Press Statement
UNAIDS welcomes new guidelines which give an additional HIV prevention option to discordant couples
19 April 2012 19 April 2012New guidelines released for couples HIV testing and counselling and for treatment and prevention in serodiscordant couples
GENEVA, 19 April 2012—New guidelines have been issued encouraging couples to go together for HIV testing in order to know their HIV status. The guidelines, released by the World Health Organization (WHO), also recommend that in couples who are serodiscordant—where one partner is living with HIV and the other not—antiretroviral therapy is offered to the person living with HIV to prevent his or her partner from becoming infected with the virus.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) strongly welcomes the new guidelines and calls on all countries to implement them to reach the targets set in the United Nations 2011 Political Declaration on AIDS.
“Couples can now reap the benefits of antiretroviral therapy, to improve their own health, and to protect their loved ones,” said UNAIDS Executive Director Michel Sidibé. “By encouraging couples to test together, we can provide comprehensive options for HIV prevention and treatment—that they can discuss and manage jointly.”
New evidence now shows that antiretroviral therapy reduces the risk of HIV transmission from a person living with HIV to their sexual partners. WHO recommends that antiretroviral therapy be offered to HIV-positive individuals in discordant relationships even when they do not require it for their own health. The guidance also states that it is possible for couples to stay HIV serodiscordant indefinitely if they consistently practice safer sex using condoms.
“I am excited that with the roll out of these new guidelines, millions of men and women have one additional option to stop new HIV infections,” said Mr Sidibé. “This development begins a new era of HIV prevention dialogue and hope among couples.”
According the new guidelines, “couples who test together and mutually disclose their HIV status are more likely than those testing alone to adopt behaviour to protect their partner. Another potential benefit of couples testing together and sharing their results is that they can support each other, if one or both partners are HIV-positive, to access and adhere to treatment and prevent transmission of HIV to children”.
UNAIDS recommends that HIV testing and counselling should always be confidential and initiation of treatment must always be voluntary and never mandatory or coercive. Couples should have access to the full range of HIV prevention options available including the use of male and female condoms and medical male circumcision. They should also be provided with access to health services such as tuberculosis screening and reproductive health services including family planning with access to effective contraceptives and conception counselling for sero-discordant couples.
According to UNAIDS estimates, around 14 million people are eligible for antiretroviral treatment. At the end of 2011, only 6.6 million people were receiving the life-saving medicines. The guidelines recommend that in situations of limited or inadequate resources, people who require antiretroviral therapy for their own health should always be given priority.

Feature Story
New initiative launched to deliver better, cheaper medicines to Africa
02 April 2012
02 April 2012 02 April 2012
UNAIDS Deputy Executive Director, Programme Dr Paul De Lay speaking at the launch of the East African Community (EAC) Medicines Registration Harmonization Project in Arusha, Tanzania, on 30 March 2012.
The need to ensure that people in Africa have access to essential, high quality, safe and affordable medicines has just received a major boost with the launch of the East African Community (EAC) Medicines Registration Harmonization Project in Arusha, Tanzania, on 30 March 2012.
The project is a high-level alliance bringing together the New Partnership for Africa’s Development (NEPAD), the World Health Organization (WHO), the Bill & Melinda Gates Foundation, the World Bank, the UK Department for International Development (DfID), and the Clinton Health Access Initiative (CHAI). The Arusha launch marks the starting point in the implementation of the broader African Medicines Regulatory Harmonization Programme across the continent.
The partners hope to strengthen regulatory capacity and systems for medicines in Africa, including antiretroviral drugs, so that fewer lives are lost due to drugs which are unsafe and of poor quality or which are largely unavailable or delivered inefficiently. These existing challenges can be attributed to a range of factors which include lack of human and financial resources, insufficient infrastructure, weak medicine legislation and a lengthy drug approval cycle caused by low regulatory capacity and inefficient processes.
