By Winnie Byanyima, UNAIDS Executive Director
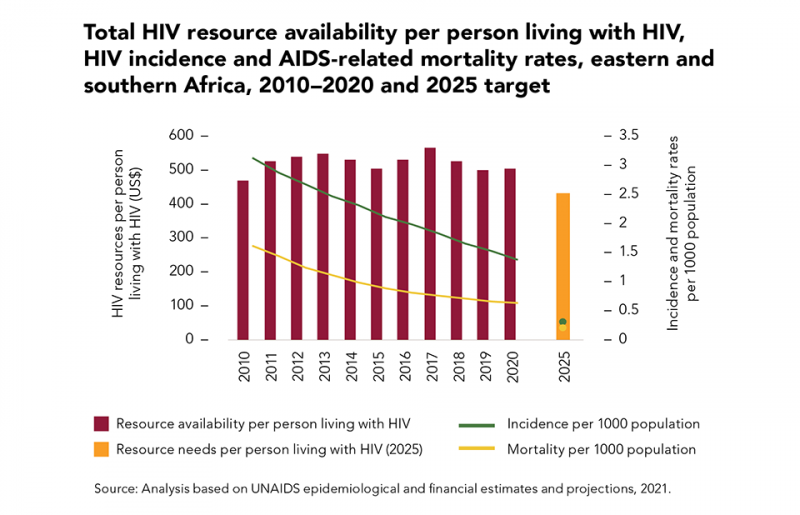
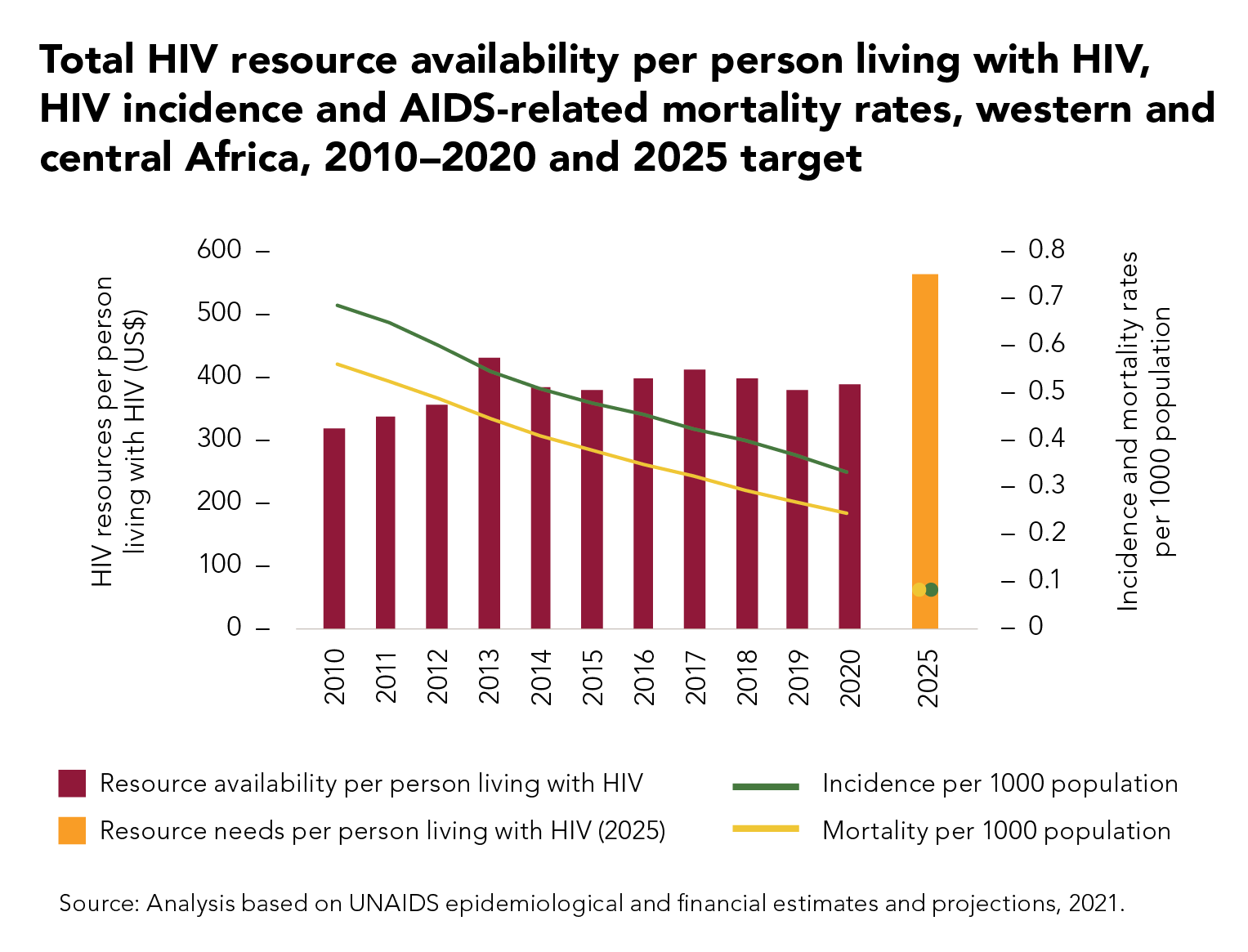
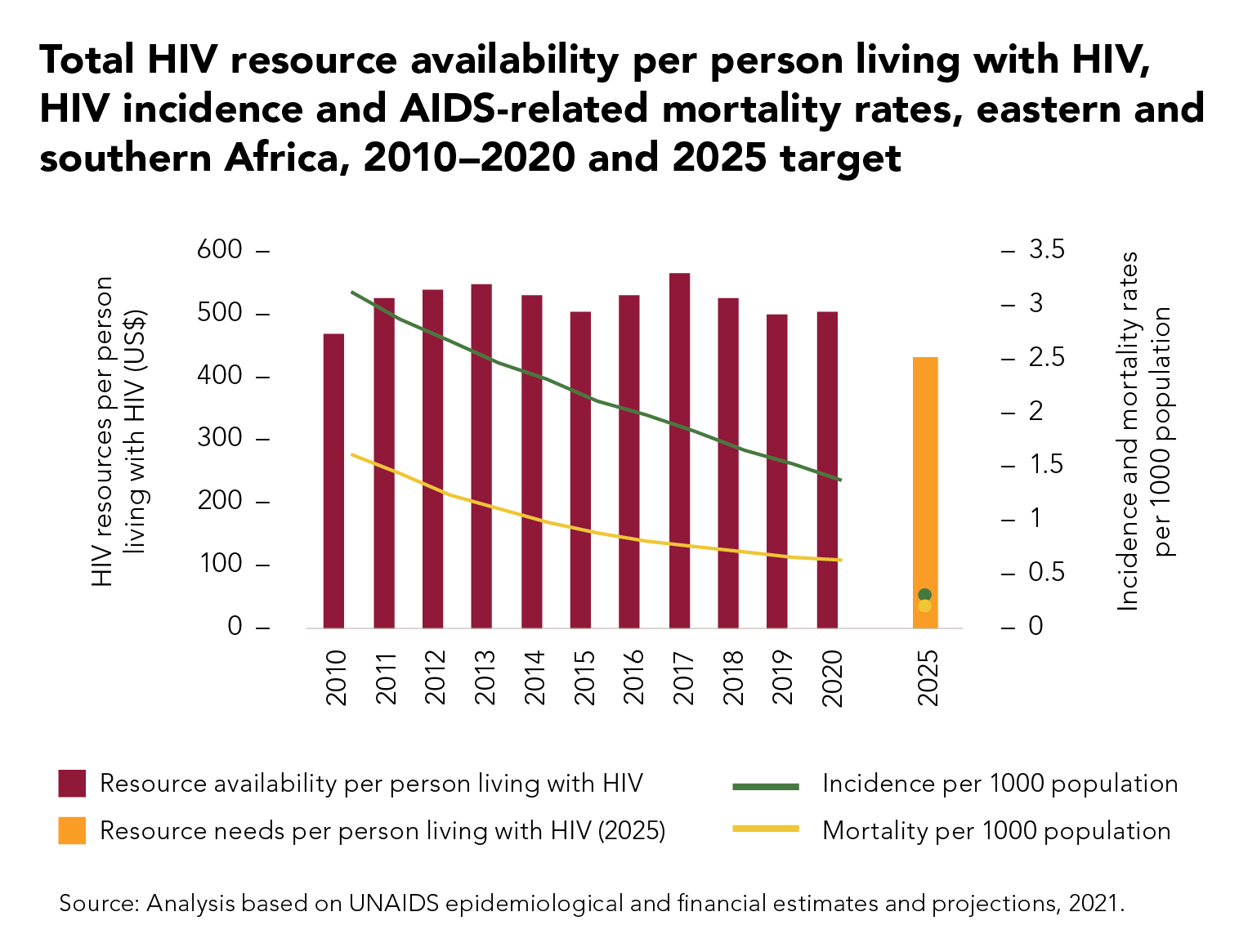
The AIDS epidemic in western and central Africa is an ongoing emergency. The early gains made against HIV in this region have not been translated into the sustained progress that has been made in other parts of sub-Saharan Africa.
