UNAIDS warns that countries urgently need to take proven, tailored, evidence-informed primary HIV prevention programmes to scale in addition to increasing access to treatment.
AMSTERDAM/GENEVA, 24 July 2018—UNAIDS is urging countries to take bold action to address the HIV prevention crisis. Around 1.8 million people became newly infected with HIV in 2017 and around 50 countries experienced a rise in new HIV infections as HIV prevention services are not being provided on an adequate scale or with sufficient intensity.
“Health is a human rights imperative and we are deeply concerned about the lack of political commitment and the failure to invest in proven HIV programmes, particularly for young people and key populations,” said Michel Sidibé, Executive Director of UNAIDS. “If countries think they can treat their way out of their epidemics, they are dangerously mistaken.”
UNAIDS’ newly released report, Miles to go: closing gaps, breaking barriers, righting injustices, shows that 47% of new HIV infections globally are among key populations. Although combination HIV prevention approaches work for key populations, including harm reduction, pre-exposure prophylaxis (PrEP), social care and condoms, many countries are unwilling to invest in approaches viewed as culturally or religiously inappropriate, unpopular or counter to the bad laws that may exist in a particular country.
HIV prevalence can be high as up to 70% among sex workers in some southern African countries; however, about three quarters of countries reporting to UNAIDS criminalize some aspect of sex work and sex workers report that condoms are often confiscated by the police.
In eastern Europe and central Asia, one third of all new HIV infections are among people who inject drugs; however, 87% of countries reporting to UNAIDS criminalize drug use or possession of drugs, driving people underground and out of reach of HIV services. Many countries do not make sterile injecting equipment and opioid substitution therapy widely available, which is a huge barrier to efforts to bring down new HIV infections among this population and their partners.
Gay men and other men who have sex with men accounted for around 57% of new HIV infections in western and central Europe and North America in 2017 and an estimated 41% of new infections in Latin America. However, globally, access to HIV services for men who have sex with men is still being blocked by bad laws. Of 100 countries reporting to UNAIDS, at least 44 had laws specifically criminalizing same-sex sexual intercourse. The death penalty applied in two countries.
“If countries don’t provide comprehensive sexuality education, condoms, harm reduction or pre-exposure prophylaxis for key populations, this will ultimately translate into more new HIV infections, higher future treatment costs and a higher burden for health-care budgets and systems,” said Mr Sidibé.
Countries that have invested are seeing results. In Finland’s capital, Helsinki, for example, scale-up of harm reduction and HIV testing and treatment services led to a steep drop in new HIV infections and high rates of viral suppression among people who inject drugs. The number new HIV diagnoses in this key population decreased from more than 60 in 1999 to almost zero in 2014.
In San Francisco, United States of America, PrEP was added to programmes that include HIV testing, rapid linkages to antiretroviral therapy and boosting support for retention in care. Between 2013 and the end of 2016, there was a 43% decrease in new HIV diagnoses in the city, a decline that is being attributed to both quicker achievement of viral suppression among people who test HIV-positive and to increased uptake of PrEP.
Women and girls also need access to HIV prevention. In 2017, around 6500 women and girls were infected with HIV every week. Limited access to education, a lack of economic autonomy and a lack of decision-making power, including over their own health, expose them to intimate partner violence, limit their ability to practise safer sex and limit their ability to benefit from HIV and sexual and reproductive health services, making them more vulnerable to HIV infection.
Women and girls must have the knowledge and power to protect themselves against HIV in safe and enabling environments and must be able to access services that meet their needs. This requires countries to reform discriminatory laws that perpetuate inequality and develop and enforce laws that promote gender equality.
Young people also need age-appropriate youth-friendly health services. More than two thirds of countries reporting to UNAIDS require parental consent for a child under 18 years to access HIV testing, and more than half require consent for HIV treatment.
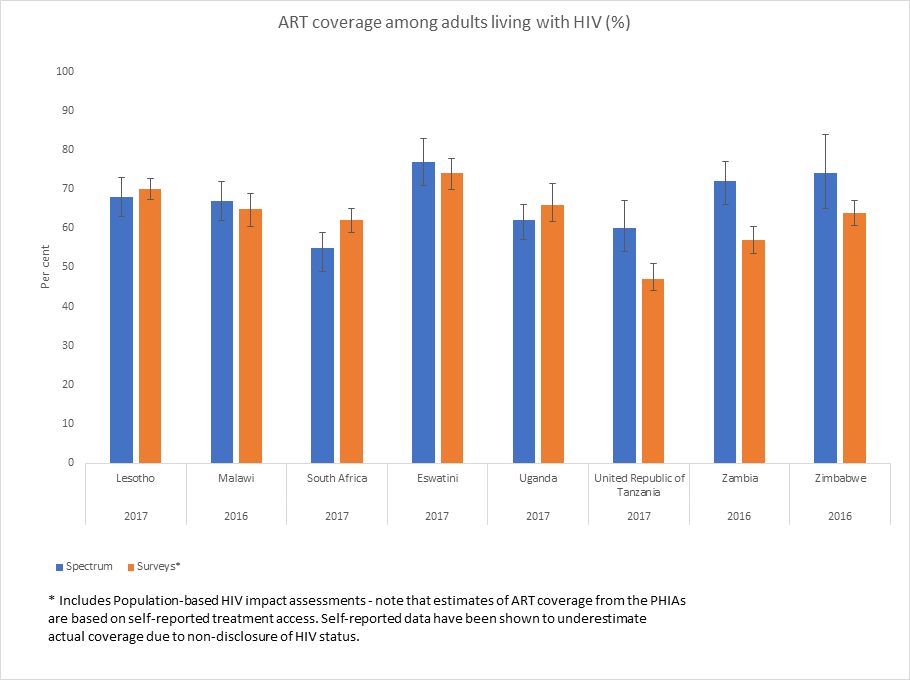
While most countries have significantly scaled up their HIV treatment programmes, some to the extent of reaching 80% of people living with HIV with antiretroviral therapy, the HIV prevention benefits of treatment that countries had hoped to achieve are not yet being realized. People are are not being diagnosed and treated soon enough, allowing transmissions to occur before they start treatment or if treatment is interrupted.
Botswana, for example, has nearly reached its 90–90–90* targets, as 86% of people living with HIV know their HIV status, 84% of people who know their status are on antiretroviral therapy and 81% of people on antiretroviral therapy are virally supressed. However, new HIV infections have failed to see any declines since 2010.
To urgently address the HIV prevention crisis and increase political commitment for HIV prevention, a Global HIV Prevention Coalition of United Nations Member States, donors, civil society organizations and implementers was established in 2017 that includes the 25 highest HIV burden countries.
The overarching goal of the Global HIV Prevention Coalition is to strengthen and sustain political commitment for primary HIV prevention by setting a common agenda—the HIV Prevention 2020 Road Map—among key policy-makers, funders and programme implementers to accelerate progress towards reducing new HIV infections by 75% by 2020.
On 23 July 2018, the Global HIV Prevention Coalition came together at an event at the International AIDS Conference in Amsterdam, Netherlands, to discuss the urgency for scaling up HIV prevention, share progress made and address persisting challenges, including policy barriers and inadequate financing for HIV prevention.
The Global HIV Prevention Coalition recently launched its first progress report, Implementation of the HIV Prevention 2020 Road Map, which shows that while initial progress has been made, more efforts are needed to move from political commitment to strong actions on the ground.
* 90% of people living with HIV know their HIV status, 90% of people who know their status are receiving antiretroviral treatment and 90% of people on treatment have suppressed viral loads.
For more information on the HIV prevention crisis, go to unaids.org.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.