
Feature Story
Innovative WFP electronic voucher programme in Zimbabwe brings relief to many living with HIV
27 April 2012
27 April 2012 27 April 2012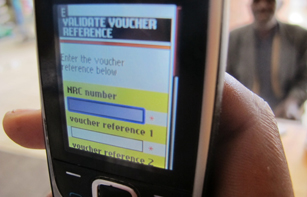
In Harare and Bulawayo, people living with HIV receive vouchers from WFP that entitle them to a month’s supply of household food items, to be collected from one of a number of local shops.
Credit: WFP
Loveness and her three children, Robert, Susan and Julia, share a room at the back of a garage in Zimbabwe’s second city, Bulawayo. All of them are living with HIV and Loveness struggles to make ends meet and to provide the family with enough food. In the past she would often go hungry herself to ensure that her children could eat a meal, often just three spoonfuls of plain porridge each.
However, Loveness and her family are looking towards a brighter future with the help of the World Food Programme (WFP). The UN body is using an innovative intervention involving electronic vouchers to provide nutritional support to chronically ill, food insecure households, many of whom are living with HIV, in Harare and Bulawayo.
An estimated 14.3% of adults, some 1.2 million people, are living with the virus in Zimbabwe and there are around 150 000 children living with HIV.
Challenging malnutrition
Under the programme implemented by WFP through cooperating NGOs and the Ministry of Health and Child Welfare, clients visiting local clinics and hospitals found to be malnourished are referred to WFP food and voucher distribution points in their vicinity where they are given SuperCereal. This is a highly nutritious fortified blend of maize meal, soy protein and micronutrients. (Malnutrition is gauged by body mass index in adults and upper arm circumference measurement in children).
They also receive an electronic voucher to buy pre-determined food, such as oil and beans, at selected supermarkets. The e-voucher's value depends on family size and when presented with a voucher, the shop assistant contacts an electronic database to verify the ration for a month’s supply.
The cash vouchers are an alternative to in-kind food assistance and WFP uses them to tackle hunger where food is available in the market place but where most people cannot afford to buy it.
A holistic approach
For those living with HIV, such as Loveness and her family, the WFP’s nutritional support forms part of a holistic approach. One important element of the programme is to encourage beneficiaries to have a medical check up once a month at a clinic or hospital in their area. The Ministry of Health and Child Welfare works closely with the WFP and provides free antiretroviral therapy (ART) when necessary. Loveness’ children are all on such medication.
The food assistance helps me because the children get enough at each meal and the little money I’ve been spending on food I can now spend on school fees
Loveness, e-voucher recipient
Food assistance not only increases the effectiveness of ART but also helps ensure greater adherence to treatment regimens. Good nutrition is essential in protecting people living with HIV and, according to WFP, the virus, malnutrition and food insecurity are inextricably linked. When people living with HIV are malnourished the risk of death increases significantly. Although people living with HIV need more calories and nutrients than people living without the virus, they often have lower appetites and are less able to absorb nutrients.
Expanding the programme
The voucher scheme supports around 8 000 clients and their families. WFP Country Director Felix Bamezon is pleased with the success of the scheme in Harare and Bulawayo and wants others areas to reap the benefits: “WFP plans to expand the e-voucher component of the programme to other cities and towns where possible."
According to Loveness, it has made a real difference, “The food assistance helps me because the children get enough at each meal and the little money I’ve been spending on food I can now spend on school fees.”
WFP is the largest humanitarian agency fighting hunger worldwide. It feeds more than 90 million people in over 70 countries every year. In 2010, WFP supported 2.5 million beneficiaries in nearly 50 countries through its HIV and Tuberculosis (TB) programmes. This included food and nutritional support to some 500,000 people living with HIV as part of their antiretroviral therapy or TB treatment.
Related

