

Press Release
New survey results indicate that Nigeria has an HIV prevalence of 1.4%
14 March 2019 14 March 2019Expanded data collection and analysis provides better understanding of HIV epidemic in Nigeria
ABUJA/GENEVA, 14 March 2019—Results released today by the Government of Nigeria indicate a national HIV prevalence in Nigeria of 1.4% among adults aged 15–49 years. Previous estimates had indicated a national HIV prevalence of 2.8%. UNAIDS and the National Agency for the Control of AIDS estimate that there are 1.9 million people living with HIV in Nigeria.
Speaking in Abuja, Nigeria, the President of Nigeria, Muhammadu Buhari, welcomed the news that there are fewer people living with HIV in the country than previously estimated and launched the Revised National HIV and AIDS Strategic Framework 2019–2021, which will guide the country’s future response to the epidemic. Nigeria has made good progress in scaling up HIV treatment and prevention services in recent years.
"For the first time, the end of AIDS as a public health threat by 2030 is truly in sight for our country,” said H.E. Muhammadu Buhari, President of Nigeria. “I urge all of us not to relent but to increase the momentum. Let us work collectively and push for the last mile.”
The data from the Nigeria National HIV/AIDS Indicator and Impact Survey (NAIIS) are based a revised and enhanced methodology. The survey provides a clearer understanding of Nigeria’s HIV epidemic and shines a light on progress and the remaining gaps and challenges.
The Executive Director of UNAIDS, Michel Sidibé, welcomed the new estimates and said the improved understanding of the country’s HIV epidemic would allow Nigeria to better reach people living with HIV and people at higher risk of acquiring HIV.
“I commend the Government of Nigeria and its partners for conducting this ambitious survey, which provides us with a much better understanding of the country’s HIV epidemic,” said Mr Sidibé. “While it is fantastic news that there are fewer people living with HIV in Nigeria than previously thought, we must not let down our guard. Let us use the results of this survey to better focus our delivery of HIV prevention, treatment and care services to the people in the greatest need and ensure that Nigeria gets on track to end the AIDS epidemic by 2030.”
While Nigeria’s national HIV prevalence is 1.4% among adults aged 15–49 years, women aged 15–49 years are more than twice as likely to be living with HIV than men (1.9% versus 0.9%.) The difference in HIV prevalence between women and men is greatest among younger adults, with young women aged 20–24 years more than three times as likely to be living with HIV as young men in the same age group. Among children aged 0–14 years, HIV prevalence according to the new data is 0.2%. Significant efforts have been made in recent years to stop new HIV infections among children.
At the national level, viral suppression among people living with HIV aged 15–49 years stands at 42.3% (45.3% among women and 34.5% among men). When people living with HIV are virally suppressed they remain healthy and transmission of the virus is prevented.
The improved understanding of the country’s HIV epidemic will allow for more efficient investments in the response to HIV and more effective planning for the provision of HIV prevention, care and treatment services, including a focus on key populations, such as female sex workers. It will permit the adoption of a population–location approach to deliver services to the people and areas where they are most needed.
The new data differentiate HIV prevalence by state, indicating an epidemic that is having a greater impact in certain areas of the country. The South-South zone of the country has the highest HIV prevalence, at 3.1% among adults aged 15–49 years. HIV prevalence is also high in the North Central zone (2.0%) and in the South East zone (1.9%). HIV prevalence is lower in the South West zone (1.1%), the North East zone (1.1%) and the North West zone (0.6%).
“The Nigeria National HIV/AIDS Indicator and Impact Survey (NAISS) findings provide Nigeria with an accurate national HIV prevalence measure of 1.4%. NAIIS also showed we are able to effectively provide antiretroviral treatment,” said Isaac F. Adewole, Nigeria’s Minister of Health. “Everyone infected with HIV needs to get treatment so they can achieve viral suppression, especially pregnant women. We must ensure pregnant women have access to antenatal services and are tested during every pregnancy. We know we can support HIV-positive mothers, hence ensuring the next generation is free from HIV.”
Nigeria has shown steady progress on increasing access to treatment for people living with HIV, with the adoption of a test and treat policy in 2016. This measure has further accelerated referrals to treatment facilities for people who test positive for the virus. From 2010 to 2017, the country almost tripled the number of people living with HIV having access to antiretroviral therapy, up from 360 000 people in 2010 to more than 1 million people in 2018. However, the new estimates released today indicate that more than half of people living with HIV still do not have suppressed viral loads.
The new data are more accurate as they are based on an expanded surveillance system and a revised and enhanced methodology. In recent years, there has been a significant expansion in the country’s response to HIV. The number of sites providing treatment has more than tripled, the number of sites providing services to prevent mother-to-child transmission of HIV has increased eightfold and the number of HIV counselling and testing sites has increased fourfold. A total of 11.3 million adults were counselled and tested for HIV in 2016, four times as many as in 2012.
“It is important that all people living with HIV get treatment and achieve viral suppression. To halt the epidemic, we need to act now,” said Sani Aliyu, Director-General of the National Agency for the Control of AIDS. “As a government working with our partners, we have what it takes to support people who are HIV-positive, to provide treatment, to protect their families and to help people live long and healthy lives.”