“Access to safe, affordable and quality medicines for the treatment of common diseases remain out of reach to many people in the East African region as a whole,” said Dr Richard Sezibera, Secretary General of the East African Community. “The programme we are launching here today will put in place a uniform and standardized medicines regulatory framework for both good health outcomes and economic gains.”
The programme we are launching here today will put in place a uniform and standardized medicines regulatory framework for both good health outcomes and economic gains
Dr Richard Sezibera, Secretary General of the East African Community
The launch was attended by ministers, representatives from regional and pan-African bodies, international organizations and donors. One of the key arguments endorsed by those at the launch was the critical need to produce creative, African sourced solutions, responsive to the particular needs of African people.
This would encourage local production of medicines—such as antiretroviral therapy for people living with HIV—in partnership with other emerging economies like the BRICS group (Brazil, Russia, India, China, South Africa). In addition it would strengthen African control of development investments through more diversified funding sources which would reduce Africa’s dependence on external factors.
At present, Africa is heavily reliant on imported medicines. 80% of the antiretrovirals keeping more than 5 million African people alive come from abroad. In addition, two thirds of all AIDS expenditures in Africa come from external sources.
According to UNAIDS Deputy Executive Director, Programme Dr Paul De Lay, who attended the launch, creating an African Medicines Regulatory Agency would allow faster roll out of drugs, stronger quality assurance, greater public confidence and the enhancement of African ownership of a sustainable AIDS response.

(L to R) UNAIDS Deputy Executive Director, Programme Dr Paul De Lay, Ambassador Dr Richard Sezibera, Secretary General of the East African Community and UNAIDS representative for African Union.
“Regional regulatory agencies will deliver a range of benefits” said Dr De Lay. “Things will be faster, more efficient and fairer,” he added.
UNAIDS believes that such regional initiatives are an essential component of a successful response to HIV. These initiatives will provide a strong platform for advocacy, coordination and regulation to make high quality drugs more widely available across the continent.
An African Medicines Regulatory Agency would additionally allow a more rapid and far reaching response to reports of possible counterfeit or tainted drugs. It will also enhance capacity to test suspect batches of medicine. Such increased regional pharmacovigilance would protect health and save lives. It is hoped that the African Medicines Regulatory Harmonization Programme can help maintain the considerable progress made in the health sector in recent years.
External links
Publications
Related

Feature Story
World TB Day: Children with tuberculosis being failed
23 March 2012
23 March 2012 23 March 2012
Much more needs to be done to prevent tuberculosis (TB) which affects at least half a million of the world’s children every year.
Credit: WHO/Stop TB Partnership
Much more needs to be done to prevent tuberculosis (TB) which affects at least half a million of the world’s children every year, with as many as 70 000 losing their lives. According to WHO and the Stop TB Partnership, most children can be saved from this curable illness with better diagnosis of the condition, greater access to health services and improved coordination of healthcare programmes.
One key area where such coordination is critical is in relation to HIV. Children living with the virus are highly vulnerable to TB infection given their compromised immune systems. HIV-positive people are 20 to 30 times more likely to develop tuberculosis, which is responsible for one quarter of AIDS-related deaths. The situation can be especially dangerous for children as TB is often not routinely considered as a possible diagnosis and can therefore remain undetected.
"We have made progress on TB. Death rates are down 40% overall compared to 1990 and millions of lives have been saved," said Dr Mario Raviglione, Director of the WHO Stop TB Department. "But unfortunately, to a large extent, children have been left behind, and childhood TB remains a hidden epidemic in most countries. It is time to act and address it everywhere," he added.
WHO and the Stop TB Partnership recognize that TB can be hard to diagnose, especially in developing countries where the method used to diagnose it—the analysis of a sputum sample—was developed 130 years ago. Nonetheless, a recent study in Bangladesh found that the detection rate of children with TB more than trebled when workers in 18 community centres received special training on childhood tuberculosis.
Addressing TB in children is relatively inexpensive. According to estimates, tuberculosis prevention for a child costs less than 3 cents a day and treatment around 50 cents a day.