Feature Story
People living with HIV in Ethiopia receive vital nutrition boost
18 October 2011
18 October 2011 18 October 2011
Credit: UNAIDS/P.Virot
Men, women and children on HIV treatment in drought-affected Ethiopia will benefit from a US$ 56 million donation from the US President’s Emergency Plan for AIDS Relief (PEPFAR) to the World Food Programme (WFP).
The donation will allow the UN agency to increase vital nutritional support to people on HIV treatment—who are often already weakened by malnutrition—and their families. Spread over five years, it is the largest contribution ever made from PEPFAR to WFP.
Welcoming the donation, Josette Sheeran, WFP Executive Director emphasized that the provision of the right nutritional support for people on HIV treatment “can make the difference between life and death. Because when malnourished people do not have the right food to eat, treatment does not work.” She added that WFP would now be able to reach more people; assisting families affected by AIDS with sustainable food security and helping to eliminate new HIV infections among children and keep their mothers alive.
Supporting children living with HIV by helping ensure good nutrition is a key concern which echoes the WFP’s new global initiative to mark World Food Day: ‘Feed a child, feed a dream’. Through an online platform, the initiative highlights the aspirations of some of the many children being supported by WFP around the world and how they can be met.
WFP will now expand its areas of operation into the country’s least developed regions of Afar, Benishangul Gumuz, Somali and Gambella to improve the nutritional status, treatment success and quality of life of people on HIV treatment and their families.
At present WFP supports HIV treatment in urban areas, including assessments, counselling and food assistance for those who are malnourished. From 2008 to 2010, an estimated 355 000 people living in households affected by AIDS in 23 towns benefited from these activities. With PEPFAR’s donation, WFP can reach an additional 375 000 people living in households affected by AIDS—those that are most vulnerable to malnutrition and food insecurity—over the next five years.
The entry criterion for the receipt of food aid is the nutritional status of the individuals as measured by body mass index for example. All people on antiretroviral therapy (ART) receive nutrition education and counselling, and only those who are malnourished will receive food rations for a period of six months. Experience has shown that nutritional recovery (>85% weight for height) occurs rapidly when ART is combined with food assistance.
Food and nutrition assistance is an essential and cost-effective means of enhancing the success of antiretroviral treatment (ART), enabling nutritional recovery and mitigating the socio-economic consequences of HIV and tuberculosis. Furthermore, this type of assistance increases the likelihood that patients will adhere to treatment, thereby reducing the likelihood that additional, more costly treatments will need to be found.
WFP is the largest humanitarian agency fighting hunger worldwide. It feeds more than 90 million people in over 70 countries every year. In 2010, WFP supported 2.5 million beneficiaries in nearly 50 countries through its HIV and Tuberculosis (TB) programmes. This included food and nutritional support to some 500,000 people living with HIV as part of their antiretroviral therapy or TB treatment.
External links
Publications
Related
 The Breaking Point: A Story from Ethiopia
The Breaking Point: A Story from Ethiopia

