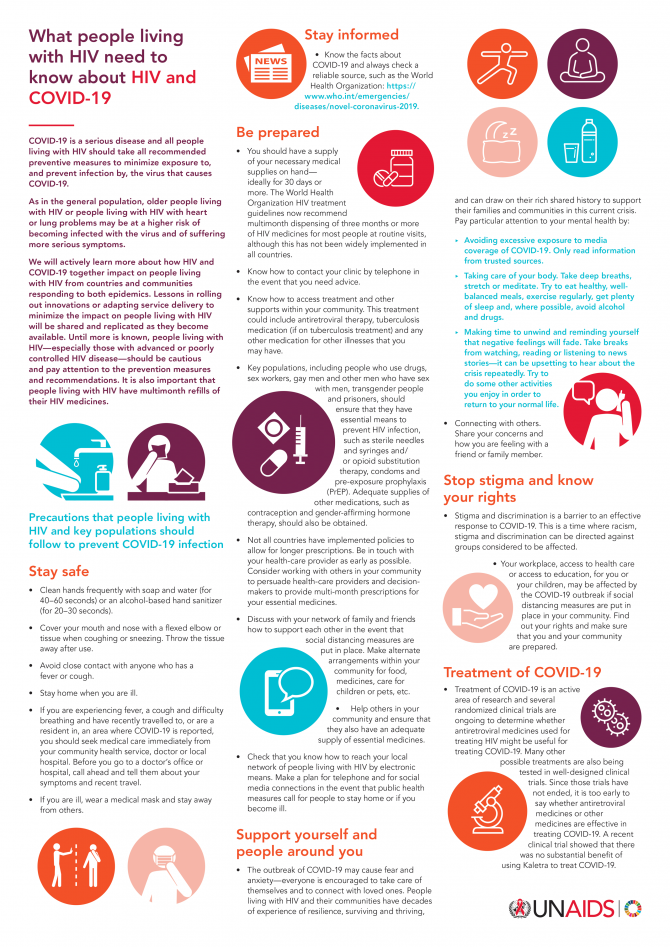
What people living with HIV need to know about HIV and COVID-19
This infographic is also available in Arabic.
01 June 2021
English edition updated June 2021. Data are emerging on the clinical outcomes of COVID-19 among people living with HIV. People living with HIV appear to be at an increased risk of more severe outcomes from COVID-19 compared with other people. People living with HIV should be vaccinated against COVID-19, regardless of their CD4 or viral load, because the potential benefits outweigh the potential risks. People living with HIV should be included in the category of high-risk medical conditions when developing vaccine priority. Importantly, when administering vaccines to people living with HIV, confidentiality about their underlying condition should be preserved.

GENEVA, 20 March 2020—UNAIDS is calling on countries to adopt a human rights-based approach in responding to the global outbreak of COVID-19 that puts communities at the centre and respects the rights and dignity of all. To help guide governments, communities and other stakeholders in planning and implementing measures to contain the pandemic, UNAIDS has produced a new guidance document that draws on key lessons from the response to the HIV epidemic: Rights in the time of COVID-19: lessons from HIV for an effective, community-led response.
The new guidance from UNAIDS is grounded in international human rights law and obligations and makes it clear that responding to an epidemic is not a question of balancing public health and human rights but rather that a successful and effective response requires us to adhere to human rights principles. The guidance has been developed by a group of international experts from communities, the public health arena, academia and the United Nations.
“Successful responses to global epidemics are always grounded in a respect for human rights and community leadership,” said Winnie Byanyima, UNAIDS Executive Director. “Countries that have made the biggest inroads in reducing the impact of HIV have done so by adopting approaches that empower communities to screen, test and seek treatment if necessary and to protect themselves and others from acquiring the virus.”
The guidance presents key lessons from the AIDS response that are crucial for an effective human rights-based approach to public health emergencies. They range from tackling stigma and discrimination faced by affected individuals and communities to prioritizing measures for reaching the most vulnerable, removing human rights barriers, establishing trust between communities and public health authorities and protecting critical frontline medical staff.
