Feature Story
UNAIDS reaffirms its partnership with Global Fund as board meeting concludes
07 May 2009
07 May 2009 07 May 2009 UNAIDS Executive Director Michel Sidibé opened a technical session on “The Global Fund's role as a strategic and responsible investor in HIV/AIDS” during the 19th Board Meeting of the Global Fund to Fight AIDS, Tuberculosis and Malaria. Geneva, 6 May 2009.
UNAIDS Executive Director Michel Sidibé opened a technical session on “The Global Fund's role as a strategic and responsible investor in HIV/AIDS” during the 19th Board Meeting of the Global Fund to Fight AIDS, Tuberculosis and Malaria. Geneva, 6 May 2009. Credit: Global Fund to Fight AIDS, Tuberculosis and Malaria/Philippe Christin
The 19th Board Meeting of the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) concluded yesterday in Geneva, Switzerland. Opening a technical session on “The Global Fund's role as a strategic and responsible investor in HIV/AIDS” earlier, UNAIDS Executive Director Michel Sidibé reaffirmed UNAIDS commitment to its partnership and reiterated his call for a fully funded Global Fund. He called for bolder action in order to address the challenges facing the AIDS response.
Michel Sidibé spoke of the need for smarter investments in the AIDS response: “as long as there are five people newly infected for every two people starting HIV treatment we will not change the trajectory of the epidemic.” He also called for the virtual elimination of mother-to-child transmission by 2015.
Mr Sidibé emphasized the importance of the mechanism provided by the Global Fund in addressing global health challenges and identified this time of economic crisis as an opportunity for change: “in this time of crisis, today’s topic - investing strategically and responsibly – is needed now more than ever.”
Investing in the AIDS response

Elizabeth Mataka, UN Special Envoy of the Secretary-General for HIV/AIDS in Africa spoke during the technical session on “The Global Fund's role as a strategic and responsible investor in HIV/AIDS” during the 19th Board Meeting of the Global Fund to Fight AIDS, Tuberculosis and Malaria. Geneva, 6 May 2009.
Credit: Global Fund to Fight AIDS, Tuberculosis and Malaria/Philippe Christin
The session was jointly developed by UNAIDS, UNICEF, WHO and the office of the Global Fund Chair.
Two aspects in particular were explored: ways to reduce costs while simultaneously improving quality of care to people living with HIV; and how to improve grant effectiveness targeting prevention of mother-to-child transmission of HIV and pediatric AIDS treatment through promoting integrated efforts.
Participants also discussed how the Global Fund can achieve higher impact in its investments and play a more effective role as a financing instrument and a partnership in supporting a comprehensive approach to HIV.
Mr Sidibé outlined the challenges needed to achieve universal access to HIV prevention, treatment, care and support which include country owned and evidence driven responses grounded in human rights. He spoke of the key role the Global Fund plays in this.
The Global fund is a key partner in the global movement to achieve universal access. It is among the most innovative and results-driven health financing mechanisms ever established.
UNAIDS Executive Director Michel Sidibé
“The Global fund is a key partner in the global movement to achieve universal access. It is among the most innovative and results-driven health financing mechanisms ever established,” said Mr Sidibé.
Mr Sidibé referred to UNAIDS Outcome Framework emphasizing the importance for UNAIDS —Secretariat and Cosponsors— to focus on areas where it has a comparative advantage and can make a difference to accelerate progress in AIDS and strengthen synergies with the other Millennium Development Goals.
The session considered how to address the increasing costs of meeting the treatment needs of people living with HIV, and identified the need for significant success in preventing new infections in order to get ahead of the AIDS epidemic.
 The 19th Board Meeting of the Global Fund to Fight AIDS, Tuberculosis and Malaria took place in Geneva 5-6 May 2009
The 19th Board Meeting of the Global Fund to Fight AIDS, Tuberculosis and Malaria took place in Geneva 5-6 May 2009 Credit: Global Fund to Fight AIDS, Tuberculosis and Malaria/Philippe Christin
The two day board meeting also included a review of strategy in relation to sexual orientation and gender identity and a presentation of a five-year evaluation report examining partnerships at global and country levels and impact these relationships have on the successful implementation of Global Fund grants. Recognizing the overall achievements of the Global Fund in its first six years, the evaluation highlighted a number of areas where it suggests improvements are required in the establishment of more effective partnerships.
The Global Fund is the world's largest funding mechanism of programmes addressing AIDS, tuberculosis and malaria. A total of US$ 15.6 billion has been approved for programmes in 140 countries and with expected disbursements of US$ 2.9 billion in 2009.