The NAIIS was led by the Government of Nigeria through the Federal Ministry of Health and the National Agency for the Control of AIDS. UNAIDS, the United States President’s Emergency Plan for AIDS Relief and the Global Fund to Fight AIDS, Tuberculosis and Malaria provided support for the work on the survey, which was overseen by the United States Centers for Disease Control and Prevention and implemented by the University of Maryland, Baltimore, with a scope that included all 36 states and the Federal Capital Territory of Nigeria. The survey reached around 220 000 people in about 100 000 households. Fieldwork was conducted between July and December 2018.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Federal Ministry of Health (FMOH)
Federal Ministry of Health is one of the Ministries in the Federal Republic of Nigeria. It is concerned with the formulation and implementation of policies related to health. The Ministry has several departments focusing on different aspects of health care. The Department of Public Health’s National HIV and STI Control Program (NASCP) participated in the conduct of NAIIS and guided its implementation. More information can be found at http://www.health.gov.ng/
National Agency for the Control of AIDS (NACA)
The National Agency for the Control of AIDS was established to coordinate the various activities of HIV/AIDS in the country. The Agency among several functions coordinate and sustain advocacy by all sectors and at all levels for HIV/AIDS/STDs Expanded Responses in Nigeria. The Agency in collaboration with the FMoH guided the implementation of NAIIS. More information can be found at https://naca.gov.ng/ for more information about NACA.
Contact
UNAIDSMichael Hollingdale
tel. +41 22 791 5534 / +41 79 500 21 19
hollingdalem@unaids.org
UNAIDS Media
tel. +41 22 791 42 37
communications@unaids.org
Press centre
Download the printable version (PDF)
Region/country


Press Release
UNAIDS urges action to change discriminatory laws in order to restore dignity and respect and save lives
01 March 2019 01 March 2019On Zero Discrimination Day, UNAIDS calls on countries to examine discriminatory provisions in their laws and policies and make positive changes to ensure equality, inclusion and protection
GENEVA, 1 March 2019—In 2018, a number of countries made landmark decisions to change discriminatory laws and bills. The Supreme Court of India struck down Section 377 of the Penal Code, which criminalized same-sex sexual relations, the Philippines lowered the age of consent for voluntary HIV testing without the need to obtain consent from a parent or guardian to 15 years and Malawi removed provisions from a draft bill that would have criminalized HIV non-disclosure, exposure and transmission.
On Zero Discrimination Day, UNAIDS recalls the equal dignity and worth of every person, as enshrined in the Universal Declaration of Human Rights, and is calling for action to change discriminatory laws and practices, which are a significant barrier for access to health and other services.
“Human rights violations are happening all over the world because of discriminatory laws and practices,” said Michel Sidibé, Executive Director of UNAIDS. “Laws must protect, not cause harm. All countries must carefully examine their laws and policies in order to ensure equality and protection for all people, without exception.”
Raising awareness, mobilizing and taking action are essential. On Zero Discrimination Day, UNAIDS is proposing specific actions that individuals, civil society organizations, parliamentarians and donor organizations can take to change discriminatory laws. These range from being an ally to someone affected by a discriminatory law to joining a nongovernmental organization, tabling amendments to laws and calling for reviews of legislation.
Making a positive change is possible and there are many ways a law can be amended or abolished. These include:
- Reforming or removing laws through parliamentary processes and the votes of parliamentarians.
- Raising awareness among parliamentarians is therefore essential, as was done in the revision of the HIV laws in the Philippines and bills in Malawi.
- In many countries, courts have the power to strike down laws that are discriminatory. This can be done if an individual or organization affected by the law takes legal action and wins the case for change.
- The case of India’s Supreme Court, which removed Section 377 in 2018, was a striking example.
- In some countries, people or politicians can propose law reform through a petition and request a national vote or referendum.
- This is a standard method of legislating in Switzerland.
UNAIDS has identified a range of laws that are discriminatory, impede access to health and social services, restrict freedom of movement and violate human rights.
In 2018:
- At least 20 countries imposed travel restrictions of some form against people living with HIV.
- Around 29 countries reported that they require the consent of a woman’s husband or partner to access sexual and reproductive health services.
- Fifty-nine countries reported mandatory HIV testing for marriage, work or residence permits or for certain groups of people in the law, regulations or policies.
- Seventeen countries criminalized transgender people.
- Forty-five countries had laws that impose the need for parental consent for adolescents and young people below 18 years to access HIV testing services.
- Thirty-three countries imposed the death penalty for drug offences in law.
- Same-sex sexual relations were criminalized in at least 67 countries and territories worldwide.
UNAIDS is actively working with United Nations partners, governments and civil society organizations to change those laws as part of the Global Partnership for Action to Eliminate all Forms of HIV-Related Stigma and Discrimination.
