Feature Story
Five questions about the HIV response in the Gambia
31 October 2021
31 October 2021 31 October 2021In the lead up to the West and Central Africa Summit on HIV/AIDS taking place in Dakar from 31 October to 2 November 2021, UNAIDS asked its country directors across the region five questions about the AIDS response in their country. Here are the replies of Ms. Sirra NDOW, UNAIDS country director in the Gambia
“Existing resources, skills and medical equipment designed for the HIV response proved essential to address COVID-19 when it emerged in the Gambia. Going forward, the country will need to refocus its efforts on providing tailored support to the most at-risk key populations which have often discontinued their treatment during the pandemic. Committing to the protection and fulfillment of their rights is the first crucial step.”
Similar to other western African countries, the Gambia has a low but highly concentrated HIV epidemic, affecting heavily key populations such as men who have sex with men and female sex workers. While impressive progress towards reducing new adult and paediatric infections have been observed in recent years, COVID-19 has caused a lot of complications. Repurposing HIV medical equipment and health personnel to address the fast-rising epidemic was necessary to limit COVID-19 related deaths. It also came with a cost—reducing the capacity to deliver HIV prevention and treatment services.
Lessons must be learned from the dual HIV/COVID-19 epidemics. Effort must be invested in better prevention services, especially tailored to key populations. Health personnel must be better trained and better supported to manage their workload and prevent bottlenecks. The approach of task shifting/sharing must continue and be further complemented by the strengthening of community health workers and decentralization of services. Finally, no progress will be truly radical unless stigma, discrimination and violence against people living with HIV and other marginalized groups are eradicated.
1. What are the main areas of progress in your country’s response to the HIV epidemic in the last five years?
The HIV epidemic in The Gambia mirrors those prevailing in other West African countries: the epidemic is overall low—less than 2% of the general population—but highly concentrated among key populations. The most recent Integrated Biological Behavioural Surveillance Study (IBBS.2018) estimates that prevalence is over 35% among men who have sex with men (MSM) and over 10% among female sex workers (IBBS 2018).
In 2018, the Gambia started implementing WHO’s recommendation to provide all people living with HIV with lifelong antiretroviral therapy (ART) regardless of clinical status or CD4 cell count. Between 2015 and 2020, impressive progress happened as new infections were cut by half and new infections among children were reduced by 75% (National AIDS Strategic Plan,2020-2025). All pregnant women attending antenatal clinics are routinely offered HIV tests, and all pregnant women living with HIV are eligible for ART (Option B+). Until the COVID-19 epidemic started, ART uptake had increased significantly. The country also adopted task shifting for HIV/AIDS and malaria—typically enabling nurses to dispense ART and capacitating community health workers to deliver a range of HIV services.
2. What are the main challenges that still need to be addressed?
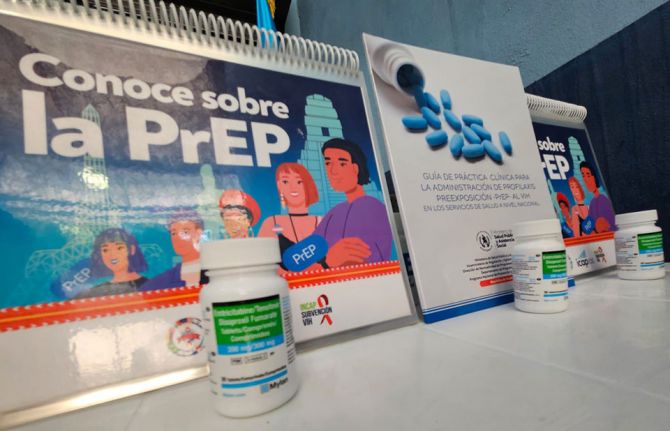
Despite increased outreach activities, the testing coverage remains very low with less than 40% of the estimated PLHIV knowing their status. Inadequate investment in HIV prevention programmes and lack of access to prevention services, especially among key population groups, continue to impede progress in the national HIV response. HIV prevalence has increased more than three-fold among MSM from less than 10% in 2011 to over 35% in 2018 (IBBS, 2018) and no program have been designed to accelerate the uptake of pre-exposure prophylaxis as a prevention strategy among MSM.
HIV-related human rights and gender situation in the Gambia has not improved in the past five years. Key populations suffer multiple burden of frequent human rights violations, systematic disenfranchisement, stigma, and discrimination. The existence of punitive laws perpetuates barriers to accessing HIV services for key populations and further contributes to their social and economic marginalization. There remains lots to be done on promoting human rights literacy, putting in place mechanisms to monitor and report human rights violations, and advocate for policy reform and sensitization of lawmakers on human rights and gender-related issues.
Inadequately trained human resources for health coupled with frequent transfers of experienced and trained staff continue to threaten the national response. Decentralizing services, engaging community health services sites should be prioritized to further expand prevention, treatment, and care services. Finally, tracking patients at ART centres is a challenge due to inadequate cross-border programmes. There is need to strengthen cross-border initiatives to enhance follow-ups, defaulter tracing and referral of patients on treatment.
3. How has COVID-19 affected the HIV response in your country?
In the Gambia, there was no public health facility adequately equipped to treat COVID-19 cases and patients were treated at the Medical Research Council. There was no public health laboratory for COVID-19 testing, so health professionals repurposed PCR machines, which were originally intended for HIV testing, to test for COVID-19. HIV laboratory staff were also requested to provide COVID-19 services in addition to routine HIV and TB services While such urgent actions were required by the emerging pandemic, it led to a severe disruption in HIV diagnosis and the delivery of HIV and TB treatment services.
Social unrest caused by the COVID-19 pandemic also impeded access to regular healthcare, including for people living with HIV (PLHIV) and resulted in disruptions of ART availability. Rapidly, a multi-month dispensation of ARVs was initiated to try to maintain continued availability of treatment for all stable PLHIVs. During this period, a sharp decline in the number of PLHIV on ART was observed as well as a decline in HIV testing services in the general population.
4. Who are the unsung leaders of the AIDS response in your country?
We commend the admirable work delivered by community health workers in the Gambia, and the outstanding solidarity displayed by the community of people living with HIV.
5. If you could ask your Head of State to change one thing to strengthen the HIV response, what would it be?
To be a champion for the AIDS responses and to commit to mobilize adequate resources for the response.