Right Hand Content
Partners:
The Global Fund to Fight AIDS, Tuberculosis and Malaria
Speeches:
Feature stories:
Call for fully funded Global Fund to fight AIDS, Tuberculosis and Malaria (31 March 2009)
New tool distills guidance on writing strong Global Fund HIV proposals (02 February 2009)
UNAIDS and The Global Fund sign cooperation agreement (03 June 2008)
External links:
Official web site of Nineteenth Meeting of the board of the Global Fund
Publications:
Joint action for results: UNAIDS outcome framework, 2009 – 2011 (pdf, 388 Kb.)
Five-Year Evaluation Study Area 2: Global Fund Partner Environment at Global & Country Levels

Feature Story
Strengthening and expanding HIV legal services
06 May 2009
06 May 2009 06 May 2009
People living with or affected by HIV often require practical assistance to maintain adequate housing, keep child custody, enforce property and inheritance rights, or access health care, education or employment without discrimination.
Credit: UNAIDS/P.Virot
Experience in the response to AIDS has shown that access to legal services is an important part of guaranteeing protection from discrimination, getting redress for human rights violations, and expanding access to HIV prevention and treatment. Yet such programmes are not sufficiently supported by national AIDS responses, and where they do exist, quality and scale are often insufficient.
The International Development Law Organization (IDLO), the UNAIDS Secretariat and the United Nations Development Programme (UNDP) hosted an international expert consultation on strengthening and expanding HIV legal services at IDLO headquarters in Rome, 3-6 May.
Meeting participants contributed to the development of tools for improving access to legal services for people living with HIV and key populations at higher risk of HIV infection, particularly those in low- and middle-income countries. The tools will support countries to develop and strengthen programmes and proposals for funding, including to the Global Fund to Fight AIDS, Tuberculosis and Malaria.
Susan Timberlake, Senior Human Rights and Law Adviser with the UNAIDS Secretariat, explains that UNAIDS advocates that access to justice must be a basic, programmatic component of the movement for universal access to HIV prevention, treatment, care and support. “The persistent reality of discrimination – whether due to HIV status, gender, or social status – means that legal services are a critical and necessary part of a comprehensive response to the epidemic,” says Timberlake.
People living with or affected by HIV often require practical assistance to maintain adequate housing, keep child custody, enforce property and inheritance rights, or access health care, education or employment without discrimination. Access to legal services is even more important in punitive legal environments. An increasing number of countries are passing overly-broad laws to criminalize HIV transmission. Men who have sex with men, sex workers and people who use drugs face criminal sanctions in many countries, blocking access to HIV services and heightening HIV vulnerability. According to research commissioned in 2008 by the International Task Team on HIV-related Travel Restrictions, some 60 countries deny entry, stay and residence based on HIV status.
No “one size fits all” for legal services
Legal services in the context of HIV take many forms. These include: legal information and advice, including through telephone “hotlines”; formal litigation, including strategic litigation to create legal policy; mediation and other forms of dispute resolution; assistance with informal or traditional legal systems (e.g. village courts); and community legal education. Legal service providers are not always lawyers. They may be paralegals, volunteers, students or peer educators. Such services are provided in a range of settings, including HIV treatment and counselling centres, “mainstream” legal aid centres, as well as prisons and community settings. Work may also be linked to advocacy for law reform.
According to Mandeep Dhaliwal, Cluster Leader on Gender, Human Rights & Sexual Diversities with the UNDP HIV Practice, the rationale for supporting HIV legal services rests on two related arguments. “One, they are essential as a means to protect the human rights of marginalized and vulnerable populations. Two, they are essential as a means to ensure optimal public health and development outcomes – both of which are underpinned by the realization of rights,” says Dhaliwal.
One of our goals as the Joint UN Programme on HIV/AIDS is to support countries to recognize how important legal services can be to their national HIV response, and then work with them to develop a strategy to scale-up these services.
Mandeep Dhaliwal, Cluster Leader: Gender, Human Rights & Sexual Diversities UNDP HIV/AIDS Practice Bureau for Development Policy
However, too often such programmes do not get the support they need. “One of our goals as the Joint UN Programme on HIV/AIDS is to support countries to recognize how important legal services can be to their national HIV response, and then work with them to develop a strategy to scale-up these services,” explains Dhaliwal. “Existing HIV legal services are generally small in scale and patchy in coverage. With high levels of ‘legal’ marginalization of vulnerable populations, the achievement of universal access to prevention, treatment, care and support demands a commitment to legal protection and access to legal services.”
The meeting in Rome supported the development of three tools to improve access to HIV legal services:
- Models of legal services applicable in different situations
- Training curriculum for lawyers
- Resource mobilization strategies.
“There are extraordinary examples of great work being done to provide legal services. We know the importance of providing an enabling legal environment to HIV prevention and treatment access,” says David Patterson, Manager of IDLO's HIV and Health Law Programme, “Why have such legal services not been taken to scale with the same urgency that we seek to provide treatment?”
