Press Statement
World AIDS Day 2020 message from UNAIDS Executive Director Winnie Byanyima
01 December 2020 01 December 2020World AIDS Day 2020 will be like no other.
COVID-19 is threatening the progress that the world has made in health and development over the past 20 years, including the gains we have made against HIV.
Like all epidemics, it is widening the inequalities that already existed.
Gender inequality, racial inequality, social and economic inequalities. We are becoming a more unequal world.
I am proud that over the past year the HIV movement has mobilized to defend our progress, to protect people living with HIV and other vulnerable groups and to push the coronavirus back.
Whether campaigning for multimonth dispensing of HIV treatment, organizing home deliveries of medicines or providing financial assistance, food and shelter to at-risk groups, HIV activists and affected communities have again shown they are the mainstay of the HIV response. I salute you!
It is the strength within communities, inspired by a shared responsibility to each other, that has contributed in great part to our victories over HIV.
Today, we need that strength more than ever to beat the colliding epidemics of HIV and COVID-19.
Friends, in responding to COVID-19, the world cannot make the same mistakes it made in the fight against HIV, when millions in developing countries died waiting for treatment.
Even today, more than 12 million people are still waiting to get on HIV treatment and 1.7 million people became infected with HIV in 2019 because they could not access essential services.
That is why UNAIDS has been a leading advocate for a People’s Vaccine against the coronavirus.
Global problems need global solidarity.
As the first COVID-19 vaccine candidates have proven effective and safe, there is hope that more will follow, but there are serious threats to ensuring equitable access. We are calling on companies to openly share their technology and know-how and to wave their intellectual property rights so that the world can produce the successful vaccines at the huge scale and speed required to protect everyone and so that we can get the global economy back on track.
Our goal of ending the AIDS epidemic was already off track before COVID-19. We must put people first to get the AIDS response back on track. We must end the social injustices that put people at risk of contracting HIV. And we must fight for the right to health. There is no excuse for governments to not invest fully for universal access to health. Barriers such as up-front user fees that lock people out of health must come down.
Women and girls must have their human rights fully respected, and the criminalization and marginalization of gay men, transgender people, sex workers and people who use drugs must stop.
As we approach the end of 2020, the world is in a dangerous place and the months ahead will not be easy.
Only global solidarity and shared responsibility will help us beat the coronavirus, end the AIDS epidemic and guarantee the right to health for all.
Thank you.
Winnie Byanyima
Executive Director of UNAIDS
Under-Secretary-General of the United Nations
World AIDS Day 2020 playlist
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.





Feature Story
Next global AIDS strategy: be part of making history
09 July 2020
09 July 2020 09 July 2020Opening a session at the 2020 International AIDS Conference on UNAIDS’ next global AIDS strategy, UNAIDS Executive Director Winnie Byanyima presented a bold plan to put the global response to HIV back on track.
“Earlier this week, I raised the alarm that the world will miss the global HIV targets by 2020. The new UNAIDS strategy will be the road map to get the global response back on track to end the AIDS epidemic by 2030,” said Ms Byanyima. “The next UNAIDS strategy must address head-on the areas where we are still lagging, like combination prevention and human rights of key populations, and address the multiple vulnerabilities of adolescent girls and young women in sub-Saharan Africa.”
The session was an opportunity for the participants to engage in a discussion with UNAIDS on the key principles and issues that should underpin the next UNAIDS global AIDS strategy.
Deborah Birx, the United States Global AIDS Coordinator and White House Coronavirus Response Coordinator, stressed the need to “bring data, communities and governments together to address the issues people are confronted with every day.”
The participants agreed on the need for the strategy to address the core vulnerabilities that put people at risk, including harmful traditional gender norms, accessing livelihoods and education and reducing the exclusion and marginalization of key populations.
“Health is not only about health. Health is also about social justice. It's not enough to provide sex workers with condoms without addressing all the factors that prevent them from using them,” said Rico Gustav, Executive Director of the Global Network of People Living with HIV and Chair of the Global Fund Strategy Committee.
To close the gaps, there is a need to apply evidence to design programmes that adapt to the different epidemics and contexts. “We do have the tools to make an impact, but we need to move that to local level. We need to look at more customized solutions,” said Quarraisha Abdool Karim, from the Centre for the AIDS Programme of Research in South Africa.