Zero Discrimination Day campaign 2019—act to change laws that discriminate.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaAnne-Claire Guichard
tel. +41 22 791 2321
guicharda@unaids.org
UNAIDS Media
tel. +41 22 791 42 37
communications@unaids.org
Press centre
Download the printable version (PDF)


Press Release
UNAIDS welcomes Shannon Hader as new Deputy Executive Director of Programme
12 February 2019 12 February 2019GENEVA, 12 February 2019—United Nations Secretary-General António Guterres has appointed Shannon Hader as the new Deputy Executive Director of Programme of the Joint United Nations Programme on HIV/AIDS (UNAIDS) and Assistant Secretary-General of the United Nations.
“Shannon is an exceptional leader in AIDS and TB—with extensive experience in improving systems for health,” said UNAIDS Executive Director Michel Sidibé. “From Washington DC to Zimbabwe she understands the epidemic and the response needed at the community, country and global levels—her vision and knowledge will be critical for UNAIDS and to ending AIDS by 2030.”
Dr Hader started her career at the US Centers for Disease Control and Prevention (CDC) and most recently served as the Director of the Division of Global HIV and TB, a key implementing agency of PEPFAR, with more than 2000 staff across 45 countries.
Prior to re-joining the CDC, she held the position of Vice President and Director for the Center for Health Systems and Solutions at the Futures Group (now Pallidum). She led the HIV response in the District of Columbia while serving as Senior Deputy Director, HIV/AIDS, Hepatitis, STD and TB Administration. And in 2017, she was a candidate for US Congress.
A public health physician, Dr Hader’s career has spanned the research, programme and policy spectrum. She is board certified in Internal Medicine, Paediatrics and Infectious Diseases. Dr Hader has worked in the response to HIV in a number of duty stations throughout Africa since she first joined the CDC in 1999.
Dr Hader will assume her new role in March 2019.
“I wish to extend my sincere appreciation to Tim Martineau for serving UNAIDS as Acting Deputy Executive Director of Programme,” said Mr Sidibé.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS Mediatel. +41 22 791 42 37
communications@unaids.org
UNAIDS
Sophie Barton-Knott
tel. +41 22 791 1697 / +4179 514 6896
bartonknotts@unaids.org
Press centre
Download the printable version (PDF)


Press Release
UNAIDS, UNICEF and WHO urge countries in western and central Africa to step up the pace in the response to HIV for children and adolescents
16 January 2019 16 January 2019DAKAR/GENEVA, 16 January 2019—At a high-level meeting in Dakar, Senegal, UNAIDS, the United Nations Children’s Fund (UNICEF) and the World Health Organization (WHO) urged countries in western and central Africa to do more to stop new HIV infections among children and adolescents and increase HIV testing and treatment coverage.
In 2017, around 67 000 children (aged 0–9 years) and 69 000 adolescents (aged 10–19 years) became newly infected with HIV. Two thirds (46 000) of adolescents newly infected with the virus were girls. While progress has been seen in stopping new HIV infections among children in some countries—eleven countries registered a reduction of more than 35% between 2010 and 2017[1]—others, including Nigeria, which has the largest epidemic in the region, experienced no declines at all.
“Countries in western and central Africa have a real opportunity to create a positive change for children and young people,” said Michel Sidibé, Executive Director of UNAIDS. “Underlying issues including a lack of domestic investment, fragile health systems, user fees, gender inequality and widespread stigma and discrimination must urgently be addressed to remove barriers and save lives.”
In western and central Africa, close to 800 000 children and adolescents aged between 0 and 19 years were living with HIV in 2017—the second highest number in the world after eastern and southern Africa.
“The majority of children living with HIV in this region are not receiving care and treatment because they do not know they have HIV as they have not been tested,” said Marie-Pierre Poirier, UNICEF Regional Director for West and Central Africa. “We can reverse that trend by focusing on a family-centered approach to HIV testing and treatment and by rolling out innovative point-of-care technologies that bring testing closer to the primary health facilities and the communities where children live.”
Less than half of all pregnant women living with HIV in the region (47%) had access to antiretroviral medicines to prevent transmission of the virus to their child and only 21% of infants exposed to HIV were tested for the virus within the first two months of life.
We should not lose anymore of Africa’s future to AIDS,” said Matshidiso Moeti, WHO Regional Director for Africa. “Effectively tackling HIV in children and adolescents needs strong and quality health services. By committing to universal health coverage, countries can fast-track progress towards an AIDS-free generation in western and central Africa.”
Although there has been some progress in antiretroviral therapy coverage for children in western and central Africa, which rose from 18% in 2014 to 26% in 2017, the region still has the lowest coverage in the world. Around 52 000 children and adolescents aged between 0 and 19 years died of AIDS-related illnesses in 2017—34 000 of whom died before they reached their fifth birthday.
In the 2016 United Nations General Assembly Political Declaration on Ending AIDS, countries from western and central Africa committed to work towards reducing the number of new HIV infections among children and young adolescents (under 15 years) to 6000 by 2020 and to ensuring access to treatment for 340 000 children and young adolescents (under 15 years) by 2020.
However, pledges to accelerate the HIV response have not been accompanied by a surge in resource mobilization. The total resources needed for an effective response in western and central Africa were 81% greater than the funds available in 2017.
