

Feature Story
A tale of two Jamaican clinics during COVID-19
03 November 2020
03 November 2020 03 November 2020A woman living with HIV is at the Centre for HIV Research and Education Services (CHARES) in Kingston, Jamaica. She normally gets a three-month allotment of her antiretroviral medicines. But not this time. The doctor warns her that, since April, state pharmacies have only been dispensing a one-month supply.
About a 20-minute drive away at the Comprehensive Health Clinic, a client waits for his name to be called. He doesn’t use one of the wooden benches allocated for sexual health patients. Instead, he finds a nearby seat and listens intently.
HIV service providers in Jamaica have been challenged this year with responding both to new challenges caused by COVID-19 and long-standing service delivery stumbling blocks. The UNAIDS Country Director, Manoela Manova, wanted to get a better understanding of the issues on the ground, so she visited both treatment sites to speak with everyone, from adherence counsellors to doctors.
The University Hospital of the West Indies’ CHARES has been a best practice model for HIV treatment in Jamaica. For the island as a whole, 79% of those on treatment were virally suppressed last year. At CHARES, however, an impressive nine in every 10 clients are virally suppressed and therefore keep healthy and are unable to transmit the virus.
But even for this accomplished programme, COVID-19 has presented significant challenges.
Laboratory support has been diverted toward COVID-19 and there has been a backlog in receiving viral load testing results.
CHARES had been used to writing three-month prescriptions for stable clients, but since COVID-19, state-run pharmacies have been dispensing only a one-month supply. This is part of the government’s strategy to avoid stock-outs given the supply chain challenges at this time, but it means that those on treatment need to go out to get their medicines more often. CHARES has begun home deliveries, particularly for older people, who are more reluctant to venture out given the novel coronavirus risk.
COVID-19 containment measures have increased the need for mental health support. Income loss, school closures and curfews have placed an added strain on thousands of Jamaican households, including many people living with HIV. But when clients are referred to psychiatric support in the main hospital they rarely go for fear of experiencing discrimination. Further, since the hospital in which CHARES is located is a designated COVID-19 treatment site, some clients have opted to stay away.
“We need closer monitoring and evaluation to address the challenges around patient management at this time,” said CHARES Programme Director Racquel Brown. “Optimally we would like to hire someone with responsibility for analysing patient data to make more strategic decisions around care and treatment.”
The Comprehensive Health Centre serves a number of people living with HIV alongside those infected with other sexually transmitted infections. Here, too, multimonth dispensing has not been possible during COVID-19. Patients’ need for nutrition support has been high during this period. Some have had their antiretroviral medicines but no food with which to take them.
But other challenges came before COVID-19. Two out of five clients are lost to follow-up. Patients have given service providers wrong addresses. And the clinic’s viral suppression rate stands at 70%, below the national average. Some come off their treatment against their doctor’s advice.
Ms Manova said many of the challenges at both clinics are linked to self-stigma and discrimination, which is the main issue facing Jamaica’s HIV response. For the country as a whole, just 43% of all people living with HIV were on treatment in 2019 despite the island’s relatively high testing coverage.
“Before and during COVID-19, our results are undermined by shame, fear and prejudice,” she noted. “For an effective public health response, we have to be deliberate and consistent about building trust with communities and combatting all forms of stigma and discrimination that block people from accessing care.”
“It was inspiring and sobering to spend time with these health-care providers,” Ms Manova said. “Jamaica has correctly treated community health-care employees as essential workers. Staff including community facilitators, social workers, adherence counsellors and case managers are just as needed as doctors and nurses. Their work is critical at this time to address the individual needs and emotions that could affect treatment outcomes.”
Our work
Region/country
Related
 Multisectoral resilience to funding cuts in Guatemala
Multisectoral resilience to funding cuts in Guatemala
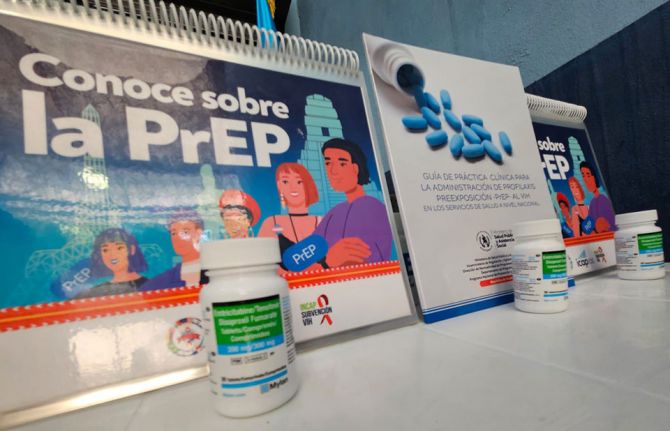
22 December 2025