There was a clear call for communities to be at the centre of the response in order to drive change. At the same time, the participants flagged the need to invest in communities to empower them to claim their leadership role, to hold everyone accountable, to help design and deliver people-centred, rights-based responses to HIV, tuberculosis and COVID-19 and to reach the hard to reach populations.
“How can we have people power when we don’t even have funding,” said Lucy Wanjiku, from the Kenya Positive Young Women Voices.
“Communities must be at the centre of the response. This means being funded, being part of decision-making and opening civic spaces for them to hold us all accountable,” added Ludo Bok, Manager of the Health and Development Group, United Nations Development Programme.
The speakers called for a serious reflection on what must be changed and a collective commitment to change the way we respond to HIV. The participants agreed on the need to focus the conversation on health as a basic right, on health as a social construct. HIV treatment and prevention cannot be delivered if there remain gaps to accessing knowledge, education, health care, harm reduction, sexual and reproductive health, secured livelihoods, economic opportunities, protection from violence and access to justice.
“I feel a renewed sense of urgency. We cannot continue to do the same things and expect a different outcome,” said Ms Byanyima. “People are expecting this strategy to set an urgent new direction for the global AIDS response—for the UNAIDS Joint Programme, for ending AIDS in every country and in every community.”
Related

Press Release
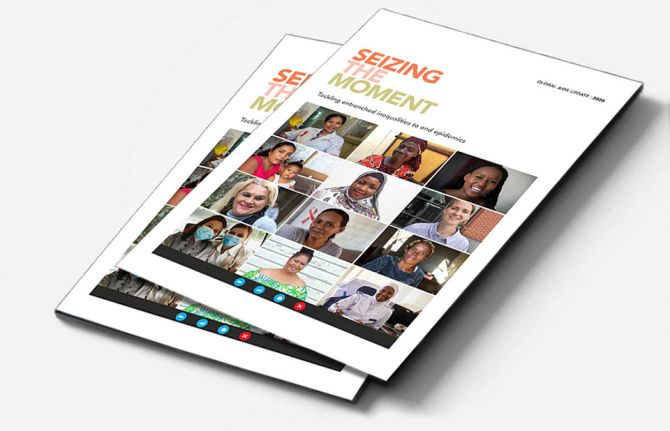
UNAIDS report on the global AIDS epidemic shows that 2020 targets will not be met because of deeply unequal success; COVID-19 risks blowing HIV progress way off course
06 July 2020 06 July 2020Missed targets have resulted in 3.5 million more HIV infections and 820 000 more AIDS-related deaths since 2015 than if the world was on track to meet the 2020 targets. In addition, the response could be set back further, by 10 years or more, if the COVID-19 pandemic results in severe disruptions to HIV services.
GENEVA, 6 July 2020—A new report by UNAIDS shows remarkable, but highly unequal, progress, notably in expanding access to antiretroviral therapy. Because the achievements have not been shared equally within and between countries, the global HIV targets set for 2020 will not be reached. The report, Seizing the moment, warns that even the gains made could be lost and progress further stalled if we fail to act. It highlights just how urgent it is for countries to double down and act with greater urgency to reach the millions still left behind.
“Every day in the next decade decisive action is needed to get the world back on track to end the AIDS epidemic by 2030,” said Winnie Byanyima, the Executive Director of UNAIDS. “Millions of lives have been saved, particularly the lives of women in Africa. The progress made by many needs to be shared by all communities in all countries. Stigma and discrimination and widespread inequalities are major barriers to ending AIDS. Countries need to listen to the evidence and step up to their human rights responsibilities.”
Fourteen countries have achieved the 90–90–90 HIV treatment targets (90% of people living with HIV know their HIV status, of whom 90% are on antiretroviral treatment and of whom 90% are virally supressed), including Eswatini, which has one of the highest HIV prevalence rates in the world, at 27% in 2019, and which has now surpassed the targets to achieve 95–95–95.
Millions of lives and new infections have been saved by the scale-up of antiretroviral therapy. However, 690 000 people died of AIDS-related illnesses last year and 12.6 million of the 38 million people living with HIV were not accessing the life-saving treatment.
“We cannot rest on our successes, nor be discouraged by setbacks. We must ensure that no one is left behind. We must close the gaps. We are aiming for 100–100–100,” said Ambrose Dlamini, the Prime Minister of Eswatini.