06 May 2025
 Impact of US funding cuts on HIV programmes in Uganda
Impact of US funding cuts on HIV programmes in Uganda

19 March 2025

Feature Story
Horn of Africa in crisis: famine, displacement and HIV
20 September 2011
20 September 2011 20 September 2011
Credit: UNAIDS/P.Virot
The ongoing drought and famine in the Horn of Africa has put the lives of millions of people in Somalia, Kenya, Djibouti and Ethiopia at serious risk. An estimated 13 million people in the region are in urgent need of humanitarian assistance, including food and medical care.
Central and southern Somalia are the areas hardest-hit in the region, where protracted civil conflicts, weak state structures and limited access to humanitarian assistance pose a complex set of challenges. According to the United Nations High Commissioner for Refugees (UNHCR), there are more than 800 000 Somali refugees in the Horn of Africa, of whom over 250 000 have fled to Kenya, Ethiopia and Djibouti since January 2011.
HIV in emergency settings
While HIV data in central and southern Somalia is scarce, experience and evidence have shown that people in emergency settings tend to have limited access to HIV prevention, treatment, care and support. The health of people living with HIV is put at further risk when their nutritional needs are not met. Displacement, loss of livelihood and increased sexual violence can pose additional risks of HIV infection.
An estimated 3 million Kenyans—among them approximately 90 000 people living with HIV—are affected by drought and food insecurity, especially in the semi-arid regions of northern Kenya. Most HIV services in the country are currently functioning, and treatment interruption is still low. However, the Joint United Nations Programme on HIV/AIDS (UNAIDS) and partners fear this situation may change as community-level interventions and nutritional support for people living with HIV are increasingly interrupted.
In recent weeks, many people in northern Kenya have moved to the slums of Nairobi, seeking a means to survive. City dwellers have faced a doubling of prices for key staple foods. The risk of unprotected transactional sex (or “food for sex”) is rising and could lead to an increase in the number of new HIV infections.
“If HIV-related vulnerabilities are not considered in emergencies, Kenya’s rallying call of an ‘HIV Free Society’ remains a far fetched dream,” said Prof. Alloys S. S. Orago, Director of Kenya’s National AIDS Control Council. “Reducing the vulnerability of people living with HIV in emergency situations requires the effective engagement of all stakeholders,” he added.
Response by UNAIDS and partners
Together with the World Food Programme (WFP) and UNHCR, the UNAIDS Secretariat and other Cosponsors have warned of the urgent need to provide HIV services to emergency-affected populations across the region.
In collaboration with regional partners and national authorities, the UNAIDS family has been working to assess the impact of the current crisis on the HIV epidemic and the related needs of affected populations across the Horn of Africa. This data is being used to effectively integrate HIV in the humanitarian response across the region.
If HIV-related vulnerabilities are not considered in emergencies, Kenya’s rallying call of an ‘HIV Free Society’ remains a far fetched dream
Professor Alloys S. S. Orago, Director of Kenya’s National AIDS Control Council
Many Somalis have fled to a refugee camp in Dadaab, northern Kenya, where comprehensive reproductive health and HIV services are available, including emergency obstetric care, HIV prevention services and the provision of antiretroviral treatment. All camp hospitals provide services for survivors of sexual violence, such as post exposure prophylaxis for HIV prevention, contraception and psychosocial support.
In Kenya, the UN family is collaborating with the national government and non-governmental organizations (NGOs) to ensure that HIV services are available in emergency-affected areas. UNHCR is conducting baseline surveys in the refugee camps and WFP is providing data on nutrition and HIV for the north and north eastern provinces, where drought-affected local populations also require continued HIV prevention, treatment, and care and support services.
In Ethiopia, UNHCR and partners—including more than 10 international NGOs—are working in refugee camps to reduce the transmission of HIV, prevent sexual violence, and provide care for survivors of sexual violence. From the start of the emergency, blood safety measures have been reinforced and male condoms have been made available. For people living with HIV, a national antiretroviral protocol is followed, including CD 4 testing, clinical monitoring and the promotion of treatment adherence.
As part of a wider continental response, the African Union (AU) recently pledged more than US $350 million to the humanitarian crisis in the Horn of Africa. At a meeting of AU Ministers and Heads of State on 25 August, all speakers expressed solidarity with affected populations and emphasized the need to tackle both the current crisis and underlying root causes, including conflict and climate change.
The UNAIDS family and partners will continue to monitor and respond to HIV needs in the Horn of Africa based on the 2010 IASC guidelines for addressing HIV in humanitarian settings. The HIV response in the region is guided by the UNAIDS vision of Zero new HIV infections, Zero discrimination and Zero AIDS-related deaths.
External links
External links
Publications
Publications
Related

Feature Story
North Star Alliance road show highlights work of its network of mobile clinics along transport corridors in Africa
29 March 2011
29 March 2011 29 March 2011
A 40-foot converted shipping container making its way around European cities is vividly highlighting the work of North Star Alliance. Credit: UNAIDS
A 40-foot converted shipping container making its way around European cities is vividly highlighting the work of North Star Alliance. This public-private partnership is committed to building a network of roadside clinics at transport ‘hotspots’ in Africa to provide long-haul truck drivers, sex workers and surrounding communities with access to basic health care.
This week the North Star Alliance road show, with its container-based model wellness centre, arrived in Geneva. UNAIDS and World Health Organization staff were able to see for themselves exactly how these centres operate. Many took advantage of the opportunity to receive free medical checks, including blood pressure testing.
From HIV prevention to antihistamines
This is one of the best public-private partnerships I’ve seen. It works well. Each partner brings specialist expertise and knowledge to make a strong and cohesive intervention that’s really making a difference
Robin Jackson, UNAIDS’ representative on the board of North Star
The broad range of services on offer in a typical wellness centre includes condom distribution, treatment for sexually transmitted infections, information on HIV prevention and nutrition, basic eye tests, malaria treatment and even getting antihistamines for the common cold. Most centres also offer HIV counselling and testing and access to a behaviour change communication specialist. North Star is planning to expand its services to include greater support for antiretroviral therapy and tuberculosis screening.
There are now 22 wellness centres in 10 countries in east and southern Africa. By the end of 2014 there will be 100 such centres covering 85% of the major transport corridors on the continent.
In the field, the shipping containers are placed at border posts or transit towns where truckers congregate and are open late, when drivers have parked for the night and sex work tends to take place. In general mobile workers, who often have to spend long periods away from their families, may have multiple partners and use the services of sex workers.
A model partnership

