Update
Parental consent laws leave adolescents vulnerable to HIV
14 February 2022
14 February 2022 14 February 2022Sexual activity often starts during adolescence. Many countries have age of consent laws in relation to sexual activity that are inconsistent with minimum age laws for accessing sexual and reproductive health information and services without parental permission. This means that adolescents may legally have sex before they can legally access any information or services relating to safer sex practices or contraception, leaving them at greater risk of HIV, other sexually transmitted infections (STIs) and unwanted pregnancy.
The removal of laws that require parental permission to access services for sexual and reproductive health and HIV prevention, testing and treatment has been shown to improve health-seeking behaviours. That effect is even stronger when schools can provide age-appropriate comprehensive sexuality education to young people so they can protect themselves from HIV, STIs, unwanted pregnancy and gender-based and sexual violence.
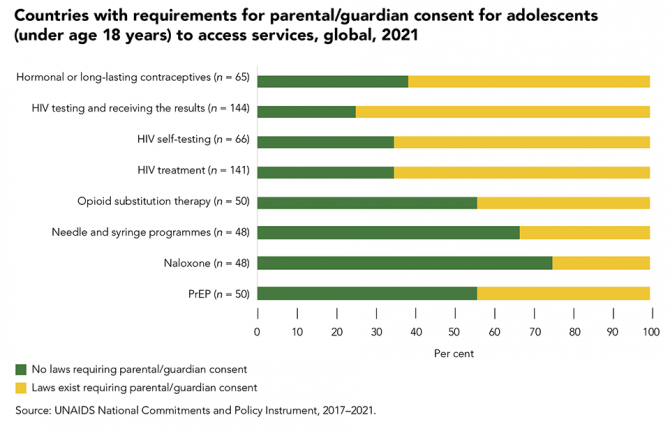
Forty countries reported to UNAIDS in 2021 that they have laws requiring parental/guardian consent for adolescents to access hormonal or long-lasting contraceptives, 108 reported that this consent is required for an HIV test, 43 for HIV self-testing, 92 for HIV treatment and 22 for PrEP. Among these countries, some provide exceptions based on demonstrated maturity: 10 for hormonal or long-lasting contraceptives, 15 for HIV testing, eight for self-testing and nine for HIV treatment. The age cut-off of parental consent laws varied by service. The majority of countries that reported having requirements for parental/guardian consent had an age cut-off of 18 years, with exceptions in a few countries where adolescents as young as 14 years could access a service without parental/guardian consent, which varied by service.
Our work
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025