are the UN Secretary General, WHO Director General, leaders of a range of countries including the UK and South Africa and UNAIDS Executive Director Winnie Byanyima.
The open letter has been signed by 941 people. They include 242 COVID-19 survivors from the following 37 countries: Australia, Azerbaijan, Bangladesh, Belgium, Brazil, Burundi, Canada, Denmark, Finland, France, Germany, India, Ireland, Italy, Japan, Kenya, Lebanon, Morocco, Netherlands, New Zealand, Nicaragua, Pakistan, Philippines, Poland, Portugal, Republic of North Macedonia, Russia, Senegal, Slovenia, South Africa, Spain
Sweden, Tajikistan, Uganda, UK, USA and Zambia. Some people fell into more than one category and a list of the signatories is available on request. The letter has been sent to the pharmaceutical companies behind the 11 vaccine candidates that are currently in Phase 3 trials.
People’s Vaccine Alliance is a coalition of organisations and activists united under a common aim of campaigning for a ‘people’s vaccine’ for COVID-19 that is based on shared knowledge and is freely available to everyone everywhere. A global common good. It is coordinated by Oxfam and UNAIDS and its members include Frontline AIDS, Global Justice Now, Nizami Ganjavi International Center, STOPAIDS, Wemos and the Yunus Centre. More than 140 world leaders, former leaders and economists have called on governments to unite behind a people’s vaccine against COVID-19.
Earlier this month, an analysis by Oxfam revealed that a small group of wealthy nations representing just 13 percent of the world’s population have already bought up more than half (51 percent) of the future doses of leading COVID-19 vaccine candidates.