Translating commitments into action requires engagement from political and community leaders, drastically scaling up investments, scaling up innovative technologies such as point-of-care for early infant diagnosis, differentiated service delivery strategies—including family testing and longer prescriptions for antiretroviral medicines—and task-shifting approaches applied to HIV care and treatment services for children across the region.
As part of concerted efforts to step up progress in the region, UNAIDS, UNICEF and WHO called a High-Level Meeting on the Elimination of Mother-to-Child Transmission of HIV and Universal Health Coverage of Paediatric HIV Testing and Treatment in West and Central Africa to unpack the challenges, share best practices and innovative approaches to address the persisting bottlenecks, agree on corrective actions and ensure commitment to action from countries and partners.
Hosted by the Government of Senegal, the meeting is being held in Dakar from 16 to 18 January 2019, bringing together ministers of health, experts, representatives of civil society and partners from across the region as well as high-level representatives of United Nations organizations, the African Union, the Economic Community of West African States and the Economic Community of Central African States.
During the meeting, countries and partners are expected to renew their commitment to the 2015 Dakar Call to Action for Accelerating the Elimination of New HIV Infections in Children and Access to Treatment for Children and Adolescents Living with HIV by 2020.
[1] Benin, Burkina Faso, Burundi, Cameroon, Cape Verde, Côte d’Ivoire, the Democratic Republic of the Congo, Liberia, Senegal, Sierra Leone and Togo.
UNICEF
UNICEF works in some of the world’s toughest places, to reach the world’s most disadvantaged children. Across 190 countries and territories, we work for every child, everywhere, to build a better world for everyone. For more information about UNICEF and its work for children in West and Central Africa, visit https://www.unicef.org/wca/ Follow UNICEF West and Central Africa on Twitter and Facebook
WHO | Africa Region
The WHO Regional Office for Africa is one of WHO’s six regional offices around the world. It serves the WHO African Region, which comprises 47 Member States with the Regional Office in Brazzaville, Republic of Congo. As the lead health authority within the United Nations system, we work with the Member States in the African Region and development partners to improve the health and well-being of people.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNICEFAnne-Isabelle Leclercq Balde
tel. +221 77 740 69 14
aleclercqbalde@unicef.org
WHO
Saya Oka
tel. +242 06 508 1009
okas@who.int
Press centre
Download the printable version (PDF)
Region/country



Press Release
UNAIDS Board calls for immediate implementation of UNAIDS agenda for change
13 December 2018 13 December 2018GENEVA, 13 December 2018—The UNAIDS Programme Coordinating Board (PCB) has called on UNAIDS to fully implement the management response (UNAIDS agenda for change) to address harassment, including sexual harassment, bullying and abuse of power, at the UNAIDS Secretariat which was presented to Board members by the Executive Director of UNAIDS on Tuesday 11 December.
The decision was agreed by the members of the PCB at the conclusion of the 43rd meeting of the PCB in Geneva, Switzerland, today. The PCB agreed to establish a working group to oversee the immediate implementation of the management response and to discuss the report of the Independent Expert Panel in a special PCB meeting before March 2019. The PCB also welcomed the statement of the UNAIDS Secretariat Staff Association and the critical role they played in bringing to the PCB’s attention the issue of harassment at the workplace.
“We don’t have a moment to lose in moving forward our management response. Our actions will make UNAIDS stronger and better,” said Michel Sidibé, Executive Director of UNAIDS. “I look forward to working with all staff to make UNAIDS a model workplace for staff in all their diversity. I look forward to an inclusive, transparent and open dialogue and collaboration with staff in shaping a new UNAIDS.”
The Executive Director of UNAIDS also told the PCB that he wanted to have an orderly transition of leadership at UNAIDS in the final year of his term. He informed the UNAIDS Board that its meeting in June 2019 would be his last Board meeting and he would complete his duties at the end of June 2019.
“I am proud of the successes of UNAIDS. In the past 10 years we have been instrumental in saving millions of lives and averting millions of new HIV infections. The staff of UNAIDS are our greatest asset and I am privileged to serve alongside them,” said Mr Sidibé. “I will work to ensure a smooth transition and pledge to keep my focus on our staff and delivering results for the people we serve."
UNAIDS’ agenda for change will be critical in ensuring that the staff of UNAIDS can continue to build on these successes and deliver maximum results for people living with and affected by HIV. It focuses on five action areas: a staff-centred approach, compliance and standards, leadership and governance, management and capacity. Each area outlines key actions that the UNAIDS Secretariat will undertake.
UNAIDS reiterates its commitment to lead by example in eliminating all forms of harassment, bullying and abuse of power by creating a respectful, transparent and accountable environment that enables all staff to contribute their full potential to deliver for the people they serve.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.


Press Release
UNAIDS puts forward a transformative agenda to create a model working environment at UNAIDS
07 December 2018 07 December 2018UNAIDS outlines five key components for action that build on recommendations made by an Independent Expert Panel
GENEVA, 7 December 2018—UNAIDS is putting in place an agenda for change to transform UNAIDS into a model working environment for all staff that ensures safety and inclusivity and upholds the highest standards of accountability and integrity. The agenda underscores that harassment, including sexual harassment, bullying and abuse of power at any level, will not be tolerated and that perpetrators will be held accountable for their actions.