A broad range of services are on offer including condom distribution, treatment for sexually transmitted infections, information on HIV prevention and nutrition, basic eye tests, and malaria treatment. Credit: UNAIDS
North Star Alliance is an independent non-governmental organization, supported by five core partners: the express distribution company TNT, the International Transport Workers’ Federation, the World Food Programme, UNAIDS and ORTEC, a large provider of logistics software. It is seen as a model of public-private partnership.
According to Robin Jackson, UNAIDS’ representative on the board of North Star; “This is one of the best public-private partnerships I’ve seen. It works well. Each partner brings specialist expertise and knowledge to make a strong and cohesive intervention that’s really making a difference. ”
External links
Related

Feature Story
Investment in health is an investment in economic development
29 March 2011
29 March 2011 29 March 2011
(from left) Advocate Bience Gawanas, Commissioner of Social Affairs at the AUC, Addis Ababa, Ethiopia; Mr Robert Joseph Mettu Mumoo, Deputy Minister of Health Ghana; Mr Modoul Diagne Fada, Minister of Health and Prevention, Senegal; Mr Michel Sidibé, UNAIDS Executive director; Mr Essimi Menye Lazare, Minister of Finance, Yaoundé, Cameroon. Credit: UNAIDS
African Ministers of Finance and Health came together in Addis Ababa on 29 March 2011 for a high level panel discussion to explore new ways of investing in health.
The panel, entitled More health for money and more money for health, was part of the 4th Joint Annual Meetings of the African Union Conference of Ministers of Economy and Finance and ECA Conference of African Ministers of Finance, Planning and Economic Development.
The discussion aimed to foster dialogue on health financing to improve health outcomes to help accelerate achievement of the health-related Millennium Development Goals. Ministers of Finance and Economic Development from Sierra Leone and Cameroon joined Ministers of Health from Ghana and Senegal as well as the Executive Directors of UNAIDS and UNFPA.
“Investing in AIDS is not only the right thing to do, but the smart thing to do,” said UNAIDS Executive Director Michel Sidibé. “Thanks to smart investments, more than four million Africans now benefit from HIV treatment, living resourceful, productive lives and raising solid families,” he continued. “And because we have invested in HIV prevention strategically over the past decade, the rate of new infections has dropped by more than one-quarter in 22 African countries,” he added.
Investing in AIDS is not only the right thing to do, but the smart thing to do. Thanks to smart investments, more than four million Africans now benefit from HIV treatment, living resourceful, productive lives and raising solid families
Michel Sidibé, UNAIDS Executive Director
Development assistance to health more than doubled with the emergence of The Global Fund to Fight AIDS, Tuberculosis and Malaria, the Global Alliance for Vaccines and Immunization (GAVI), the Bill & Melinda Gates Foundation and recently, the International Health Partnership. This progress in health financing has contributed to improvements in child health, HIV, tuberculosis and malaria.
While some improvement has been made in health outcomes in parts of the Africa continent, progress is still limited and unequally distributed both among and within countries.
Abuja commitments on health financing not being met
In 2001, African Heads of State and Government made financial commitments towards meeting the Millennium Development Goals by pledging to allocate at least 15% of their national budgets to health. These pledges remain largely unmet, as only six out of 53 African States have achieved the Abuja commitments on health financing.