The world is far behind in preventing new HIV infections. Some 1.7 million people were newly infected with the virus, more than three times the global target. There has been progress in eastern and southern Africa, where new HIV infections have reduced by 38% since 2010. This is in stark contrast to eastern Europe and central Asia, which has seen a staggering 72% rise in new HIV infections since 2010. New HIV infections have also risen in the Middle East and North Africa, by 22%, and by 21% in Latin America.
Seizing the moment shows unequal progress, with too many vulnerable people and populations left behind. Around 62% of new HIV infections occurred among key populations and their sexual partners, including gay men and other men who have sex with men, sex workers, people who inject drugs and people in prison, despite them constituting a very small proportion of the general population.
Stigma and discrimination, together with other social inequalities and exclusion, are proving to be key barriers. Marginalized populations who fear judgement, violence or arrest struggle to access sexual and reproductive health services, especially those related to contraception and HIV prevention. Stigma against people living with HIV is still commonplace. At least 82 countries criminalize some form of HIV transmission, exposure or non-disclosure, sex work is criminalized in at least 103 countries and at least 108 countries criminalize the consumption or possession of drugs for personal use.
Women and girls in sub-Saharan Africa continue to be the most affected and accounted for 59% of all new HIV infections in the region in 2019, with 4500 adolescent girls and young women between 15 and 24 years old becoming infected with HIV every week. Young women accounted for 24% of new HIV infections in 2019, despite making up only 10% of the population in sub-Saharan Africa.
However, where HIV services are comprehensively provided, HIV transmission levels are reduced significantly. In Eswatini, Lesotho and South Africa, a high coverage of combination prevention options, including social and economic support for young women and high levels of treatment coverage and viral suppression for previously unreached populations, have narrowed inequality gaps and driven down the incidence of new HIV infections.
The COVID-19 pandemic has seriously impacted the AIDS response and could disrupt it more. A six-month complete disruption in HIV treatment could cause more than 500 000 additional deaths in sub-Saharan Africa over the next year (2020–2021), bringing the region back to 2008 AIDS mortality levels. Even a 20% disruption could cause an additional 110 000 deaths.
“Those of us who survived HIV and fought for life and access to treatment and care cannot afford losing the gains that took so much effort to win. In some Latin American countries we are seeing how HIV resources, medicines, medical staff and equipment are being moved to the fight against COVID-19,” said Gracia Violeta Ross, President of the Bolivian Network of People Living with HIV. “Some good lessons and practices of the HIV response, such as meaningful participation and accountability, are being ignored. We will not allow HIV to be left behind.”
To fight the colliding epidemics of HIV and COVID-19, UNAIDS and partners are leading a global call for a People’s Vaccine for COVID-19, which has been signed by more than 150 world leaders and experts demanding that all vaccines, treatments and tests be patent-free, mass produced and distributed fairly and free for all.
UNAIDS is also urging countries to increase investments in both diseases. In 2019, funding for HIV fell by 7% from 2017, to US$ 18.6 billion. This setback means that funding is 30% short of the US$ 26.2 billion needed to effectively respond to HIV in 2020.
“We cannot have poor countries at the back of the queue. It should not depend on the money in your pocket or the colour of your skin to be protected against these deadly viruses,” said Ms Byanyima. “We cannot take money from one disease to treat another. Both HIV and COVID-19 must be fully funded if we are to avoid massive loss of life.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 22 791 1697 / +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)


Press Release
UNAIDS Executive Director sets out HIV/COVID-19 landscape at opening of PCB meeting
24 June 2020 24 June 2020GENEVA, 24 June 2020—The 46th meeting of the UNAIDS Programme Coordinating Board commenced on 23 June 2020. Held for the first time as a virtual meeting, as a result of the COVID-19 pandemic, the meeting will see three days of discussion and reflection on the HIV response, the interconnectedness between the twin pandemics of HIV and COVID-19 and the work of the Secretariat and the Joint Programme.
In her opening address to the PCB meeting, Winnie Byanyima, the Executive Director of UNAIDS, presented an overview of the HIV/COVID-19 landscape in mid-2020 and told the online audience that the HIV epidemic is still urgent, unfinished business.
“Even before COVID-19 we were not on track to meet our targets for 2020. Now the COVID-19 crisis risks blowing us way off course,” warned Ms Byanyima. “As a Joint Programme, we must address the deeper challenges to recover from this crisis to beat both pandemics and foster safe, equitable and resilient societies,” she added.