As the document recognizes, epidemics tend to expose and exacerbate existing inequalities in society, with their impact often felt most among marginalized and vulnerable groups of people. Financial and other barriers that prevent people from seeking medical help and advice when they need to must be removed, both for their own good and for improved broader public health outcomes.
The guidance also warns against blanket compulsory travel restrictions and criminal sanctions against people affected by epidemics such as COVID-19. Such measures tend to have a disproportionate effect on the most vulnerable and create more barriers to health. Restrictions that are imposed must respect human rights and be necessary, proportionate, evidence-informed and of limited duration. Empowering people to protect themselves and others through voluntary measures can have a greater effect.
“This is a serious and difficult situation for everyone,” said Ms Byanyima, “To come through, we must draw on our valuable experience from responding to other global epidemics, such as HIV: ground the response in human rights, engage communities and leave no one behind.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.

20 March 2020
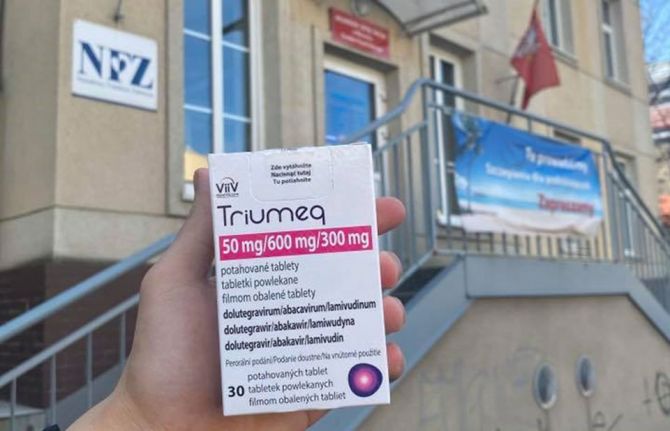
20 March 2020 20 March 2020Getting calls at all hours of the day is not unusual for Liu Jie, the Community Mobilization Officer in the UNAIDS Country Office in China. Because of the COVID-19 outbreak in China, the whole office has been active in helping people living with HIV to continue to access treatment, especially in Hubei Province, where the pandemic was first reported. Recently, Ms Liu was surprised when she had a call from Poland.
"A Chinese man introduced himself, saying he is stranded and will run out of HIV medicine in two days,” Ms Liu said.
With travel restrictions closing down more and more countries, the man could neither return home nor access medicine. Not knowing what to do, he reached out to a Chinese community-based organization, the Birch Forest National Alliance, and through them contacted UNAIDS in Beijing, she explained.
He, like countless other people abroad, was caught in limbo by the fallout from the COVID-19 outbreak. Days earlier, the UNAIDS Country Office in China had helped another Chinese person living with HIV access medicine while stuck in Angola. In both cases, colleagues in Beijing reached out to UNAIDS country offices and the Community Mobilization Team in Geneva, Switzerland. The UNAIDS Country Director for Angola reached out to the Angolan Network of AIDS Service Organisations and the person accessed medicine in no time.
For the case in Poland, Jacek Tyszko, a Polish native and part of the UNAIDS Community Mobilization Team, knew exactly what to do. “Because we have been in touch with regional networks of people living with HIV in central and eastern Europe, I made one call,” Mr Tyszko said.
Anna Marzec-Boguslawska, head of the National AIDS Center in Poland, quickly agreed to follow up. She has always been very responsive, which allows us to move quickly on the ground. Twenty-four hours later, Ms Liu received a photo of a man holding up a box of medicine in front of a grey building. Minutes later her phone rang.
“It was the same Chinese guy calling again from Poland,” she said. “He was crying with joy, saying he had his medicine and that was a picture of him just now.”
She added, “He kept saying how he could not believe that we made the impossible possible.”
The Director of the Birch Forest National Alliance, Bai Hua, also thanked UNAIDS. “This case really reflects that UNAIDS is rooted among the communities,” he said.


24 March 2020
24 March 2020 24 March 2020On the day of China’s Lantern Festival, 8 February, Shen Ming was making sweet dumplings, the traditional festival delicacy, at his home in Wuhan in China’s Hubei Province. From time to time, he would raise his head to watch the local news on the television to get the latest on the COVID-19 outbreak.