(from left) Donald Kaberuka, President of African Development Bank and Michel Sidibé, UNAIDS Executive Director. Credit: UNAIDS
Moreover, some 32 of the 53 Africa Union (AU) member States still invest less than half the WHO-recommended US$ 40 per person. Eleven of these countries are investing about US$ 5 per person, an amount too low to tackle diverse health challenges and strengthen health systems.
Participants at the panel discussion concluded that investment in health is an investment in economic development. It was agreed that a key element for sustainable economic development is long-term investment in human, health and social development.
As part of his participation at the conference, Mr Sidibé also met with Mr Donald Kaberuka, President of the African Development Bank. They agreed to explore and support innovative sustainable mechanisms for funding the AIDS response on the African continent.
Related

Feature Story
New framework to eliminate transmission of HIV from mothers to their babies
28 March 2011
28 March 2011 28 March 2011
(from left) Helen Jackson, UNAIDS, Senior HIV Prevention Adviser, ESA; Elhadj As Sy, UNICEF Regional Director for Eastern and Southern Africa (ESA); Tigest Ketsela, Director, Family and Reproductive Health, World Health Organization (WHO), Africa Region; Michael Klaus, Regional Chief of Communication, UNICEF ESARO.
The elimination of mother-to-child transmission of HIV in Eastern and Southern Africa has come a step closer with the endorsement of a new regional framework following a three-day consultation in Nairobi, Kenya earlier this month.
The consultation brought together government representatives from 15 high-burden countries[i], civil society organizations and donors. They were joined by the UN Children’s Fund (UNICEF), the Joint United Nations Programme on HIV/AIDS (UNAIDS), the World Health Organization (WHO) and the UN Population Fund (UNFPA).
In 2009 some 370,000 young children were newly infected with HIV. It was noted that although the scale of the problem of mother-to-child transmission of HIV cannot be underestimated, there is much that can be done. According to Elhadj As Sy, UNICEF Regional Director for Eastern and Southern Africa, “We now have the leadership at all levels to bring this number down. We know what works. Now is the time to act and make a difference. An AIDS-free generation by 2015 is possible.”
Championing both new and existing interventions
Partners endorsed the UNAIDS call for the virtual elimination of mother-to-child transmission of HIV by 2015 and adherence to the new WHO guidelines that recommend giving pregnant women and new mothers a combination of three antiretroviral drugs. They also pledged to vigorously pursue all four components of the internationally agreed UN strategy to dramatically reduce mother-to-child transmission.
There was an acknowledgement that a different approach is needed if the elimination target is to be achieved. A series of priority actions—which include enhanced support for existing programmes and strategies to implement new ones—were defined:
- Improving coverage access and use of services
- Strengthening the quality of existing interventions
- Integrating efforts to prevent mother-to-child transmission into routine antenatal and reproductive health services
- Making paediatric HIV care a routine part of child health services
- Promoting health systems development
- Improving measurement of programme performance and impact assessment
- Engaging communities more fully
The partners also agreed to work on ensuring that all pregnant women and their partners are counselled and tested during their first antenatal care visit.
Room for optimism
If countries continue rapid scale up of quality, comprehensive PMTCT service access, the goal of elimination of HIV transmission from mother to infants by 2015 can be achieved
Helen Jackson, Senior HIV Prevention Advisor for UNAIDS in Eastern and Southern Africa
Although many pregnant women are still falling through the treatment coverage net, in recent years scaled up prevention of vertical transmission efforts have been effective. According to UNAIDS 2010 estimates, in southern Africa in 2009 an estimated 130,000 infants were newly infected, more than 30% fewer than in 2004. In Botswana, Namibia, South Africa and Swaziland treatment coverage has reached more than 80%[ii]. Given these figures, and the possibility that they can be achieved across the region, participants in the consultation expressed optimism.
“If countries continue rapid scale up of quality, comprehensive PMTCT service access, the goal of elimination of HIV transmission from mother to infants by 2015 can be achieved,” said Helen Jackson, Senior HIV Prevention Advisor for UNAIDS in Eastern and Southern Africa. “We have joined forces to make sure this happens.”
[i] South Africa, Mozambique, Uganda, United Republic of Tanzania, Kenya, Zambia, Malawi, Zimbabwe, Ethiopia, Angola, Burundi, Lesotho, Botswana, Rwanda, Swaziland and Namibia.
[ii] Ibid
Related