Participants included legal service providers and leaders of organizations working with people living with HIV, women’s groups, people who use drugs, men who have sex with men and sex workers, as well as representatives from IDLO, UNAIDS, UNDP, and the Global Fund. They came from diverse countries and epidemic settings, including Australia, Botswana, Brazil, China, Denmark, Egypt, Georgia, Guatemala, India, Indonesia, Nepal, Papua New Guinea, St Lucia, Uganda, Ukraine, the United States of America and Viet Nam.
Right Hand Content
Cosponsors:
External links:
International Development Law Organization (IDLO)
Publications:
International Guidelines on HIV/AIDS and Human Rights (pdf, 932 Kb)
Related

Feature Story
HIV response and the education sector: UNESCO Best practice series
04 May 2009
04 May 2009 04 May 2009 The five booklets in UNESCO’s Good Policy and Practice in HIV & AIDS and Education aim to help education sectors in developing countries mount an effective response to HIV.
The five booklets in UNESCO’s Good Policy and Practice in HIV & AIDS and Education aim to help education sectors in developing countries mount an effective response to HIV.The negative impact of HIV is felt on education systems and schools, learners and teachers around the world from children dropping out of school to care for sick parents to the loss of teachers in their most productive years. As part of efforts to support governments, donors, NGOs, education planners and managers, school governing bodies and teachers in dealing with the implications of the epidemic and to share knowledge on effective responses, UNESCO has developed a best practice series entitled Good Policy and Practice in HIV & AIDS and Education.
The booklets in the series are broad in scope and highlight issues and lessons learned in a range of settings in developing countries. They examine policies, programmes and activities by a variety of actors and draw lessons from case studies and a review of both published and unpublished literature.
 Credit: Copyright 2003 Harvey Nelson, Courtesy of Photoshare.
Credit: Copyright 2003 Harvey Nelson, Courtesy of Photoshare.Out-of-school learners are also a focus of the series. For example, in Zambia, an interactive radio programme which provides access to education in an informal setting, for children who are unable to attend school is featured. Produced by the Ministry of Education Broadcasting Services Department, the weekday shows integrate life skills and HIV prevention into lessons on literacy, mathematics and other subjects. Drama, songs and participatory activities are used to introduce the lessons. The project, operating in 450 sites, covers 180,000 children, most of them orphans, and almost 50% of them girls.
UNESCO hopes that a best practice in one educational institution, ministry, country or region can be adapted and used effectively elsewhere.
The first booklet provides an overview and examines policy and programme responses. It also focuses on the need for more data and research around education sector responses to the AIDS epidemic.
The second has learners at its centre: their rights to education, protection, knowledge and skills, and care and support. One aspect examined is the exploration of successful prevention programmes for young people. In Namibia, for instance, the My Future is My Choice project has operated for over 10 years promoting AIDS prevention in schools. It aims to protect young people from HIV and other sexually transmitted infections, unwanted pregnancies and alcohol and drug abuse, by encouraging them to think for themselves and take responsibility for their future and their own development.
 Credit: Copyright 2005 Netsanet Assaye, Courtesy of Photshare
Credit: Copyright 2005 Netsanet Assaye, Courtesy of PhotshareIn booklet three, attention is turned towards educators and their role. It discusses their needs for training, care and support and the importance of their conduct in ensuring safe and secure learning environments. The fourth concentrates on the importance of strategic partnerships at multiple levels (i.e. global, regional, and within countries), of involving people living with HIV, and of working with children and young people. The fifth and final booklet in the series explores effective learning and quality education. It summarizes factors contributing to effective learning in the context of AIDS education and highlights issues to consider in developing and adapting relevant learning materials.
For UNESCO, Good Policy and Practice in HIV & AIDS and Education is a ‘living’ resource which will be expanded and refined as new knowledge and strategies become available. This series is considered a tool, a stepping stone, to support the education sector’s full engagement in national responses to the AIDS epidemic.
Right Hand Content
Good Policy and Practice in HIV & AIDS and Education:
Booklet 1: Overview
Booklet 2: HIV & AIDS and Safe, Secure and Supportive Learning Environments
Booklet 3: HIV & AIDS and Educator Development, Conduct and Support
Booklet 4: Partnerships in Practice
Booklet 5: Effective Learning
Cosponsors:
Feature stories:
Supporting young learners living with HIV in Namibia and Tanzania (23 December 2008)
ICASA 2008: Courage and hope, African teachers living positively (03 December 2008)
Publications:
Toolkit for Mainstreaming HIV and AIDS in the Education Sector: Guidelines for Development Cooperation Agencies. (UNAIDS IATT on Education, 2008)
( En | Fr | Es ) (pdf, 1Mb | 904 Kb | 1 Mb)
Improving the education response to HIV and AIDS: Lessons of partner efforts in coordination, harmonisation, alignment, information sharing and monitoring in Jamaica, Kenya, Thailand and Zambia. (UNAIDS IATT on Education, 2008) (pdf, 791 Kb.)