The agenda is based on a survivor-centred approach to harassment and will ensure that all staff are trained, equipped and supported to call out incivility, sexism, intolerance and other undesirable and unacceptable behaviours. It will strengthen management systems to fit the demands of a decentralized organization and ensure that decision-making happens at the right levels, with full transparency and internal controls for compliance with policies and standards.
The agenda builds on a strong body of work already under way to create a model working environment and draws on recommendations made by an Independent Expert Panel. The Panel was called for by the Executive Director of UNAIDS in February 2018 to provide recommendations on how to further strengthen the implementation of UNAIDS’ zero tolerance policy on sexual harassment.
The Panel’s recommendations and the UNAIDS Secretariat management response and agenda for change will be presented to the UNAIDS Programme Coordinating Board on the first day of its 43rd meeting, which will take place from 11 to 13 December 2018.
“Driven by the AIDS crisis, UNAIDS has been a model for harmonized, system-wide efforts in the United Nations. Today, inspired by the #MeToo movement, we aim to be a model workplace, for the United Nations system and beyond,” said Michel Sidibé, Executive Director of UNAIDS. “Staff are our main asset and they must be able to perform their functions in a safe, enabling and nurturing environment. This transformation will ensure that we can attract the greatest talent and further empower our staff to deliver on our crucial mandate.”
The agenda for change focuses on five key action areas: a staff-centred approach, compliance and standards, leadership and governance, management and capacity. Each area outlines a set of actions the UNAIDS Secretariat will undertake.
In line with its staff-centred approach, the agenda for change will include active bystander training to ensure that everyone in UNAIDS feels equipped and supported to call out incivility, sexism, intolerance and other undesirable and unacceptable behaviours. It will also establish mechanisms for confidential referral to survivor-centred counselling, expand the cadres of Dignity at Work Advisers and provide skills-building for all staff on preventing and addressing harassment, ethics and integrity, knowing your rights at work, diversity and inclusion.
A key component is the recommendation by the Panel to establish an external and independent investigation, disciplinary and redressal system, and UNAIDS will work with stakeholders, including survivors and women’s rights experts, to examine options to take this forward.
UNAIDS will be strengthening its senior management capacity by implementing a new process for the selection of UNAIDS Country Director positions, which it will look to expand to all other senior director-level appointments. This will ensure that UNAIDS’ leaders have the right mix of skills and experience to manage staff as well as skills and experience in technical areas.
In addition, UNAIDS will be implementing a 360-degree feedback mechanism in management appraisals for director-level staff to assess competency in managing people and resources and to detect signals of mismanagement and unacceptable behaviours.
To continue to show greater transparency, UNAIDS will publish reports on disciplinary and accountability actions taken and will proactively refer cases of suspected sexual harassment, harassment, bullying and abuse of power.
UNAIDS will also continue to drive implementation of the United Nations System-Wide Action Plan on Gender Equality and the Empowerment of Women, as well as the updated Gender Action Plan, to build on the significant achievements made in recent years and advance progress towards the new, far-reaching targets set by UNAIDS.
In its findings, the Panel made observations about the UNAIDS leadership and called for change. “I have taken on board the criticisms made by the Panel,” said Mr Sidibé. “In proposing this agenda, I am confident that we can focus on moving forward. I will spend the next 12 months implementing this agenda for change and making the UNAIDS workplace one where everyone feels safe and included.”
The report also highlights that the global AIDS response has witnessed major successes under the leadership of Mr Sidibé. His call for the elimination of new HIV infections among children galvanized action, and significant reductions in new HIV infections have been achieved in all parts of world. Eleven countries have already eliminated new HIV infections among children.
Similarly, during this period, the UNAIDS 90–90–90 targets have propelled a major movement for HIV treatment access. Today, more than 21.7 million people are accessing life-saving antiretroviral therapy, compared to just over 5 million at the end of 2008.
UNAIDS has actively supported civil society engagement, championed human rights, and advocated for the rights of sex workers, gay men and other men who have sex with men, people who inject drugs, transgender men and women, prisoners and migrants to access HIV services. The Executive Director has made the rights of women and girls a priority, including access to sexual and reproductive health services, eliminating gender-based violence and removing harmful gender norms.
Today there is greater freedom of movement for people living with HIV as UNAIDS has worked with countries to remove travel restrictions. HIV and health issues have been kept at the top of political agendas. UNAIDS pioneered the concept of global solidarity and shared responsibility, and today more than half of all resources invested in low- and middle-income countries come from domestic sources. UNAIDS’ agenda for change will be critical in ensuring that UNAIDS staff can continue to contribute to these extraordinary results.
UNAIDS is resolute in its commitment to lead by example in eliminating all forms of harassment, bullying and abuse of power at UNAIDS by creating a respectful, transparent and accountable environment that enables all staff to contribute their full potential to deliver for the people they serve.