Ms Byanyima urged countries to learn the lessons from a history of unequal access to HIV services and apply them to the fight against COVID-19. She noted that millions of people died from AIDS-related illnesses while there were medicines available that could have saved their lives—leaving access to medicines to pharmaceutical companies resulted in prices that were too high for people in developing countries.
In the same vein, Ms Byanyima reiterated her call for a People’s Vaccine for COVID-19, with an international agreement that any vaccines and treatments discovered for COVID-19 be made available to all countries. “Developing countries must not be priced out,” she said.
The Executive Director also spoke about the increasing relevance of UNAIDS during a new pandemic and how it has a unique combination of experience and expertise that can help ensure that investments in the COVID-19 response reflect the vital lessons learned from the HIV response.
Supporting HIV treatment and prevention, working on the front line with communities, supporting human rights and gender equality and campaigning against stigma and discrimination—these are part of UNAIDS’ core mandate, she told the meeting. UNAIDS will continue to deliver on that mandate and reach the people who are left the furthest behind, but will also move the global policy needle and tackle the inequalities that place people at greater risk of both HIV and COVID-19, she said.
Turning to the next global UNAIDS strategy, Ms Byanyima committed that the critical new strategy, designed to shape an improved HIV response, will reflect the widest possible input and engagement—from the PCB, its constituencies and the global AIDS community. She suggested that an ambitious draft strategy be presented to the 47th meeting of the PCB in December 2020, with a final version to be reviewed and adopted by the PCB in March 2021.
Ms Byanyima updated the PCB on the internal transformation of UNAIDS, outlining how she will bring feminist leadership principles to help change the culture of the organization. A series of other steps—including a revised performance management system and an independent ethics function—that will ensure that the transformation continues to be on course were announced.
Ms Byanyima ended her address with a reminder of the huge returns that are seen from investing in UNAIDS. She said that it is vital that UNAIDS, along with funding sources such as the Global Fund to Fight AIDS, Tuberculosis and Malaria and the United States President’s Emergency Plan for AIDS Relief, be fully funded.
“As COVID-19 has shown, investments in HIV principles, approaches and infrastructure and expertise extend far beyond the AIDS response,” she said.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)
Documents
Report of the UNAIDS Executive Director — Opening of the 46th meeting of the UNAIDS Programme Coordinating Board
23 June 2020
2020 is a critical year for our Joint Programme as we collectively define the path to getting back on track to ending the AIDS epidemic by 2030. Our revised timelines for adoption of the next strategy are highly ambitious. We need the full support of all the tremendously dedicated people in UNAIDS-within our staff, our board and all our stakeholders to make this happen.

Opinion
Health: providing free health for all, everywhere
20 May 2020
20 May 2020 20 May 2020By Winnie Byanyima, UNAIDS Executive Director — First published in World Economic Forum's Insight Report (May 2020)
Recognizing the public-health catastrophe
As we have seen in wealthier countries, economic and social determinants of ill-health are strong predictors of the likelihood of dying from COVID-19. The greatest risk will be for poor people in poor countries who have a much higher burden of existing illness, and of whom hundreds of millions are malnourished or immunocompromised. For the quarter of the world’s urban population who live in slums, and for many refugees and displaced people, it is not possible to socially distance or to constantly wash hands.
Half the world’s people cannot access essential healthcare even in normal times. While Italy has one doctor for every 243 people, Zambia has one doctor for every 10,000 people. Mali has three ventilators per million people. Average health spending in low-income countries is only $41 per person a year, 70 times less than high-income countries.
The pressure the pandemic will place on health facilities will not only affect people with COVID-19 – anyone needing any care will be impacted. This has previously been the case. During the Ebola epidemic in Sierra Leone there was a 34% increase in maternal mortality and a 24% increase in the stillbirth rate, as fewer women were able to access both pre- and post-natal care.
The International Labour Organization predicts 5 million-25 million jobs will be eradicated, and $860 billion-$3.4 trillion will be lost in labour income. Mass impoverishment will make treatment inaccessible for even more people. Already every year 1 billion people are blocked from healthcare by user fees. This exclusion from vital care won’t only hurt those directly affected – it will put everyone at risk, as a virus can’t be contained if people can’t afford testing or treatment.
Lockdowns without compensation are, at their crudest, forcing millions to choose between danger and hunger. As in many developing country cities, over three quarters of workers are in the informal sector, earning on a daily basis, many who stay in will not have enough to eat and so large numbers will ignore lockdown rules and risk catching the coronavirus.