Advocacy Briefing Notes – Girls’ Education and HIV Prevention. (UNAIDS IATT on Education, 2008) (pdf, 253 Kb.)
Advocacy Briefing Notes – HIV and AIDS Education in Emergencies. (UNAIDS IATT on Education, 2008) (pdf, 275 Kb.)
Advocacy Briefing Notes – Mainstreaming HIV in Education. (UNAIDS IATT on Education, 2008) (pdf, 277 Kb.)
Advocacy Briefing Notes – Teachers Living with HIV and AIDS. (UNAIDS IATT on Education, 2008) (pdf, 273 Kb.)
Related

Feature Story
Influenza A(H1N1) and HIV infection
01 May 2009
01 May 2009 01 May 2009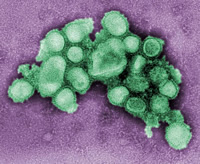 "Swine influenza"
"Swine influenza"Credit: C. S. Goldsmith and A. Balish, CDC
There are many questions concerning the potential impact of emerging influenza A(H1N1)* on people living with HIV, as they are more susceptible to opportunistic infections.
There is no documented information on clinical interactions between HIV and influenza A(H1N1) virus, whose transmission, incubation period and clinical manifestations have generally been similar to those of seasonal influenza viruses. Although there are inadequate data to predict the impact of a possible human influenza pandemic on people living with HIV, interactions between HIV and A(H1N1) influenza could be significant. Country preparedness plans for influenza should address the needs of people living with HIV, and national AIDS plans, especially in high HIV prevalence countries, should consider public health action required in case of pandemic influenza.
The World Health Organization has prepared a guidance note to assist countries and health workers in understanding the relevant risks and taking appropriate measures.
*As of 30 April 2009, WHO refers to the new influenza virus as influenza A(H1N1).
Right Hand Content
Related

Feature Story
'Never abandon, never give up’: ILO film helps China’s migrant workers challenge AIDS stigma
30 April 2009
30 April 2009 30 April 2009
Wang Baoqiang, star actor and former migrant construction worker is now a spokesperson for the ILO HIV/AIDS project in China Credit: courtesy of ILO
Zhang Xiao Hu is one of China’s estimated 200 million migrant workers. He is also one of the stars of ‘Never abandon, never give up’, a short Charlie Chaplin-style film aimed at reducing HIV stigma and promoting condom use among the country’s migrant workers. Beginning on 4 May, the International Labour Organization (ILO) and Mega-info Media, the company which runs China’s national railway station television network, will begin screening the film in 500 stations in 450 cities across the country. Over a three month period, 40 million people will have an opportunity to see the film.
In the film Zhang plays a construction worker stigmatized because he is living with HIV. This mirrors his real life situation as he is China’s first internal migrant worker to speak out publicly about his HIV status and has suffered stigma in the past from colleagues. As he says, “No one wanted to work with me, eat with me or share a dormitory.”
Leading filmmaker Gu Changwei
‘Never abandon, never give up’ is produced and directed for the ILO by Gu Changwei, a winner at the 2005 Berlin Film Festival and considered one of the leading filmmakers working in China today. Established star Wang Baoqiang, who is now serving as a spokesperson for the ILO HIV/AIDS project in China, also takes a lead role in the movie. He befriends Zhang Xiao Hu at his workplace and uses his celebrity persona to encourage his colleagues to cast aside their prejudices.
‘Hometown Fellows’ campaign
The project forms part of the ‘Hometown Fellows’ campaign where the ILO, in partnership with the Ministry of Labour, employer and worker bodies, and the State Council AIDS Working Committee Organization is collaborating with 19 large-scale enterprises in construction, mining and transport sectors in China’s provinces most affected by HIV. Although overall prevalence of the virus is relatively low in China (UNAIDS reported a 0.1% prevalence in 2008), there are pockets of high infection among specific populations and in some localities. With support from grass roots non-governmental organizations, the ILO is carrying out a comprehensive, multi-channel behaviour change programme for 190,350 internal migrant workers in Guangdong, Yunnan and Anhui provinces.
According to Constance Thomas, Director of the ILO in China, partnering with authorities on such projects, “helps us reach out to the workers for social protection to ensure their occupational safety and health…They do have the right to work in China and they have the right not to be discriminated against.”
The ‘Hometown Fellows’ project is intended to address high HIV-related stigma and low condom use among migrants and taps into powerful social networks among migrant workers who often move from rural areas and work together in large cities throughout China.
Formative research among the migrants shows a strong social bond based on common provincial origin that is potentially influential on attitudes and behaviour. This is in sharp contrast to migrant worker perceptions of health officials, company management and receiving communities, where there is, typically, considerable distrust and a sense of alienation.
The ILO behaviour change communication strategy has two tiers. Firstly, it has developed a range of communication tools based on the hometown fellowship concept where key message are delivered through migrant voices. Never abandon, never give up forms part of this intervention.