Feature Story
UNAIDS calls better integration of HIV prevention and treatment in maternal, newborn and child health programmes in Ethiopia
30 July 2010
30 July 2010 30 July 2010
UNAIDS Executive Director Mr Michel Sidibé (left) met with H.E. Dr Tedros Adhanom Ghebreyesus, Minister of Health Ethiopia at the Ministry of Health, Addis Ababa, Wednesday 28 July 2010
The Executive Director of UNAIDS, Michel Sidibé paid a visit to Ethiopia to discuss ways of accelerating progress towards achieving universal access to HIV services and reaching the Millennium Development Goals in the country.
High on the agenda was exploring the progress and challenges Ethiopia is facing in preventing mother-to-child HIV transmission (PMTCT).
Mr Sidibé visited the HIV treatment centre and maternity ward at St Paul’s hospital in Addis Ababa where nutritional support is integrated with health service delivery for people living with HIV. While there, Mr Sidibé had an opportunity to participate in the “Mother Support Group Discussions,” a peer support group of HIV positive women who meet fortnightly for psychological support by sharing their experiences and exchanging views on a range of social issues including experiencing stigma, positive living, telling their partners about their HIV status, clinic attendance, and family planning.

UNAIDS Executive Director Mr Michel Sidibé (left) listens to a discussion with PMTCT programme clients at Gulele sub city food distribution centre, Addis Ababa, Wednesday 28 July 2010.
On conclusion of his visit, Mr Sidibé met with the journalists to highlight the need for renewed commitment towards the virtual elimination of mother to child transmission of HIV and the need for innovative approaches to sustain the response.
Mr Sidibé praised the efforts being made by the government of Ethiopia towards eradicating mother-to-child HIV transmission and called on the leadership to intensify efforts to increase access to PMTCT services while addressing the factors undermining access to these services including gender inequality, stigma and discrimination and the insufficient involvement of the community.
Mr Sidibé also urged for enhanced integration of HIV prevention and treatment into maternal, newborn and child health programmes.
Earlier, the UNAIDS executive director had paid a visit to one of the HIV urban projects supported by the World Food Programme (WFP) which provide food and nutritional assistance to pregnant and lactating women living with HIV who are accessing PMTCT services. He met with a group of mothers who participate in this project and commended the initiative which supports lives of mothers and babies through the provision of food and nutritional support.
Related
 The Breaking Point: A Story from Ethiopia
The Breaking Point: A Story from Ethiopia

06 May 2025
 Impact of US funding cuts on HIV programmes in Uganda
Impact of US funding cuts on HIV programmes in Uganda

19 March 2025

Feature Story
WFP Addresses Vital Role of Food and Nutrition in Global AIDS Response
11 August 2009
11 August 2009 11 August 2009
The United Nations World Food Programme (WFP) and its partners explored the vital role of nutrition and food security for people living with HIV during a satellite session at ICAAP09. Credit: WFP/Jim Holmes
During a satellite session at the IX International Congress on AIDS in Asia and the Pacific (ICAAP), held in Bali, Indonesia, the United Nations World Food Programme (WFP) and its partners explored the vital role of nutrition and food security for people living with HIV. Participants examined models of integrating this key area into HIV treatment, care and support, as well as implementation opportunities and challenges.
The widespread recognition of food and nutrition as a critical component of the global AIDS response has come after prolonged advocacy by WFP and others. Optimizing the nutritional status of people living with HIV is a scientifically recognized best practice. Without proper nutrition, people living with HIV become malnourished and treatment is less effective. WFP is placing greater emphasis on the integration of nutritional care in the health sector.
Since each country’s HIV epidemic is different, national AIDS responses need to reflect reality and address the context of unique risks and vulnerabilities. For WFP, the UNAIDS advocacy message, “Know your epidemic, know your response” means that national AIDS responses will include a nutrition and food component when appropriate.
In Asia, there are an estimated 5.0 million people living with HIV. Viral transmission focuses on vulnerable populations susceptible to infection such as sex workers or injecting drug users. In this context, WFP’s action on AIDS reflects the epidemic trend with activities such as the inclusion of mitigation and safety nets for these most at risk populations in national action plans and poverty reduction strategies.
Dr Martin W. Bloem, Head of WFP’s Nutrition and HIV/AIDS Policy, led the satellite session, entitled ‘Models for integrating nutrition and food security into HIV treatment, care and support in the Asia region: Opportunities and challenges’. He was joined by three additional speakers: Professor Emeritus Praphan Phanuphak, Director, Thai Red Cross AIDS Research Centre; Dr Angela Kelly, Team Leader, Papua New Guinea Institute of Medical Research; and Ms Kaniz Fatima, Project Officer and HIV Focal Point, WFP Bangladesh.
They shared their expertise and knowledge on the impact of nutrition and food security for people living with the virus; opportunities and challenges related to nutrition programme design and the development of HIV nutrition guidelines; and priorities for future strategies.
WFP Addresses Vital Role of Food and Nutrition in
IX International Congress on AIDS in Asia and the Pacific
Cosponsors:
Feature stories:
African Union summit focuses on economic growth and food security (02 July 2009)
Swaziland: WFP supports families living with HIV (08 June 2009)
HIV and high food prices (01 April 2009)
The impact of nutrition and HIV: World Food Programme (26 November 2008)
New UNAIDS policy on HIV, food security and nutrition (21 May 2008)
Publications:
UNAIDS Policy Brief – HIV, food security and nutrition (pdf, 244 Kb)
UNAIDS Policy Brief – HIV, food security and nutrition (expanded version) (pdf, 247 Kb)
Related