Integrated services needed
Integration of maternal and child health services, HIV care and tuberculosis care to save the lives of children with TB is seen to be an absolute necessity, requiring bold political leadership. This is especially the case if the commitment made by countries in the 2011 Political Declaration on AIDS—to cut in half the number of deaths among people living with HIV by 2015—is to be realised.
We have made progress on TB. Death rates are down 40% overall compared to 1990 and millions of lives have been saved. But unfortunately, to a large extent, children have been left behind, and childhood TB remains a hidden epidemic in most countries. It is time to act and address it everywhere
Dr Mario Raviglione, Director, WHO Stop TB Department
According to WHO/Stop TB Partnership, all HIV-positive pregnant women, babies and children at clinic visits should be checked for signs of tuberculosis and given appropriate treatment if required. When detected in children living with HIV, TB treatment needs to begin immediately and, after two to eight weeks on such treatment, antiretroviral therapy (ART) should be started. Furthermore, relevant personnel need to be trained to check patients for TB risk, signs and symptoms and refer them for TB preventive therapy or TB treatment as needed.
Other recommendations to get to zero TB deaths among children are the inclusion of children and pregnant women among the participants of research studies on new TB diagnostics and drugs; more accurate national estimates of the number of childhood TB cases and deaths; and increased funding for TB diagnostics, drugs and vaccines.
According to Dr Lucica Ditiu, Executive Secretary of the Stop TB Partnership, the key to the ultimate goal of preventing TB deaths in children is for partners to work together to pinpoint those most in need: “Before we can give prevention or treatment we have to find the children at risk of TB, and this will only happen if governments, civil society and the private sector work together."
External links
External links
Partners
Partners
Publications

Feature Story
Libya: UNAIDS works with National Transitional Council to rebuild the country’s AIDS response
17 February 2012
17 February 2012 17 February 2012
As Libya celebrates the first anniversary of the 17 February revolution, UNAIDS together with the governing National Transitional Council are putting the building blocks in place to rejuvenate the country’s AIDS response.
Following UNAIDS Executive Director meeting with the Libyan Deputy Minister of Health Dr. Adel M. Abushoffa, a short term plan has been set up for the country’s AIDS response. The foundation has also been laid to the development of a comprehensive national strategic plan on AIDS.
In collaboration with the World Health Organization (WHO), UNAIDS is providing technical guidance to the government through a resident UNAIDS Senior Advisor to monitor the HIV epidemic, identify priorities and together with the government identify the main gaps in the response.
In the short term, the Libya has requested UNAIDS to support the procurement of antiretroviral (ARV) treatment drugs for around 3000 people living with HIV while working in parallel to reestablish the ARV supply and procurement system that has been interrupted for more than six months. The ARVs are now being shipped to the country.
UNAIDS is taking the lead in coordinating the UN system’s response to AIDS in Libya and new partnerships have been established with key donors such as the European Commission.
Some of the critical long term issues that need attention include strengthening the human resource base of the health system and ensuring that healthcare workers have the skills to provide HIV prevention and treatment services.
The AIDS response also has to focus on reducing stigma and discrimination, especially by health workers, decentralization of HIV-related services, reaching people at increased risk of HIV such as sex workers, men who have sex with men, people who inject drugs as well as migrants and displaced people. The long term national strategic plan will focus on building the capacity of civil society organizations to implement HIV prevention outreach programmes.
As a first step to developing evidence informed AIDS response, Libya, in collaboration with WHO and UNAIDS, is strengthening its HIV surveillance system. Information about the epidemiological situation in Libya is sparse, yet preliminary assessments indicate a severe epidemic among people who inject drugs as well as anecdotal information about HIV infection among sex workers and sex trade on migration routes in the south of the country.