This movie is an excellent production which can help to reduce stigma and discrimination against people living with HIV far beyond the labour sector. It addresses not only stigma related to HIV, but also vulnerabilities linked with living at the margins of society.
Dr Bernhard Schwartlander, UNAIDS Country Coordinator in China
Secondly, working through enterprise structures, the programme taps into existing migrant social networks to deliver peer education in the workplace, dormitories and nearby entertainment areas. This peer education is reinforced through group training in enterprises as well as targeted messages delivered through company owned television and radio channels.
Dr Bernhard Schwartlander, UNAIDS Country Coordinator in China applauds this production, "This movie is an excellent production which can help to reduce stigma and discrimination against people living with HIV far beyond the labour sector." He added, "It addresses not only stigma related to HIV, but also vulnerabilities linked with living at the margins of society."
Migrant workers make up some 15% of the total Chinese population according to official estimates and they are considered vulnerable to HIV due to challenging social conditions, low HIV knowledge and lack of access to quality health services.
Right Hand Content
Cosponsors:
Feature stories:
‘Love and Relationships’: Film festival in Cambodia addresses HIV prevention (06 April 2009)
New report shows Asian migrant women in the Arab states have heightened vulnerability to HIV (10 March 2009)
Love in a Time of HIV (19 December 2008)
Powerful film brings AIDS issues to communities in Democratic Republic of Congo (16 June 2008)
Publications:
Migrants and HIV: Far away from home club (pdf, 899 Kb.)
Reducing HIV stigma and discrimination: a critical part of national AIDS programmes (pdf, 598 Kb.)
Art for AIDS (pdf, 2.11 Mb.)

Feature Story
Funding for AIDS drugs in jeopardy as global financial crisis hits health sector
28 April 2009
28 April 2009 28 April 2009The current crisis in financial markets and the world economy is having a profound effect on both governments’ global development commitments and national resources. Households already most vulnerable to poverty, risk further impoverishment as unemployment rises and incomes are reduced. There is widespread concern that progress in health and education will be severely undermined.
This is the second in a series of articles on the how the economic downturn impacts people already affected by HIV and how investment in sustainable financing is critical for global AIDS and development responses. The World Bank has just published a report that explores these issues in depth.

Averting a Human Crisis during the Global Downturn: Policy Options from the World Bank's Human Development Network states that a number of countries are already facing shortages of AIDS drugs due to the economic crisis.
Credit: Courtesy of the World Bank
The worldwide economic downturn may already be causing hardship in supplying life-saving drugs to people with HIV, according to a new World Bank report which highlights the clear and rising human cost of the current financial climate.
Averting a Human Crisis During the Global Downturn: Policy Options from the World Bank's Human Development Network, reports preliminary findings from a survey in 69 countries showing that 8 countries already face shortages of antiretroviral (ARV) drugs or other disruptions to AIDS treatment. The survey, conducted by the World Bank, UNAIDS and the World Health Organization last month also contends that, in total, respondents in 22 countries in Africa, the Caribbean, Europe and Central Asia, and Asia and Pacific expect the crisis to impact treatment programmes over the coming year. Together, these countries are home to more than 60 percent of people worldwide on ARVs.
This is a serious development. Despite rapid recent expansion in the numbers of people receiving treatment, two thirds of those in need of such drugs still do not get them. And unmet need is growing faster than treatment access is expanding. The global crisis seems likely to exacerbate the situation.
"This new report shows that people on AIDS treatment could be in danger of losing their place in the lifeboat,” says Joy Phumaphi, the World Bank's Vice President for Human Development and former Health Minister for Botswana.
Prevention programmes in jeopardy
We cannot afford a ‘lost’ generation of people as a result of this crisis. It is essential that developing countries and aid donors act now to protect and expand their spending on health, education and other basic social services and target these efforts to make sure they reach the poorest and most vulnerable groups.
Joy Phumaphi, the World Bank's Vice President for Human Development
HIV prevention programmes are also in jeopardy. The report states that survey respondents in 34 countries, where 75 percent of people with the virus live, expect prevention programmes for their key populations at higher risk (including sex workers and people who inject drugs) to be adversely affected as they are marginalized and tend to get lower priority than say pregnant women and children.
The world has made an international commitment to providing universal access to HIV prevention, treatment, care and support services to those in need by 2010. The global scale up towards this key goal, which has been gathering momentum, may well be threatened by what the report calls “these extraordinarily challenging times for the global economy.”
In Averting a Human Crisis During the Global Downturn, the Bank is encouraging countries which depend extensively on external donor AIDS financing to identify impending cash shortages as far as possible in advance, and to liaise with the Bank and other partners to help to mobilize 'bridge financing' that prevents interruptions to AIDS treatment. At the same time, the Bank warns that maintaining and expanding effective HIV prevention programmes during the current crisis is essential to guard against a resurgence of new infections.