As we have seen in the AIDS response, governments struggling to contain the crisis may seek scapegoats – migrants, minorities, the socially excluded – making it even harder to reach, test and treat to contain the virus. Donor countries may turn inwards, feeling they can’t afford to help others and, as the presence of COVID-19 anywhere is a threat to people everywhere, this will not only hurt developing countries, it will also exacerbate the challenge in donor countries too.
And yet, amid the pain and fear, the crisis also generates an opportunity for bold, principled, collaborative leadership to change the course of the pandemic and of society.
Seizing the public-health opportunity
Contrary to conventional wisdom that responding to a crisis takes away the capability needed for major health reforms, the biggest steps forward in health have usually happened in response to a major crisis – think of the post-Second World War health systems across Europe and in Japan, or how AIDS and the financial crisis led to universal healthcare in Thailand. Now, in this crisis, leaders across the world have an opportunity to build the health systems that were always needed and which now cannot be delayed any longer.
Universal healthcare
This pandemic has shown that it is in everyone’s interest that people who feel unwell should not check their pocket before they seek help. As the struggle to control an aggressive coronavirus rages on, the case to end user fees in health immediately has become overwhelming.
Free healthcare is not only vital for tackling pandemics: when the Democratic Republic of the Congo instituted free healthcare in 2018 to fight Ebola, healthcare utilization improved across the board with a more than doubling of visits for pneumonia and diarrhoea, and a 20%-50% increase in women giving birth at a clinic – gains that were lost once free healthcare was removed. Free healthcare will also prevent the tragedy of 100 million people driven into extreme poverty by the cost of healthcare every year.
Because COVID-19 has no vaccine yet, all countries will need to be able to limit and hold it. The inevitability of future pandemics makes permanent the need for strong universal health systems in every country in the world.
Publicly funded, cutting-edge medicines and healthcare must be delivered to everyone no matter where they live. To enable universal access, governments must integrate community-led services into public systems. This crisis has also highlighted how our health requires that the health workers who protect and look after us are themselves protected and looked after.
Given the interconnectedness between health and livelihoods, all countries will also need to strengthen social safety nets to enhance resilience. COVID-19 has reminded the world that we need active, accountable, responsible governments to regulate markets, reduce inequality and deliver essential public services. Government is back.
Financing our health
Many developing countries were already facing debt stress leading to cuts in public healthcare. In recognition that worldwide universal healthcare is a global public good, lender governments, international financial institutions and private financial actors need to both extend and go beyond the temporary debt suspensions that have been announced recently. The proposal by the Jubilee Debt Campaign and hundreds of other civil society organizations sets out the kind of ambition required.
Bilateral donors and international financial institutions, including the World Bank, should also offer grants – not loans – to address the social and economic impacts of the pandemic on the poor and most vulnerable groups, including informal sector workers and marginalized populations. Support to developing countries’ ongoing health system costs needs to be stepped up. It would cost approximately $159 billion to double the public health spending of the world’s 85 poorest countries, home to 3.7 billion people. This is less than 8% of the latest US fiscal stimulus alone. It is great to see donor countries using the inspiring and bold language of a new Marshall Plan – but currently pledged contributions are insufficient.
Business leadership
A new kind of leadership is needed from business too; one that recognizes its dependence on healthy societies and on a proper balance between market and state. As President Macron has noted, this pandemic “reveals that some goods and services must be placed outside the rules of the market”. ’The past decade has seen a rapid increase in the commercialization and financialization of healthcare systems across the globe. This must end.
As a group of 175 multimillionaires noted in a public letter released at the World Economic Forum Annual Meeting 2020 in Davos, it is time for “members of the most privileged class of human beings ever to walk the earth” to back “higher and fairer taxes on millionaires and billionaires and prevent individual and corporate tax avoidance and evasion.” Responsible business leaders should support corporate tax reform, nationally and globally, that will necessarily include higher rates, removing exemptions, and closing down tax havens and other tax loopholes.
Despite the lessons from AIDS, monetizing of intellectual property has brought a system of huge private monopolies, insufficient research into key diseases and prices that a majority of the world can’t afford. Countries will need to use all available flexibility to ensure availability of essential health treatments for all their people, and secure new rules that prioritize collective health over private profit. There needs to be prior international agreement that any vaccines and treatments discovered for COVID-19 will be made available to all countries. The proposal by Costa Rica for a “global patent pool” would allow all technologies designed for the detection, prevention, control and treatment of COVID-19 to be openly available, making it impossible for any one company or country to monopolize them. Developing countries must not be priced out or left standing at the back of the pharma queue.