Related

Feature Story
Uniting around a common agenda to address HIV and non-communicable diseases
19 September 2011
19 September 2011 19 September 2011
L to R: South African Minister of Health Dr Aaron Motsoaledi, Director-General of WHO Dr Margaret Chan, UNAIDS Executive Director Michel Sidibé and US Global AIDS Coordinator Eric Goosby participating in the UNAIDS and WHO event on NCDs and HIV.
At the United Nations High Level Meeting on AIDS in New York this June Heads of State and Government adopted a new Political Declaration on HIV/AIDS. As well as setting bold targets to scale-up the response to HIV by 2015, the declaration also included a commitment to work with partners to strengthen advocacy, policy and programmatic links between HIV and non-communicable diseases (NCDs).
On 19 - 20 September 2011, Heads of State and Government are coming together at the United Nations in New York, this time to address the prevention and control of NCDs worldwide. The High Level Meeting of the United Nations General Assembly on the Prevention and Control of NCDs will provide unique opportunity for both NCD and HIV communities to work together for a common agenda.
"Maximizing synergies and integration has been a central focus for UNAIDS for many years,” said UNAIDS Executive Director Michel Sidibé. “AIDS is not an isolated disease, it is a movement which can be leveraged to benefit a wide range of health and development issues.”
AIDS is not an isolated disease, it is a movement which can be leveraged to benefit a wide range of health and development issues
UNAIDS Executive Director Michel Sidibé
Non-communicable diseases––in particular cardiovascular diseases, cancers, chronic respiratory diseases and diabetes––are the biggest cause of death worldwide. More than 36 million people die annually from NCDs (63% of global deaths), including 9 million people who die too young, before the age of 60. More than 90% of these premature deaths from NCDs occur in developing countries and could have largely been prevented.
Experience in addressing HIV and NCDs shows that many of the challenges are common; organizing and delivering adequate prevention services; chronic treatment and care; addressing the social and environmental determinants of these health issues; and reaching people without access to services and people who are disproportionally affected by these diseases both particularly common in regions such as Sab-Saharan Africa.
During the High Level Meeting, UNAIDS and WHO will co-host an event on Tuesday 20 September to unite participants around a common agenda to address NCDs and HIV. The panel will include the Director-General of WHO, the Executive Director of UNAIDS, the South African Minister of Health, the US Global AIDS Coordinator, WHO’s Goodwill Ambassador for Cancer Control and a representative from civil society.
Participants will discuss lessons learnt from experience in responding to NCD’s and HIV. They will also look at finding ways to scale-up action to broadly integrate HIV and NCD programmes, improve health systems and ensure that people most in need have access to services.
External links
External links
Multimedia
Publications
Publications
- Uniting to address NCDs and HIV (event flyer)
Related

Feature Story
Accelerating treatment 2.0 in Asia and the Pacific
28 August 2011
28 August 2011 28 August 2011
While the number of people living with HIV receiving antiretroviral therapy (ART) in Asia and Pacific almost tripled from 280 000 in 2006 to 739 000 in 2009, coverage remains low and only one in three people living with HIV had access to treatment in the region that year.
Early and equitable access to treatment in is hampered by stigma, discrimination and inaccessible service delivery. Limited use of rapid diagnostic and poor linkages between HIV testing and counseling and treatment results to delayed initiation of treatment. Funding constraints also hamper scale up and sustained access to ART.
With 4.9 million people living with HIV in the region, six courtiers account for over 90% of people eligible for treatment: China, India, Indonesia, Myanmar, Thailand and Viet Nam.
Treatment 2.0: the next phase of ART
Against this backdrop, the World Health Organization and UNAIDS Regional Support Team in Asia and Pacific, together with the Asia and Pacific Network of People Living with HIV Working Group (ANP +) organized a session to explore the critical components Treatment 2.0, an innovative approach to treatment on the second day of the 10th International Congress on AIDS in Asia and the Pacific.
In our region some people living with HIV do not even know that HIV can be treated
John Rock, of APN +
Treatment 2.0 is an initiative coordinated by UNAIDS and WHO to catalyze the next phase of HIV treatment scale-up, grounded in public health and human rights. The approach aims at universal and sustained access to antiretroviral treatment through radical simplification and innovation of treatment regimens, renewed commitment and resources, with a focus on decentralized delivery systems and greater involvement of communities.