His paid particular attention to the new traffic restriction measures. Unlike most people in the city, who stayed indoors all day because of the lockdown, Shen Ming needed to go out almost every day—he is a volunteer who is driving people living with HIV to pick up their medicines from hospitals during the outbreak.
Shen Ming had planned to drive someone to Jinyintan Hospital in the afternoon. Just enough time to have the sweet dumplings, he thought. As the water began to boil, his phone rang. A colleague from the Wuhan Lesbian, Gay, Bisexual and Transgender Center asked him if he could drive another two people to get their medicine right away. He said yes. “You see,” he said. “It will save me a lot of time because I can drive three people to the hospital in one go.”
He switched off the hob and put on a protective suit and mask. “Never mind the sweet dumplings. I can cook them later,” he said. “Besides, I can have a video call with my parents while I’m having the dumplings in the evening.”
A new year away from home
It was more than two weeks since Wuhan, the epicentre of the COVID-19 outbreak, was locked down. An uncomfortable silence hung over the city, which appeared deserted, in stark contrast to the energy of the city before the outbreak.
Shen Ming had had totally different new year plans. He had booked a flight to his home town in Zhejiang Province and had even bought some spicy local delicacies for his parents as new year gifts. “They are more accustomed to sweet food, but I want them to try something different,” he said.
Two days before his flight, Shen Ming got a text message from his boyfriend. “How are you?” the message read. “I got bad news: my father has been diagnosed with COVID-19. And my mother and I both have a high fever too. We are all on the way to the hospital and will stay there if there are beds for us.”
Shen Ming offered his condolescences to his boyfriend, and the next day went to see his doctor. He was relieved to be told that he was not infected, but was advised to stay in Wuhan for observation—he never thought that the coronavirus would be the reason for his first new year away from his family.
So, you are also HIV-positive, like us?
His first passenger was from Shanghai. Wuhan was put under lockdown just as he was about to leave. Soon, he found his HIV medicine running out. “If the medicine of people living with HIV is disrupted, their health will suffer. It might be inaccurate, but I can feel their fear, anxiety and dispair,” Shen Ming said.
Thanks to a directive from China’s National Center for AIDS/STD Control and Prevention, people living with HIV can receive medicine refills wherever they are. All they need is a letter from their service provider. However, they faced a challenge, as taxis and public transport services were stopped during the lockdown.
A survey jointly conducted by UNAIDS and the BaiHuaLin alliance of people living with HIV, a community-based organization in Beijing, shows that nearly 65% of the respondents in Hubei Province had difficulty getting their medicines during the lockdown. With most medical staff concentrating on COVID-19, community-based organization such as the Wuhan Lesbian, Gay, Bisexual and Transgender Center asked for volunteers like Shen Ming to transport people living with HIV to pick up their medicines.
On his first drive, Shen Ming put on three face masks and rolled down the car window to reduce the possibility of getting infected. His trip was to the same hospital that looked after people affected by COVID-19. He was nervous when arriving at the hospital, but to his relief the HIV clinic and the COVID-19 clinic were far apart. The Wuhan Lesbian, Gay, Bisexual and Transgender Center gave him a protective suit after learning that he didn’t have adequate protective equipment, and he eventually became more relaxed.
He would walk to the clinic with his passengers and wait there until they got their medicine. Afterwards, they would have a chat. “So, you are also HIV-positive, like us?” almost all of them would ask Shen Ming. He isn’t. “It doesn’t matter,” he said. “AIDS is just a chronic disease. The care for people living with HIV goes beyond the community of people living with HIV.”
“I will probably stay here”
It was late when he got back home after driving the three people to the hospital on the day of the Lantern Festival. Hungry, he turned on the hob and cooked noodles. This is the first time that Shen Ming hadn’t had sweet dumplings on the Lantern Festival, but he was happy because he got to meet his boyfriend, albeit briefly.
“I will continue my volunteering work until they don’t need me. It would be best if I’m not needed,” he said with a smile on his face.“I will probably stay in this city. I’ll buy a house when the epidemic is over, and build a home here.”