Potential cuts in health and education financing
The World Bank is concerned that the downturn will lead to cuts in health and education financing across the board, not only in the sphere of AIDS. The report also shows how previous crises have forced developing countries to cut back on spending in these areas. Evidence from past downturns in Argentina, Indonesia, Thailand, and Russia shows that governments were forced to cut health services as a result of shrinking budgets and that returning health spending to pre-crisis levels took up to 10-15 years.
”We cannot afford a ‘lost’ generation of people as a result of this crisis,” Phumaphi contends. “It is essential that developing countries and aid donors act now to protect and expand their spending on health, education and other basic social services and target these efforts to make sure they reach the poorest and most vulnerable groups.”
In support of this strategy, on 24 April the World Bank stated that it was mobilizing up to US$ 3.1 billion this year in health financing to help poor countries battle threats to their social services during the global crisis. This effectively triples Bank support from US$ 1.0 billion in 2008 and will be used to strengthen health systems in poor countries, boost their performance in preventing and treating communicable diseases, and improving child and maternal health, hygiene and sanitation.
The Bank also said it was doubling its education financing this year in low- and middle-income countries to US$ 4.09 billion.
This report draws heavily on ongoing collaborative work by the World Bank, UNAIDS and WHO which will be released soon in a joint publication. Information was collected by agency representatives working closely with the National AIDS authorities in 69 low- and middle-income countries, which together include most people on treatment in the developing world. Preliminary conclusions are referenced here for consideration at the 2009 IMF World Bank Spring Meetings in Washington DC.
Funding for AIDS drugs in jeopardy as global fina
Cosponsors:
Feature stories:
HIV and high food prices (01 April 2009)
Minister of Foreign Affairs of the Russian Federation discusses financial crisis with UN agencies (09 March 2009)
As global economy slows International Health Partners push for faster health progress (12 February 2009)
Publications:
Averting a Human Crisis During the Global Downturn: Policy Options from the World Bank's Human Development Network (pdf, 1.09 Mb.)
Related

Feature Story
International Technical Consultation on ‘Positive Prevention’
27 April 2009
27 April 2009 27 April 2009 The concept of ‘positive prevention’ provides an opportunity to highlight the prevention needs of people who know their positive serostatus.
The concept of ‘positive prevention’ provides an opportunity to highlight the prevention needs of people who know their positive serostatus.Ever since HIV testing was developed in the early days of the epidemic, the role of people living with HIV in HIV prevention has been an important aspect of the AIDS response. Following the advent of combination antiretroviral treatment which significantly prolongs life and improves quality of life for people living with HIV, there have been increasing calls to incorporate what is known as ‘positive prevention’ in the continuum of prevention and care programmes and services.
The concept of ‘positive prevention’ provides an opportunity to highlight the prevention needs of people who know their positive serostatus, and is a useful lens through which to understand the important linkages between prevention, treatment, care and support.
However, despite increasing funding directed towards positive prevention, there is a lack of clear understanding globally and regionally of the concept, objectives and programmatic features of ‘positive prevention’, either within the community and representatives of people living with HIV, or between civil society and other partners.
As a direct consequence, the Global Network of People living with HIV (GNP+) and UNAIDS are convening a technical consultation on 27-28 April 2009 in Tunisia on the subject to help develop a common understanding of ‘positive prevention’, as well as guidelines and action plans to inform policies and programmes.
The term ‘positive prevention’ itself will be discussed during the technical consultation as, even though it is the most commonly used term, other terms are also used by different organizations and programmes such as ‘Prevention and Care for People Living with HIV/AIDS’ or ‘prevention with HIV-positive people’.
Participants at the consultation will represent civil society, government agencies, UNAIDS Cosponsors and Secretariat and international development agencies. A majority of the participants will be people living with HIV as the conversation around positive prevention has too often occurred without the involvement of people living with HIV at the design stage and has led to significant shortcomings in most current approaches.
The technical consultation follows the significant Positive Leadership Summit held in Mexico in 2008 and is part of an ongoing process to ensure that positive prevention efforts are based on a solid consensus among positive people. To that end, experts will identify strategies to gather experiences and knowledge of stakeholders, in particular people living with HIV at regional, national and local levels.
 If the prevention needs of positive people are to be adequately addressed, people who know they are living with HIV must be involved in defining and developing programmes.
If the prevention needs of positive people are to be adequately addressed, people who know they are living with HIV must be involved in defining and developing programmes.It is expected that the meeting will facilitate the development of a set of principles that will guide the work of and partnerships between multilateral, bilateral, governmental and civil society organizations in designing positive prevention programmes. Participants will also develop recommendations on the scaling up of programmes and policies, informed by the local context.