“Substantial gains can be achieved through appropriate task-shifting and community-based delivery systems,” said Dr Iyanthi Abeyewickreme, HIV/STI Regional Advisor at WHO Regional Office for South-East Asia. “Decentralized services will help to leverage scarce resources to maximize their effect.”
Human and economic benefits
With 60% of people eligible for treatment in the region still not yet able to access it, need for scale up is urgent. There is ample evidence of the human and economic benefits of antiretroviral therapy for people living with HIV. In China, for example, it is estimated that the provision of free antiretroviral therapy has lead to a 64% drop in AIDS related mortality. A resent study has also shown that the risk of transmitting HIV to an uninfected sexual partner can be reduced by as much as 96%, when people living with HIV receive timely and effective antiretroviral therapy.
Funding is critical to take advantage of the multiple new opportunities and developments within the treatment arena.
Dr Bob Verbruggen, of the UNAIDS Regional Support Team in Asia and Pacific
John Rock, of APN +, stated that enhanced understanding of the life-saving benefits of treatment is needed: “In our region some people living with HIV do not even know that HIV can be treated,” he said. He also warned that treatment access needs to be safeguarded against terms of free trade agreements that could affect affordability and availability. Treatment scale up in the region necessitates increased and sustained financing. But experts at the Treatment 2.0 session underlined that investment now will ensure savings in the future.
What is needed to scale up treatment?
Dr Bob Verbruggen, of the UNAIDS Regional Support Team in Asia and Pacific said, “Funding is critical to take advantage of the multiple new opportunities and developments within the treatment arena. Implementing Treatment 2.0 will require important short-term funding from both international and domestic sources, but will yield huge savings in the medium and long term if we simultaneously invest in high-impact HIV prevention programmes.”
The session highlighted country experience and key steps to roll-out Treatment 2.0 in the Asia and Pacific region, and preliminary results from pilot countries such as Viet Nam. Some of the recommendations made included combined action of optimizing drug regimens, advancing point-of-care and other simplified platforms for diagnosis and monitoring, reducing costs, adapting delivery systems, and mobilizing communities and protecting human rights.

Feature Story
Eliminating new paediatric HIV infections and congenital syphilis in Asia-Pacific
27 August 2011
27 August 2011 27 August 2011
Ngan is living with HIV. She gave birth to her son, who was born free of HIV, because Ngan had access to PMTCT services.
Credit: UNAIDS/ Mott
One of the key goals of the global AIDS response is the elimination of new HIV infections among children by 2015 and keeping their mothers alive. In Asia and the Pacific, both Thailand and Cambodia are on track to reach this goal. However, overall, coverage of prevention of mother-to-child transmission is well below global averages, with very wide variations across the region.
During a symposium held on August 27 during The 10th International Congress on AIDS in Asia and the Pacific, experts explored how the 2015 elimination goal could be best achieved in Asia and the Pacific and what immediate concrete steps need to be taken. Organised by the United Nations Children’s Fund (UNICEF), the World Health Organisation (WHO) and UNAIDS, the session also reviewed progress on prevention of mother-to-child transmission of HIV and discussed opportunities and challenges.
The event was intended to build on both the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive, launched in June 2011, and a regional UN Task Force framework on the issue developed in November last year.
Participants heard that improved coverage of prevention of mother to child HIV and congenital syphilis services, better monitoring of mothers living with HIV and their children and greater coordination among health services in the region are critical to eliminating new infections in children.
“To reach the goal of zero new infections among children by 2015, national health services and communities need to work together,” said Steven Kraus, Director of the UNAIDS Regional Support Team for Asia and the Pacific in conjunction with the session. “By coordinating efforts, not only will lives be saved and HIV transmission to children be halted, but national health systems will be strengthened as well.”