Last year, there were 150 000 AIDS-related deaths in the region, and 200 000 people became newly infected with HIV. Every week more than 1000 adolescent girls and young women aged 15–24 years become infected with HIV in the region; 1.2 million people in western and central Africa are still waiting to initiate life-saving HIV treatment. Only 35% of children living with HIV in western and central Africa are on treatment.
Now the COVID-19 crisis has obstructed services and exacerbated the inequalities that drive the AIDS epidemic. If we don’t act now, not only will many more lives be lost, but containing the AIDS pandemic will be more difficult and expensive in the coming years.
Ending AIDS is achievable: there is a tested set of approaches that are proven to work, including in challenging settings.
From Cabo Verde’s leadership on the elimination of vertical transmission of HIV, to Cameroon’s decision last year to eliminate user fees for all HIV services at public health facilities and accredited community sites, examples that light the way are already there. By aligning policy with the evidence of what has succeeded, we can end AIDS as we promised.
Countries and communities are already leveraging the experience and expertise of the AIDS response to reduce the impact of COVID-19 across this region. From Côte d’Ivoire, to Guinea, to Senegal, public health authorities, international organizations, civil society actors and communities of people living with and affected by HIV have worked together to ensure that people living with HIV continue to receive their medication, to deliver care and prevention services in safe and innovative ways, to deliver food to people who have lost their incomes in lockdown, to convey messages about the importance of hygiene and social distancing in order to stay well and to dispel myths that feed stigma and discrimination and weaken public health messaging.
This spirit of cooperation and partnership is vital for stronger pandemic responses.
This week, hosted by the President of Senegal, Macky Sall, UNAIDS and the Civil Society Institute for HIV and Health in West and Central Africa are organizing a summit in Dakar on how to close the gaps in the region’s HIV response and strengthen pandemic preparedness.
Here are three of the bold actions we need to take.
First, embrace and enable communities to be at the centre of planning and delivery.
Communities know the situation on the ground—they must be given the resources and the space to lead. Countries need to ensure an enabling environment for communities to be involved in providing services as an integral part of the public health response, be involved as co-planners, be able to highlight experiences and concerns and be able to play their essential role ensuring accountability.
Countries need to lift those legal, policy and programmatic barriers that hold this back, and to scale up financial support to unleash the incomparable contribution of communities.
Second, increase investment.
Countries need to increase the scale of provision in prevention, testing and treatment and eliminate all financial barriers to ensure universal access to services.
The Abuja commitment to invest 15% of government budgets in public health needs to be met. Joint commitments made by health and finance ministers at the Africa Leadership Meeting to increase domestic revenues dedicated to health must be fulfilled.
International donors too have to step up with support at the time of the worst crisis in decades. Enabling the required fiscal space will require debt cancellation to support governments in scaling up investments in health and in tackling the social drivers of HIV and pandemic risk.
International action to prevent harmful tax competition and illicit financial flows is likewise key. It is difficult to advance towards fair and progressive taxation, and grow revenues, when large corporations and high-net-worth individuals are systemically enabled internationally to evade the taxes the ordinary citizen must pay, and which are essential for health, education, social protection and economic investment.
Third, address the inequalities that drive the epidemic.
COVID-19 has once again shown the world how epidemics thrive on inequalities, both between countries and within them. The new UNAIDS strategy adopted earlier this year puts the fight to end inequalities at the centre of the mission to end AIDS.
Inequalities drive HIV. Vulnerable groups of people represent 44% of new HIV infections in western and central Africa. Their partners represent a further 27%.
The ECOWAS Strategy for HIV, TB, Hepatitis B & C and Sexual and Reproductive Health and Rights among Key Populations puts it so well:
“the protection of human rights for all members of each key population is crucial to success. Laws that discriminate or create barriers should be reformed, to ensure that key populations are free from stigma, discrimination and violence and their vulnerability to HIV is reduced.”
Gender inequality likewise drives HIV: of the new HIV infections among young people in western and central Africa, almost three quarters are among adolescent girls and young women. The issue is power.
Research shows that ensuring that girls complete secondary education reduces their risk of acquiring HIV by up to half, and that combining this with a package of services and rights for girls’ empowerment reduces their risk further still.
The Education Plus initiative, co-convened by UNICEF, UNESCO, UNFPA, UN Women and UNAIDS, with governments, civil society and international partners, is helping to accelerate the actions and investments needed to ensure that every African girl is in school, safe and strong.
What we need to do to end AIDS is also what we need to do to enable Africa to rise.
Governments, international organizations, scientists, researchers, community-led organizations and civil society actors cannot be successful alone, but together they can create an unbeatable partnership and an unstoppable force to end AIDS as a public health threat by 2030.