“Positive prevention” programmes
Many HIV programmes worldwide seek to include people living with HIV in their prevention efforts. Diverse programmatic activities are undertaken, including support for self-help groups and community empowerment, counselling in the context of HIV testing or of family planning, engagement of positive people in education programming (e.g. in delivering personal testimonies), and behaviour change programming directed at HIV-positive people or discordant partners. The aims of these programming efforts vary widely, and are not always explicit or consistent. Quite often, positive prevention programmes have focused on HIV testing and so are seen as irrelevant to people who already know their serostatus. Most existing interventions focus almost entirely on preventing the onward transmission of HIV, which may be counter-productive to programmes intended to address prevention, care and support for HIV positive people in a holistic manner.
If the prevention needs of positive people are to be adequately addressed, people who know they are living with HIV must be involved in defining and developing programmes. A human rights approach combating stigma and discrimination is essential to the success of positive prevention. Positive prevention requires addressing social vulnerabilities such as poverty, gender-based violence, xenophobia and homophobia. It is also inextricably linked with access to treatment, care and support.
While most agree that among the measures of success of positive prevention is the reduction of HIV transmission, it is also widely felt that positive prevention should not be exclusively about preventing onward transmission of HIV. The discussion about positive prevention needs to explore the efforts of people who know they are living with HIV to learn and practice ways to promote their own health and prevent disease.
Right Hand Content
Feature stories:
Positive Leadership Summit 2008 (31 July 2008)
HIV positive leaders meet in Monaco (25 January 2008)
Multimedia:
Listen to Rodrigo Pascal, UNAIDS Partnerships Officer
External Links:
Global Network of People Living with HIV/AIDS (GNP+)
Publications:
Practical guidelines for intensifying HIV prevention (pdf, 1.87 Mb)

Feature Story
World AIDS Campaign: An opportunity to spark changes in society
24 April 2009
24 April 2009 24 April 2009
(from left) Allyson Leacock, Chair of the Steering Committee of World AIDS Campaign; Michel Sidibé, Exective Director of UNAIDS; Marcel van Soest, Executive Director of The World AIDS Campaign.
Credit: UNAIDS/O. O'Hanlon
AIDS presents a political opportunity to spark changes in society and talk about issues like human rights, homophobia and sex education according to UNAIDS Executive Director Michel Sidibé.
"You will never make a difference if you look at AIDS in isolation," Mr Sidibé said during his first meeting with the head of the World AIDS Campaign in Geneva.
Executive Director of The World AIDS Campaign Marcel van Soest said, “AIDS is a disaster beyond a health issue, it’s a human rights issue too.”
AIDS is a disaster beyond a health issue, it’s a human rights issue too.
Marcel van Soest, Executive Director of the World AIDS Campaign
International representatives from a wide range of communities including The Global Network of People Living with HIV/AIDS (GNP+) and The Global Unions AIDS Programme attended the meeting.
UNAIDS and the World AIDS Campaign reaffirmed their intention to put human rights and universal access to treatment, prevention, care and support at the centre of their campaigning agendas.
In addition to talks on how to help guarantee continuation of treatment, and to stop discrimination against people living with HIV participants looked at ways to invigorate campaigning at local and national levels.
The 2009 World AIDS Day Campaign will be unveiled in Nairobi, Kenya early in June.
Right Hand Content
Partners:

Feature Story
Official launch of the V Latin American and Caribbean Forum on HIV/AIDS and STDs
24 April 2009
24 April 2009 24 April 2009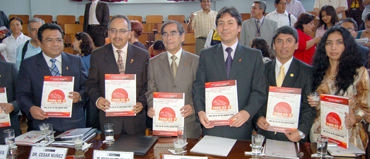 (L to R): Dr Jose Luis Sebastian Mesones, Technical Secretariat of the Horizontal Technical Cooperation Group and National AIDS Coordinator from Peru, UNAIDS Regional Director for Latin America, César Antonio Núñez, Minister of Health of Peru, Dr Oscar Raúl Ugarte Ubilluz, Minister of Labour, Jorge Elisban Villasante Aranibar, Director of Health Services of Peru, Dr Edward Cruz Sánchez and Mrs. Guiselly Flores Arroyo, representing the Latin American network of people living with HIV.
(L to R): Dr Jose Luis Sebastian Mesones, Technical Secretariat of the Horizontal Technical Cooperation Group and National AIDS Coordinator from Peru, UNAIDS Regional Director for Latin America, César Antonio Núñez, Minister of Health of Peru, Dr Oscar Raúl Ugarte Ubilluz, Minister of Labour, Jorge Elisban Villasante Aranibar, Director of Health Services of Peru, Dr Edward Cruz Sánchez and Mrs. Guiselly Flores Arroyo, representing the Latin American network of people living with HIV.Credit: Ministry of Health of Peru/J.E.Castro Varillas
The V Latin American and Caribbean Forum on HIV/AIDS and STD’s, FORO 2009 was officially announced on Thursday 16th April in Lima. The Forum will take place in Peru’s capital from 22nd to 26th June under the theme “Health is our right, universal access is our goal, no discrimination our challenge”.