To reach the goal of zero new infections among children by 2015, national health services and communities need to work together
Steven Kraus, Director of the UNAIDS Regional Support Team for Asia and the Pacific
Anupama Rao Singh, UNICEF Regional Director for East Asia and the Pacific, maintained that while countries in the region are working to scale up the elimination of new HIV infections among children, there was a need increase monitoring. “A lack of critical monitoring means they do not know how many children born to HIV-positive mothers are free of HIV and how many are infected,” she added, “Improved monitoring, especially through strong data management and follow-up, will go a long way towards our ultimate goal of having zero new infections among the region’s children.”
Without proper follow up systems, many of the children infected with HIV at birth or through breastfeeding will not be treated and about half will die before their second birthday.
The need to scale up antiretroviral (ARV) therapy was also highlighted.
"Technologies like the WHO 2010 recommendations for ARV drugs for treating pregnant women and preventing HIV infections in infants exist and we know what needs to be done. Now we have a new strategy to do it more efficiently and effectively in ways that also contribute to stronger health services,” said WHO South East Asia Regional Director, Dr Samlee Pliangbanchang. “The vision for a new generation free from HIV is within our reach."
By providing high-quality, coordinated, antenatal care and family planning services, identifying and treating pregnant women living with HIV and syphilis, and providing follow-up treatment for children, countries in the region can achieve the goal of zero new infections among their children and keeping their mothers alive, the participants concluded.
External links
External links

Feature Story
Global Fund Round 11: UNAIDS support countries to strengthen proposals
19 August 2011
19 August 2011 19 August 2011
On 15 August 2011, the Global Fund to Fight AIDS, Tuberculosis and Malaria launched its Round 11 call for proposals.
This latest round of funding comes at a critical time in the global AIDS response, as countries work towards scaling up HIV prevention, treatment, care and support programmes and meeting the goals set out in the recently adopted 2011 Political Declaration on HIV/AIDS.
To support countries to submit high quality proposals, WHO and UNAIDS, in consultation with the other UNAIDS Cosponsors, have developed a resource kit for Global Fund Round 11 applications and a “toolkit for key populations proposals and for the targeted pool.”
“To maximize resources, countries need to be smarter in their investment choices,” said Tim Martineau, Director, Programme Effectiveness and Country Support Department, UNAIDS. “This toolkit will help countries make strategic decisions that bring about more results and fill critical gaps in national AIDS responses.”
This toolkit will help countries make strategic decisions that yield tangible impact and fill critical gaps in national AIDS responses
Tim Martineau, Director, Programme Effectiveness and Country Support Department, UNAIDS
The resource kit includes technical briefs and reference materials on key thematic areas to complement the Global Fund guidance for proposal writing. A special Resource Kit web site organized by thematic areas has been created and can be accessed via the UNAIDS and WHO web sites.
“This toolkit will go a long way in addressing some of the uncertainties and questions in developing a winning Global Fund proposal,” said Derek Aryee, Chair of the Country Coordinating Mechanism in Ghana.
Round 11 is an important opportunity for countries to consider key priority areas for inclusion in their proposals, including efforts to eliminate mother to child transmission of HIV, addressing TB-HIV co-infection, strengthening services for key populations and efforts to strengthen community system interventions.
UNAIDS is working closely with countries as they prepare their applications. Support provided includes direct technical assistance and strategic information through UNAIDS country offices, together with peer and expert reviews of proposals prior to the submission deadline of 15 December 2011.
For more information on the Global Fund and Round 11 please visit http://www.theglobalfund.org/en/application.