Leadership is needed in reshaping global cooperation: the COVID-19 crisis has exposed our multilateral system as unequal, outdated and unable to respond to today’s challenges. We will face even greater threats than this pandemic, which only an inclusive and just multilateralism will enable us to overcome.
All of us need all of us
The COVID-19 pandemic is simultaneously a crisis worsening existing inequalities and an opportunity that makes those inequalities visible.
The HIV response proves that only a rights-based approach rooted in valuing everybody equally can enable societies to overcome the existential threat of pandemics. Universal healthcare is not a gift from the haves to the have-nots but a right for all and a shared investment in our common safety and wellbeing.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Related


Opinion
We must act together to beat COVID-19 in Africa
03 May 2020
03 May 2020 03 May 2020The COVID-19 outbreak has been placing unprecedented strains on sophisticated health systems in Europe and Asia, with overstretched medical staff struggling to treat their patients and intensive care facilities overwhelmed in rich countries. With cases rising in Africa, concerns are increasing on the impact on fragile health systems there. This crisis is already exposing glaring inequalities between the rich and the poor in the developed world, and it is about to reflect even greater inequalities between the North and the South.
This health crisis, like others, is hitting the poorest and the most vulnerable the hardest, especially in Africa. What does social distancing mean in Africa’s congested townships, its packed markets and buses. How will people wash their hands several times a day to protect themselves from the virus without having access to water and basic sanitation? And what does that mean for women and girls who bear the daily burden of hauling water from rivers and wells for their households? How will a mother choose between going to work to put food on the table or staying at home with a cough or a fever? How do we tell informal workers, taxi drivers and all those who operate in the platform economy and live hand-to-mouth not to go to work?
We need to act now! There are four things we must do urgently: scale up testing and isolate infected people and communities, invest in health and protect our healthcare workers, focus on the community to ensure that the community response is strong, and have a constant supply chain.
The Africa Centre for Disease Control and Prevention estimates that 10 million testing kits will be necessary to respond to COVID-19 effectively over the next three months. Hundreds of millions of personal protective items such as face masks, protective gowns and gloves will also be needed. At a time when there is a global demand for these medical supplies, Africa must not be left behind. As we have seen in other countries, the best way to reduce infections and deaths is to test, treat and isolate infected people and communities to contain the virus. So, the supply of testing equipment and access to testing must be the priority.
A lack of investment in Africa’s social infrastructure, including in its health systems, mounting debt and massive corporate tax dodging has left the continent ill-prepared to face this coming emergency. Without publicly provided health care, people are left exposed to disease. User fees for accessing health services deny ordinary people their right to health. This is the time to abolish them. Rich countries are rightly pumping billions of dollars into their own economies and social security systems to keep people and businesses afloat, but will there be massive coordinated international financial support for the developing countries to fight Covid-19? We are in this together. Nothing but a global response will defeat this aggressive virus.
In responding to the HIV epidemic, community-led services have been core to our most important advances in preventing new infections and getting people on treatment. In the response to COVID-19, communities will no doubt step into the breach and public health authorities must engage with them now and build trust for the upcoming battle. We will not win without communities. It is communities who will design and implement their own context specific prevention measures, in markets, in buses, at funerals. As we have seen in the AIDS response, it will most often be women who will lead the charge in terms of caring for the sick and making sure that their children and communities are as safe as possible. We must ensure that resources flow to them so that they can carry on their important work, that they are fairly compensated and that their families are financially secure.
And the response must respect the human rights of the most vulnerable. There have already been incidents all over the world where individuals or communities are being blamed for the virus. This must stop. It’s wrong and counter-productive for the wider public good. Let us learn the lessons of the AIDS response and know that stigma and discrimination will hold us back in getting to grips with this pandemic.
In addition, to make sure that medicines continue to reach people in need, we must ensure the security of the global supply chain in this period. UNAIDS is working closely with all its partners to make sure that essential medicines and medical supplies continue to get to where they are most needed. We will continue to do so.
I wish we were in a different place. That everyone had the right to health and that we were in a stronger position to face this new challenge. That debate will continue and my voice will stay strong. For now, we must do the best we can for our communities.
Let us help and support each other during this time – we are all in this together and we will beat this virus through solidarity, compassion, and kindness.
Winnie Byanyima, UNAIDS Executive Director
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.