FORO 2009 was officially launched by the Minister of Health of Peru, Dr Oscar Raúl Ugarte Ubilluz together with the Minister of Labour, Jorge Elisban Villasante Aranibar, Director of Health Services of Peru, Dr Edward Cruz Sánchez, UNAIDS Regional Director for Latin America, César Antonio Núñez, Mrs. Guiselly Flores Arroyo, representing the Latin American network of people living with HIV, and Dr Jose Luis Sebastian Mesones, Technical Secretariat of the Horizontal Technical Cooperation Group and National AIDS Coordinator from Peru.
Health Minister Ugarte invited all stakeholders working in Latin America and the Caribbean to come to Lima and engage in an open discussion about universal access to HIV prevention, treatment, care and support in the region and single out the gaps in the response. This was reinforced by Labour Minister Villasante, who also raised the importance of reducing stigma and discrimination in the workplace in particular.
During the launch, UNAIDS Regional Director for Latin America, César Antonio Núñez stressed that FORO 2009 “offers an opportunity to governments and civil society to review progress made in the region towards universal access to HIV prevention, treatment, care and support under a human rights perspective.”
Dr Núñez pointed out to the audience that there are close to 500 new HIV infections in the region every day and highlighted the urgency to prioritize HIV prevention efforts as well as the need to reject all forms of stigma and discrimination against people living with HIV and people most at risk of HIV infection.
The main objective of the forum is to promote coordinated national and regional efforts to achieve universal access to HIV prevention, treatment, care and support in the region. The meeting will also serve as a platform to share lessons learned to improve practices on HIV interventions, prevention, research and access to information.
Furthermore, the meeting will review the response to AIDS through analysis of progress made in the fulfilment of the International HIV commitments made by governments in the region. The forum will highlight recent successes, as well as outlining the challenges faced in the region and ways to overcome them. Finally, it will promote the greater participation of all the social actors in response to the epidemic.
Some 4,000 people are expected to attend this year’s Latin American and Caribbean Forum on HIV/AIDS and STD’s. Participants will include people living with HIV, civil society groups, non-governmental and governmental institutions, academia, the media, UN agency representatives and the private sector.
Official launch of the V Latin American and Carib
External links:

Feature Story
New Country Response Information System to strengthen national M&E
24 April 2009
24 April 2009 24 April 2009
UNAIDS announces the launch of the Country Response Information System (CRIS) version 3, which is a tool for managing national HIV data. In support of Three Ones principles, and especially the principle of one national monitoring and evaluation system, CRIS3 enables national AIDS authorities to store, share and utilize the national HIV data in an effective manner with national and international counterparts.
The new released version brings improved features for monitoring national programmes and progress towards set national targets, such as those of universal access. Version 3 is more flexible and adaptable to meet the requirements of individual countries, using internationally agreed standards for HIV monitoring and evaluation.
Some of the main highlights of CRIS3 include:
- Ability to import indicators from the Indicator Registry, and flexibility in indicator data entry;
- Intuitive and clear user interface, reducing need for user training and time needed for use;
- Options of using CRIS3 either via web in countries with good internet access, or as a standalone application in settings with limited connectivity with data exchange between systems; and
- Improved technical and user support for national installations and configuration.
Supporting national HIV databases
As one of its mandates, UNAIDS provides guidance and develops tools for countries to better plan and manage their national monitoring and evaluation (M&E) system. Two of the most relevant tools recently developed by UNAIDS to facilitate the monitoring and evaluation of national HIV responses are the Indicator Registry (repository of standardized set of internationally agreed indicators) and CRIS3 (tool for monitoring national response to AIDS). Used together they complement each other as countries can use the indicator registry to select standardized indicators for their national monitoring purposes and use them in CRIS3 for data collection, storing, analysis and reporting.
CRIS3 has been developed with country needs in mind, emphasizing advanced programmatic features for national programme monitoring, including multiple monitoring plans that can accommodate the reporting needs of different donors, such as The Global Fund to fight AIDS, Tuberculosis and Malaria, the United States President’s Emergency Plan for AIDS Relief (PEPFAR) and others.
CRIS3 is at its best for use of national and district M&E officers as they have various backgrounds and skills to use different M&E tools. UNAIDS supports capacity building in M&E skills through different means, such as M&E trainings and CRIS specific trainings. Regional training events are organized during 2009 and the UNAIDS Country Monitoring systems team can be contacted for further details.
For more information on CRIS3 you may visit the support web-site: www.cris3.org or contact the Country Monitoring Systems team: cris@unaids.org
Mr. Taavi Erkkola (erkkolat@unaids.org).