External links
External links
Related
 Keeping up the momentum in the global AIDS response
Keeping up the momentum in the global AIDS response
24 April 2019
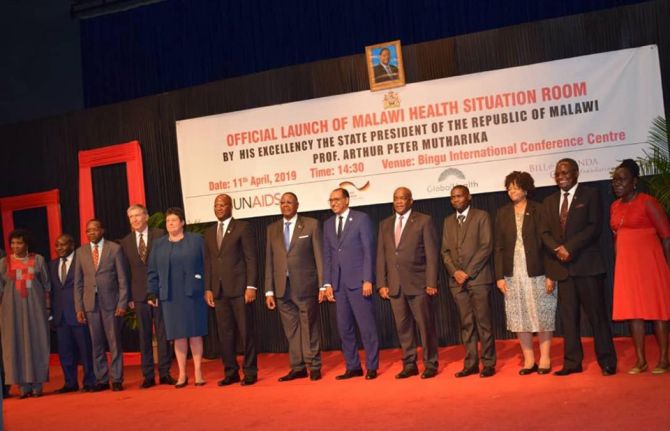 Malawi launches its health situation room
Malawi launches its health situation room
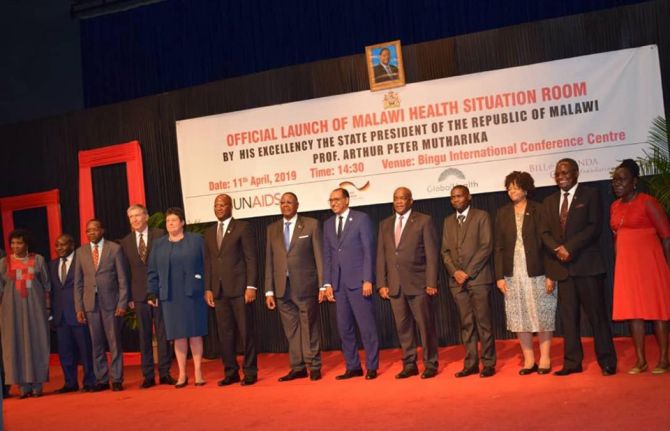
12 April 2019
 Learning lessons on evaluation
Learning lessons on evaluation

02 April 2019

Feature Story
Treatment success in South Sudan: Fozia’s story
15 August 2011
15 August 2011 15 August 2011This is an updated version of a story first published at undp.org

Women living with HIV waiting for treatment at a hospital in Sudan.
Credit: UN/FRED NOY
Weak and unable to walk, Fozia Bullen, from Nagbaka village in South Sudan, had lost all hope when she arrived at Maridi Hospital, one of the few antiretroviral therapy centres in the country for people living with HIV. Her doctor said she had reached a critical stage of illness, with rashes, loss of appetite, and severe weight loss.
After one month of treatment, Ms Bullen was discharged in better health and continues taking medication at home. After four months of treatment, her rashes disappeared, and she put on a significant amount of weight, which enables her to carry out daily work, tend to her gardens, and provide for her family.
She is one of many people living with HIV in South Sudan, which is considered to have a generalized HIV epidemic, with an estimated prevalence of three percent.
Under a five year US$ 27 million project of the Global Fund to Fight AIDS, Tuberculosis and Malaria, thousands of people in South Sudan are now receiving lifesaving HIV treatment. The project brings together a range of partners including the United Nations Development Programme (UNDP), the World Health Organization (WHO), other UN agencies, the Southern Sudan AIDS Commission, the Ministry of Health, and NGOs.
A total of 4,156 people living with HIV have been able to access treatment since 2008. The project, which begun in 2006, has established more than 20 treatment centres across the country.
There has also been significant progress in other key areas. As of March 2011 around 130,000 people had received voluntary HIV counselling and testing and more than 158,000 young people have been educated about the virus. This is a setting where, according to latest research, less than ten percent of people have comprehensive knowledge of effective HIV prevention methods.
The project’s notable successes in addressing the HIV epidemic in South Sudan have been achieved in a country impoverished by more than 20 years of conflict with the north. However, despite celebrations of South Sudan’s independence in July, the world’s newest nation remains fragile, with a lack of basic services and infrastructure, a depressed economy, nascent governance and legal systems, and a returning population of refugees forced to flee the country during the conflict.