Feature Story
UNAIDS Cosponsors out in force for 9th ICAAP
09 August 2009
09 August 2009 09 August 2009
The 10 UNAIDS Cosponsors are presenting a strong showing as thousands of delegates converge in Bali, Indonesia, to share ideas, knowledge, best practices, lessons learned and research findings at the 9th International Congress on AIDS in Asia and the Pacific (ICAAP).
The Cosponsors are an integral part of the UN’s response to the global AIDS epidemic and UNAIDS brings together their efforts and resources.
Echoing the Congress theme, ‘Empowering people - strengthening networks’, the Cosponsors are organising and presenting symposia, skills-building workshops and satellite meetings drawing together a number of participants from a range of disciplines with the aim of helping to build and nurture partnerships to bolster the AIDS response in the region.
A number of events are joint Cosponsor initiatives. For example, the Symposium on ‘HIV prevention and most at risk young people’, taking place on 10 August, is sponsored by UNFPA, UNICEF, UNESCO, UNDP, WHO and UNAIDS. The symposium, hosted by the Asia Pacific Regional UN Coordination Group on Most at Risk Young People, is designed to look at the specific needs of this population which is, in general, not being reached by HIV prevention services. This includes injecting drug users, men who have sex with men and sex workers and their clients. Representatives from these groups will also take part in the panel discussion –one further example of how Cosponsor ICAAP activities are designed to involve key populations.
Other examples of Cosponsor activities include UNDP, ILO and UNAIDS (with the Joint United Nations Initiative on Mobility and HIV/AIDS in South East Asia) collaborating on a joint symposium on 12 August entitled, ‘The Impact of the Financial Crisis on Labour Migration and HIV’ in which they will bring their respective expertise to bear on this pressing international issue. UNHCR, along with UNAIDS, is hosting a satellite session on 12 August called ‘Opportunities and challenges in addressing HIV amongst diverse humanitarian populations’. WFP will use a satellite session on 11 August to explore the vital role of nutrition and food security for people living with HIV and will, along with its partners, look at ‘Models for integrating nutrition and food security into HIV care, support and treatment in the Asia Region: Opportunities and challenges’.
The World Bank is also championing the screening, on 10 August, of the film, Suee (Needle) by Cannes Film Festival award winner, Sai Paranjpye, which deals with the lives of injecting drug users and the anti-AIDS stigma they face. The film emerged from the South Asia Region Development Marketplace, a grant programme spearheaded by the Bank and supported by a range of partners including UNAIDS, UNICEF, UNODC and UNDP.
There is an extremely broad range of other Cosponsor activities taking place over the five days of the Congress and a number of these events will be highlighted on the UNAIDS website as the ICAAP progresses.
UNAIDS and its ten Cosponsors work to provide technical support to countries to assist them in the implementation of their national AIDS plans. A ‘division of labour’ guides the technical support provided to enhance coordination, avoid duplication and provide the best assistance available. Each of the Cosponsor organizations leads in at least one technical area. These organizations are:
Office of the United Nations High Commissioner for Refugees (UNHCR)
United Nations Children's Fund (UNICEF)
United Nations Development Programme (UNDP)
United Nations Population Fund (UNFPA)
United Nations Office on Drugs and Crime (UNODC)
International Labour Organization (ILO)
United Nations Educational, Scientific and Cultural Organization (UNESCO)
Related