Report of the Independent Expert Panel on prevention of and response to harassment, including sexual harassment, bullying and abuse of power at UNAIDS Secretariat:
http://www.unaids.org/en/resources/documents/2018/report-iep
Transforming UNAIDS, an agenda for eliminating all forms of harassment and upholding dignity, accountability and well-being in the workplace. UNAIDS management response to the Independent Expert Panel report
http://www.unaids.org/en/resources/documents/2018/management-response-to-iep-report
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)




Press Release
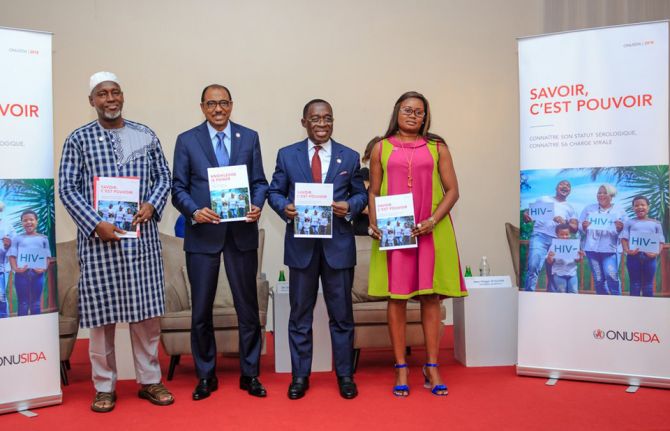
New UNAIDS report shows that 75% of all people living with HIV know their HIV status
22 November 2018 22 November 2018Report also calls for increased efforts to reach the 9.4 million people living with HIV who are not aware that they are living with the virus and the estimated 19.4 million people living with HIV who do not have a suppressed viral load
ABIDJAN/GENEVA, 22 November 2018—A new report from UNAIDS shows that intensified HIV testing and treatment efforts are reaching more people living with HIV. In 2017, three quarters of people living with HIV (75%) knew their HIV status, compared to just two thirds (67%) in 2015, and 21.7 million people living with HIV (59%) had access to antiretroviral therapy, up from 17.2 million in 2015. The report shows, however, that 9.4 million people living with HIV do not know they are living with the virus and urgently need to be linked to HIV testing and treatment services.
The report, Knowledge is power, reveals that although the number of people living with HIV who are virally suppressed has risen by around 10 percentage points in the past three years, reaching 47% in 2017, 19.4 million people living with HIV still do not have a suppressed viral load. To remain healthy and to prevent transmission, the virus needs to be suppressed to undetectable or very low levels through sustained antiretroviral therapy. And to effectively monitor viral load, people living with HIV need access to viral load testing every 12 months.
“Viral load testing is the gold standard in HIV treatment monitoring,” said Michel Sidibé, Executive Director of UNAIDS. “It shows that treatment is working, keeping people alive and well and keeping the virus firmly under control.”
The report outlines that access to viral load testing is mixed. In some parts of the world, getting a viral load test is easy and is fully integrated into a person’s HIV treatment regime, but in other places there may be only one viral load machine for the entire country.
World AIDS Day 2018 message by UNAIDS Executive Director, Michel Sidibé
“Viral load monitoring needs to be as available in Lilongwe as it is in London,” said Mr Sidibé. “HIV testing and viral load testing should be equal and accessible to all people living with HIV, without exception.”
In Côte d’Ivoire, the United States President’s Emergency Plan for AIDS Relief is supporting a national scale-up plan for viral load testing. In just three years, as the number of people on treatment doubled, 10 additional laboratories began viral load testing. Subsequently, viral load testing coverage increased from 14% in 2015 to 66% in 2017 and is projected to reach 75% by the end of 2018.
“This year's UNAIDS theme for World AIDS Day (Live life positively—know your HIV status) reiterates the fact that HIV testing remains the only way to know your status and to adopt a healthy life plan,” said Eugène Aka Aouele, Minister of Health and Public Hygiene, Côte d’Ivoire.
Children and HIV and viral load testing
Viral load testing is particularly important for newborns, as HIV progresses much faster in children—peak mortality for children born with HIV is within two or three months of life. Standard rapid diagnostic testing is ineffective up until 18 months of age, so the only viable test for HIV for very young children is a virological test, which they need to receive within the first four to six weeks of life. However, in 2017, only half (52%) of children exposed to HIV in high-burden countries received a test within the first two months of life.
Important advances are being made. New point-of-care testing technologies—testing that takes place in an environment as close to the person as possible—have been shown to shorten the time it takes to return children’s test results from months to minutes, which is saving lives.
More videos for World AIDS Day
The persistent barriers to knowing one’s status
The report shows that one of the biggest barriers to HIV testing is stigma and discrimination. Studies among women, men, young people and key populations have revealed that fear of being seen accessing HIV services, and if the person is diagnosed, fear that this information will be shared with family, friends, sexual partners or the wider community, was preventing them from accessing HIV services, including HIV testing.
For key populations—gay men and other men who have sex with men, transgender people, sex workers, people who use drugs, people in prisons and other closed settings and migrants—these barriers can affect access to an even greater extent. Stigma and discrimination, from society and health services, can deter members of key populations from accessing health care, while criminal laws can compound that discrimination, increase rates of violence and create additional barriers, including fear of arrest and harassment.