To support the AIDS response in South Sudan, UNAIDS is reinforcing its office in Juba in August 2011. Recently appointed UNAIDS country coordinator, Dr Medhin Zewdu is ready to take on her new job.
“National ownership is key to a successful and sustainable AIDS response,” said Dr Zewdu. “I look forward to advancing the agenda on AIDS in discussion with the government, and with the people on the ground including civil society and people living with HIV,” she added.
Related

Press Release
New public health approaches aim to reduce the spread of HIV and save lives of men who have sex with men and transgender people
21 June 2011 21 June 2011GENEVA, 21 June 2011—New public health recommendations from the World Health Organization (WHO) and partners aim to help policymakers and doctors scale up access to treatment and prevention services for HIV and sexually transmitted infections among men who have sex with men and transgender people. These are the first global public health guidelines to focus on these specific population groups.
There has been a recent resurgence of HIV infection among men who have sex with men, particularly in industrialized countries. Data are also emerging of new or newly identified HIV epidemics among men who have sex with men in Africa, Asia, the Caribbean andLatin America. Generally, men who have sex with men are nearly 20 times more likely to be infected with HIV than general populations. HIV infection rates among transgender people range between 8 to 68% depending on the country or region.
One reason for this is the stigma experienced by many men who have sex with men and transgender people. In many countries, criminalization of same sex relationships drives such relationships underground, making people afraid to seek HIV prevention and treatment services. WHO and its partners advise more inclusive approaches and suggest some practical ways to improve their access to HIV prevention, diagnosis, treatment and care services.
"We cannot imagine fully reversing the global spread of HIV without addressing the specific HIV needs of these key populations," said Dr Gottfried Hirnschall, WHO's Director of HIV/AIDS Department. "We are issuing these guidelines to help countries and communities scale up the services needed to reduce new infections and save lives."
"Men who have sex with men and transgender people everywhere face huge difficulties in accessing HIV services," said George Ayala, Executive Director of the Global Forum MSM & HIV (MSMGF), a key partner in producing the recommendations. "The guidelines both present evidence for effective prevention interventions for these populations and provide recommendations to help ensure that pervasive barriers like stigma and criminalization no longer stand in the way of life-saving services.”
The new guidelines "Prevention and treatment of HIV and other sexually transmitted infections (STIs) among men who have sex with men and transgender people: Recommendations for a public health approach" provide 21 recommendations for actions to be taken by multiple stakeholders, in close cooperation with men who have sex with men and transgender people, including:
- For national policy-makers: To develop anti-discrimination laws and measures to protect human rights, and to establish more inclusive services for men who have sex with men and transgender people based on their right to health
- For health service providers: To offer HIV testing and counselling followed by treatment for patients with CD4 count 350 or below as recommended in the WHO 2010 HIV treatment guidelines
- For communities: To scale up behavioural interventions for the prevention of HIV and STIs among men who have sex with men and transgender people
- For affected individuals: Practice consistent condom use over choosing partners based on HIV infection status (sero-sorting)
"Urgent action is needed to ensure that the basic human rights of people most at risk of HIV infection are respected and that they have the information and tools to protect themselves against HIV and gain access to antiretroviral therapy if needed,” said Mariângela Simào, Chief, Prevention, Vulnerability and Rights, UNAIDS.
The WHO guidelines have been developed over the past year through global consultations involving public health officials, scientists, and representatives from donor organizations, civil society and health service providers. The new guidelines can be found at: http://www.who.int/hiv/pub/guidelines/msm_guidelines2011/en/ .
Contact
WHOTunga Namjilsuren
tel. + 41 22 791 1073/ +41 79 203 3176
namjilsurent@who.int
UNAIDS Geneva
Sophie Barton-Knott
tel. +41 22 791 1697
bartonknotts@unaids.org
Global Forum on MSM & HIV
Jack Beck
tel. +1 510 271 1956
jbeck@msmgf.org
Publications
Publications
Press centre
Download the printable version (PDF)