Feature Story
Swaziland: WFP supports families living with HIV
08 June 2009
08 June 2009 08 June 2009A version of this story was first published at wfp.org

Vusie Maphalala takes part in a joint project run by WFP and Swaziland’s Ministry of Health.
Credit: WFP/Banele Dlamini
Dressed in his smartest suit, Vusie Maphalala waits patiently in the tiny health clinic in Mpolonjeni, located in Swaziland’s capital Mbabane, to collect his life-saving antiretroviral drugs. As a man with HIV, he knows that they are the key to survival – to living long enough to help his three small children grow up.
But he also knows that drugs alone are not enough.
Two years ago, he watched his wife die. She was on HIV treatment but was too weak and too malnourished to thrive. So Mr Maphalala comes each month not just to pick up his drugs but also his food ration which he receives under a joint project run by WFP and Swaziland’s Ministry of Health. Every month he receives more than seven kilogrammes of nutritious corn-soya blend known locally as ‘sidonono’.
Health started improving
“I was malnourished and virtually bedridden when I started getting food from WFP,” said 44-year-old Mr Maphalala, who had been battling to take the drugs on an empty stomach. “But within two months, my health and strength started improving.”
According to Martin Bloem, Chief of the HIV and Nutrition Service at WFP, “Good nutrition is essential in the treatment of HIV particularly in regions where it coincides with widespread malnutrition and tuberculosis. The current economic crisis makes it even harder for people on treatment to stay well fed."
There is no doubt, in Mr Maphalala’s mind, how important the food rations have been. “This area has often been hit by drought and sometimes there was no food, which made it very difficult to keep on taking my medication,” he said, knowing people who have been too hungry to continue their treatment. “But I don’t miss a single dose any more.”
Support to others
Now Mr Maphalala is healthy enough to do manual work and to look after his sons – as well as providing much-needed support to other HIV-positive people in his community who receive antiretroviral therapy (ART).
“As a volunteer, I help people who have recently enrolled in ART to plan their drug schedule,” he said. “I also teach them the importance of nutrition and explain that eating the corn-soya blend will help them stick to that schedule.”
Swaziland has one of the highest levels of HIV in the world. According to latest WHO/UNAIDS/UNICEF estimates, some 26 percent of the adult population is living with the virus. The 2008 Swaziland Country Progress Report states that prevalence among women is 31 percent. Young girls aged 15-24 are disproportionately affected and are nearly four times more likely to be infected than their male counterparts. The demand for treatment has been rising and in 2007 almost 60,000 people were in need of ART, 42% of whom received it.
Nutrition and food security are key components of treatment, care and support for individuals, families and communities affected by HIV, particularly in sub-Saharan Africa. Poor nutrition can hasten the onset of AIDS-related illnesses as well as making it more difficult to stick to ART. HIV also weakens the immune system and can impair food intake and absorption of nutrients. And in fact, those living with the virus need more food than those not infected. Adults with HIV have an energy requirement 10-30% higher than normal. This figure rises to 50-100% in children.
Addressing nutrition and food security is essential if the overarching international commitment to provide universal access to HIV prevention, treatment, care and support services by 2010 is to be met.
WFP implements AIDS programmes in over 50 countries addressing treatment, care and support and impact mitigation.
Swaziland: WFP supports families living with HIV
Cosponsors:
World Food Programme (WFP)
Feature stories:
HIV and high food prices (01 April 2009)
New UNAIDS policy on HIV, food security and nutrition (21 May 2008)
The impact of nutrition and HIV: World Food Programme (26 November 2008)
Publications:
The impact of nutrition and HIV: World Food Programme 26 November 2008 (pdf, 242 Kb.)
Linking Research and Action. Rethinking Food Aid to Fight AIDS (2004) (pdf, 35.3 Kb.)