This infographic is also available in Arabic.


12 March 2020
12 March 2020 12 March 2020The COVID-19 outbreak is rightly shining a light on international and national responses to health emergencies—exposing gaps in our systems, showing our strengths and drawing on the valuable experience of responding to other health threats, such as HIV. At UNAIDS, we know that people living with HIV will have some anxiety and questions about the emergence of the virus that causes COVID-19. One of the most important lessons to be drawn from the response to the HIV epidemic is to listen and learn from the people most affected. UNAIDS continues to do so.
It’s important to underline that there is currently no strong evidence that people living with HIV are at an especially increased risk of contracting COVID-19 or, that if they do contract it, they will experience a worse outcome. As in the general population, older people living with HIV or people living with HIV with heart or lung problems may be at a higher risk of getting the virus and of suffering more serious symptoms. As for the general population, people living with HIV should take all recommended preventive measures to minimize exposure and prevent infection. As COVID-19 continues to spread around the world, it will be important for ongoing research in settings with a high prevalence of HIV in the general population to shed more light on the biological and immunological interactions between HIV and the new coronavirus.
But legitimate measures to contain the virus may have unintended adverse effects on people living with HIV. When the COVID-19 outbreak began in China, UNAIDS conducted a survey of people living with HIV to listen to their needs. A follow-up study has shown that some people living with HIV are beginning to experience challenges in receiving medicine refills. This is leading to some anxiety. In response, UNAIDS has been working with networks of people living with HIV and government officials to support special deliveries of medicines to designated pick-up points. A hotline has been established in China so that people living with HIV can continue to express their concerns while the outbreak persists. With our partners, we will also be closely monitoring developments in global supply chains to ensure that essential medical supplies continue to reach the people who need them and that disruptions to the manufacture of active pharmaceutical ingredients are kept to a minimum.
UNAIDS calls upon countries preparing their COVID-19 responses to ensure that people living with HIV have reliable access to their treatment medications. It’s now urgent that countries fully implement current HIV treatment guidelines from the World Health Organization for multimonth dispensing, ensuring that most people living with HIV are given three months or more of their medications. This will help to alleviate the burden on health facilities should COVID-19 arrive and allow people to maintain their treatment regimens uninterrupted without having to risk increased exposure to COVID-19 when retrieving their medicines.
A primary lesson from the AIDS response is that stigma and discrimination is not only wrong but counterproductive, both for an individual’s own health and for public health outcomes in general. That’s why UNAIDS has been supporting campaigns to reduce stigma and discrimination faced by people affected by COVID-19. We have never beaten a health threat through stigma and discrimination and our response to COVID-19 must be guided by lessons learned through the response to HIV. This includes listening to people affected by the outbreak and establishing trust and communication between people affected and health authorities, even before the disease burden rises.
Our biggest gains against HIV have come in countries that have reduced stigma and discrimination, encouraging people to test for the virus and to seek treatment if necessary. Using communication channels recommended by public health experts, let’s listen to people affected by COVID-19 and apply their lived experience so that we can strengthen our response to the virus.
The deaths caused by the COVID-19 outbreak are tragic and my thoughts go out to their families and loved ones. But if we are smart, the international community and individual countries will use this experience to further strengthen monitoring systems and make adequate investments in health infrastructure, both at the global and national levels. UNAIDS urges governments and health officials across the world not to delay in implementing public education programmes for all their citizens about the practical measures that should be taken to curtail the transmission and spread of the virus at the local level.
A people-centred approach is critical. Everyone must have the right to health—it’s our best defence against global epidemics.
Winnie Byanyima, UNAIDS Executive Director


GENEVA, 29 February 2020—UNAIDS welcomes the appointment of Deborah Birx as the White House Coronavirus Response Coordinator. Ms Birx’s distinguished career as a world-renowned medical expert has included her contribution to the recent progress in the global response to HIV and her commitment to working with communities affected by HIV in her position as the United States Global AIDS Coordinator and United States Special Representative for Global Health Diplomacy.