“In Côte d'Ivoire, HIV prevalence among sex workers is 11% and 13% for men who have sex with men and 9.2% for people who inject drugs,” said Pélagie Kouamé, President of the Network of Key Populations in Côte d’Ivoire. “We cannot leave key populations behind. Things must change and evolve so that we can come out from the shadows and no longer live in fear.”
Other barriers include violence or the threat of violence, especially among young women and girls. Parental consent laws and policies are also a barrier, since in some countries young people under the age of 18 years need parental consent to take an HIV test. In addition, services are often too far away and difficult to access or too expensive. There can also be delays or failures in returning HIV test results and delays in treatment initiation. In some countries, people do not seek HIV testing as they feel they are not at risk—in Malawi, one study found that among adolescent girls and young women (aged between 15 years and 24 years), considered to be at higher risk of HIV, more than half (52%) did not consider themselves at risk of HIV and so were unlikely to seek HIV testing services.
Next generation of testing options
The report highlights how providing a variety of testing options and services, such as community-based testing and home-based testing, can help mitigate many of the logistical, structural and social barriers to HIV testing. They offer testing options for people who live far away from health services, do not have the constraints of inconvenient opening hours, which is particularly important for men and people from key populations, and do not come with the stigma and discrimination often perceived in traditional health and HIV services.
“We cannot not wait for people to become sick,” said Imam Harouna Koné, President of the Platform of Networks in the Fight Against AIDS. “We must go out to our communities and offer HIV testing and treatment services.”
The report outlines the importance of taking a five Cs approach: consent, confidentiality, counselling, correct test results and connection/linkage to prevention, care and treatment. “There isn’t a one size fits all approach to HIV testing,” said Mr Sidibé. “There are a number of different strategies needed to reach people at risk of HIV, including innovative approaches such as self-testing, where people may feel more comfortable that their privacy is respected.”
Another important step to take is to integrate HIV testing services within other health services, including maternal and child health services, services for tuberculosis and services for sexually transmitted infections and viral hepatitis. Tuberculosis is the leading cause of death of people living with HIV, accounting for one in three AIDS-related deaths; however, it is estimated that 49% of people living with HIV and tuberculosis are unaware of their coinfection and are therefore not receiving care.
Access to HIV testing is a basic human right, and UNAIDS is calling for a global commitment to remove the barriers preventing people from testing for HIV, which include eliminating HIV-related stigma and discrimination, ensuring confidentiality in HIV testing and treatment services, deploying an optimal mix of HIV testing strategies to reach the populations most in need, integration with other health services, removing policy and legal barriers hindering access to HIV testing and treatment, expanding access to viral load monitoring in low- and middle-income countries and ensuring access to early infant diagnosis for newborns.
The report demonstrates that implementing these measures will hugely advance progress towards ensuring that all people living with and affected by HIV have access to the life-saving services they need.
In 2017 an estimated:
- 36.9 million [31.1 million–43.9 million] people globally were living with HIV
- 21.7 million [19.1 million–22.6 million] people were accessing treatment
- 1.8 million [1.4 million–2.4 million] people became newly infected with HIV
- 940 000 [670 000–1.3 million] people died from AIDS-related illnesses
Download PowerPoint slides from Knowledge is power report
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Knowledge is Power: Thobani's story
Message from WHO
Press centre
Download the printable version (PDF)




Press Release
UNAIDS teams up with Google and Makhulu Media to release virtual reality educational films about HIV testing
20 November 2018 20 November 2018360HIV harnesses the power of immersive technology to reach young people
GENEVA, 19 November 2018—Ahead of World AIDS Day, which takes place on 1 December, UNAIDS is releasing a series of virtual reality (VR) films focused on HIV testing.
Using the latest technology, the films help to demystify HIV testing. With goggles that viewers can wear for a full VR experience, the aim is to reach young people who may want to know their HIV status but are afraid or worried about taking an HIV test.
In the films, a group of talented young people re-enact several scenarios of a young woman’s journey to find out her HIV status. Going from her home to a local health clinic, the films allow viewers to explore different settings through a 360-degree experience.
Makhulu Media, a South African production company produced the VR films, with guidance from UNAIDS and the support of Google, the Desmond Tutu HIV Foundation and the Children's Radio Foundation, which were filmed entirely in the township of Nyanga, near Cape Town, South Africa.
“HIV is preventable and treatable but too few young people know their status,” said UNAIDS Executive Director Michel Sidibé. “We hope that this highly engaging tool will help to dispel fears and show the simple steps that people can take to find out their HIV status.”
At the beginning of the project, Makhulu Media organized workshops with young people to discuss their knowledge of HIV, to share their interactions with health-care providers and to describe their experiences while visiting clinics. The next step involved filming non-actors re-enacting scenes between patients and health-care workers. The short films address the fear of a positive test result and HIV-related stigma.
“We wanted to see if immersive virtual reality films could encourage people to take an HIV test and improve relationships between nurses and young people by helping them to step into each other’s shoes,” said Makhulu Media producer Rowan Pybus.
“The data coming back from the study we have commissioned are very positive,” case study researcher and Makhulu Media co-producer Sydelle Willow Smith said. “The youth and health-care workers involved in the film believe that having the films played to people in waiting rooms in clinics would be very useful.”
The films are being rolled out in clinics, schools and communities in South Africa. Despite progress in reducing AIDS-related deaths and in people accessing treatment, new HIV infections in 2017 in South Africa reached 270 000. This is down from a high of 530 000 in 1998, but the country has 7.2 million people living with HIV—the highest in the world. Google Program Manager Sarah Steele believes that the potential for VT to produce positive social impact is enormous.
“360HIV is a powerful example of how virtual reality can help change the attitudes and beliefs that underlie some of the world’s most urgent social and environmental challenges,” she said.
A quarter of the 37 million people living with HIV in the world do not know their status. The theme of this year’s World AIDS Day campaign is Live Life Positively—Know Your HIV Status and UNAIDS has prepared a range of communications materials that are now available to download from the UNAIDS website at https://knowyourstatus.unaids.org. All the films and trailers can be found here.
Makhulu Media
Founded in 2004, Makhulu is an award-winning film, photography and creative media agency based in Cape Town, South Africa. Passionate about storytelling, environmental issues, community and the arts, they are among the first to have adopted virtual reality filmmaking in the region. Having pioneered a solar-powered mobile cinema, Sunshine Cinema, to screen educational films, Makhulu subsequently branched out into VR.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.





Press Release
Victoria Beckham visits UNAIDS in Geneva to lend her support to the AIDS response ahead of World AIDS Day
23 November 2018 23 November 2018UNAIDS International Goodwill Ambassador urges people to test for HIV and to seek treatment if necessary
GENEVA, 23 November 2018—A little over one week before World AIDS Day, UNAIDS International Goodwill Ambassador Victoria Beckham has visited the organization’s Geneva, Switzerland, headquarters to support calls for people to know their HIV status and to seek treatment for HIV if necessary.
“I am really happy to be in Geneva to support UNAIDS in the run-up to World AIDS Day,” said Ms Beckham during her visit. “We need to make sure that people feel supported to take an HIV test by ending the stigma and discrimination still too often associated with the virus. Today, we have the medicines to keep people healthy and to stop the virus being transmitted. AIDS isn’t over yet, but it can be.”
UNAIDS estimates that there were around 36.9 million people living with HIV worldwide in 2017, with around 21.7 million people accessing life-saving medicines that keep people alive and well and stop the transmission of the virus. However, UNAIDS also estimates that around one in four people worldwide continue to be unaware that they are living with HIV.
During the visit, the UNAIDS Executive Director, Michel Sidibé, met with Ms Beckham to thank her for her support and to discuss the latest developments in the AIDS response.
“We have made a lot of progress in expanding access to treatment, but the number of people who don’t know their HIV status is still far too high,” said Mr Sidibé. “We have to make sure that people have access to testing services and are provided with treatment immediately if they need it. We also have to make sure that people have access to the full range of HIV prevention options to bring down the number of new HIV infections.”
Thanks to antiretroviral therapy, AIDS-related deaths have been reduced by more than 51% since the peak in 2004. In 2017, 940 000 people died from an AIDS-related illness worldwide, compared to 1.9 million in 2004. In 2017, however, there were 1.8 million new HIV infections.
In many regions of the world, women continue to be the worst affected by the epidemic and every week 6600 young women aged 15–24 years become infected with HIV. In sub-Saharan Africa, three in four new infections among adolescents aged 15–19 years are among girls, and young women aged 15–24 years are twice as likely to be living with HIV than men.
In other regions, the epidemic is concentrated among key populations, such as gay men and other men who have sex with men, sex workers, transgender people, people who inject drugs, prisoners and other incarcerated people and migrants.
It is estimated that around 35.4 million people worldwide have died from an AID-related illness since the start of the epidemic.

Press Release
Prime Minister and the First Lady of Lesotho visit UNAIDS
24 October 2018 24 October 2018GENEVA, 24 October 2018—The Prime Minister Thomas Thabane and the First Lady of Lesotho, Maesaiah Thabane, visited UNAIDS headquarters in Geneva, Switzerland, to advocate for the end of AIDS and reduce its impact on young people.
They met the Executive Director of UNAIDS, Michel Sidibé, and UNAIDS staff members.
Around one in six people in Lesotho is living with HIV, one of the highest rates in the world. And more women are affected than men—27.7% of women are living with HIV, while 19.7% of men are. Progress has been made, with AIDS-related deaths declining from 15 000 in 2005 to about 5000 in 2017, but more needs to be done to prevent new HIV infections, notably from mother to child, with the mother-to-child transmission of HIV rate standing at 11.3%.
“We can and we will end new HIV infections among babies,” said Mr Thabane.
The First Lady meanwhile has been a champion of young people. She has shown strong commitment to reducing breast cancer and cervical cancer and pushing access to integrated reproductive health services.
“If we want to reduce and end gender-based violence against women, we must send our girls to school and keep them there,” said Ms Thabane. “We must invest in girls.”
Mr Sidibé expressed his full support, praising Lesotho for making significant progress in its HIV response. He said, “Ending AIDS begins with young people. That means engaging girls and boys and providing them with information through traditional and social media channels.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