“Vice President Mike Pence’s decision to appoint Deborah Birx to serve as the White House Coronavirus Response Coordinator is a wise one,” said UNAIDS Executive Director Winnie Byanyima. “Ms Birx has repeatedly demonstrated her unparalleled ability to control infectious diseases and is extremely well positioned to develop an effective plan to address COVID-19 in the United States of America.”
Connecting people in need quickly with services that prevent, or treat, the effects of disease requires a specialized skill that Ms Birx has developed over her nearly three decades as a public health expert. Her experience with tackling disease-related stigma and discrimination and her understanding of how to develop effective health responses that deliver results for people will be invaluable in her new role.
"I am confident that Ms Birx will translate the expertise she has applied to HIV to COVID-19,” said Ms Byanyima. “The insights gleaned from the response to HIV can be helpful for the containment of this new viral threat. There is a need for more collaborative work across disease categories. Even as we battle new diseases, we must remain vigilant about concurrent epidemics.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.

GENEVA, 19 February 2020—A survey of people living with HIV has found that the current coronavirus disease outbreak, known as COVID-19, is having a major impact on the lives of people living with HIV in the country.
In the survey, nearly a third (32.6%) of people living with HIV reported that, because of the lockdowns and restrictions on movement in some places in China, they were at risk of running out of their HIV treatment in the coming days—of these, almost half (48.6%) said they didn’t know where to collect their next antiretroviral therapy refill from. However, a close partnership between the government and community partners is determined to ensure that access to life-saving HIV treatment is not interrupted as the country fights to get COVID-19 under control.
The Chinese National Center for AIDS/STD Control and Prevention has directed local authorities to ensure that non-resident people living with HIV can collect their medication wherever they are and has published and disseminated lists of antiretroviral therapy clinics. The UNAIDS China Country Office is working with the BaiHuaLin alliance of people living with HIV and other community partners to urgently reach those people living with HIV who are at risk of running out of their medicines in the next 10–14 days and will offer support as necessary. UNAIDS will also be donating personal protective equipment to civil society organizations serving people living with HIV, hospitals and others to help improve the quality of care for people in health facilities and to prevent coinfection of people living with HIV with COVID-19.
“People living with HIV must continue to get the HIV medicines they need to keep them alive,” said Winnie Byanyima, UNAIDS Executive Director. “I applaud the efforts of the Chinese National Center for AIDS/STD Control and Prevention to support people living with HIV affected by the lockdowns to get their medicines—we must ensure that everyone who needs HIV treatment gets it, no matter where they are.”
The COVID-19 outbreak in China has resulted in an unprecedented response, resulting in hospitals and health-care workers being overwhelmed as they look after COVID-19 patients. Lockdowns in cities have resulted in people living with HIV who had travelled away from their hometowns not being able to get back to where they live and access HIV services, including treatment, from their usual health-care providers.
While the vast majority of the respondents (82%) said that they had the information they need to assess personal risk and take preventive measures against COVID-19, almost 90% said that they wanted more information on specific protective measures for people living with HIV. Similar to the general population, many of the respondents (more than 60%) said that they didn’t have enough personal and household protective equipment, such as face masks, soap or disinfectant, medical alcohol or gloves. Nearly a third reported being anxious and needing psychosocial support during the COVID-19 outbreak.
“We need to know how many people living with HIV are contracting COVID-19, whether people living with HIV are at greater risk of contracting COVID-19 and, if they contract it, whether they are in greater danger from it—at this stage of the COVID-19 outbreak there are so many unknowns. We must fill in the gaps in our knowledge, and fill those gaps in rapidly,” added Ms Byanyima.
The survey was devised and launched jointly by UNAIDS and the BaiHuaLin alliance of people living with HIV, with the support of the Chinese National Center for AIDS/STD Control and Prevention. UNAIDS mobilized community support for the survey and promoted the survey online in order to maximize the responses to it—more than 1000 people living with HIV replied. Responses were collected from 5 to 10 February 2020. A follow-up in-depth survey is to be carried out in partnership with the School of Medicine at Zhongshan University, which will go beyond community needs and will look at health systems issues that have a direct impact on HIV services.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.