



Feature Story
HIV community activists tackle COVID-19 in Lesotho
02 December 2020
02 December 2020 02 December 2020It is a sunny weekday morning in the small town of Morija, Lesotho. On the expansive lawn of the Morija Museum and Archives, under the shade of tall trees, a group of children and teenagers sit on evenly spaced plastic chairs.
They have all had their temperatures checked, have washed their hands at purpose-built tippy-taps and are wearing brightly coloured seshoeshoe fabric face masks.
The learners would usually be in school at this time, but schools throughout the country remain closed due to COVID-19. In response to this crisis, local community-based organizations have had to implement new and innovative programming.
This particular programme is called Skills & Soup, implemented by the Hub, a Morija-based nongovernmental organization. On a bi-weekly basis, groups of learners visit to receive a nutritious meal and participate in a range of activities and educational programming, including dance and taekwondo, maths and science lessons and COVID-19 awareness sessions.
Today, the Hub is hosting a pair of guest facilitators from the Maseru-based nongovernmental organization Kick4Life, which specializes in delivering HIV and life skills education through sports-based curricula.
Puky Ramokoatsi, an experienced educator and gender equality activist, is leading the session with confidence and ease. She begins with an energizer, getting the learners to stand up to chant and dance along with her, all the while remaining at a two-metre distance from one another. She keeps her mask on throughout the session, the volume and authority of her voice unhindered.
During the session, Ms Ramokoatsi and her co-facilitator, Mbulelo Mochochoko, play a series of sound clips from a portable speaker. The clips, taken from new animations developed by Kick4Life, feature catchy music and short conversations between two characters who discuss a range of health-related topics, including HIV, nutrition, mental health and ways to protect oneself against COVID-19.
“Who can remind me which fluids can transmit HIV?” asks Ms Ramokoatsi after one of the clips has played. The children stand up and stretch their hands out eagerly, competing to be the first to give the correct answer.
The session is a far cry from Kick4Life’s signature programming, which typically includes close-contact games and activities, with children huddled in groups for discussions or holding hands while standing in a circle.
As with community-based organizations across the region, Kick4Life has adapted its approach to HIV and health education to mitigate the risk of COVID-19 transmission and in response to national lockdowns and government-mandated restrictions.
“We were forced to close our offices in March, when Lesotho went into lockdown, so we had to quickly adjust,” Ms Ramokoatsi explains. “We partnered with the British High Commission in Lesotho to adapt our curriculum into six short animations which could be easily distributed through our online platforms and to include new messaging about COVID-19. We also aired the sound clips from these animations on national radio stations. These are some of the ways that we continued to engage with young people even during the lockdown.”
While COVID-19 cases remain relatively low in Lesotho, at just over 2000 cumulative cases as of November 2020, testing capacity is also low. Only 25 500 tests have been conducted since March 2020. By comparison, a neighbouring country, South Africa, has conducted more tests than this in one day.
In 2019, there were 340 000 people living with HIV in Lesotho, 120 000 of whom are not on HIV treatment.
In addition, a third and silent epidemic plagues Lesotho—that of sexual and gender-based violence. It is estimated that one in three women in Lesotho have experience sexual or physical violence in their life—the same as the global average.
Ms Ramokoatsi has been involved with Kick4Life since 2010, when she began to participate in the organization’s programmes because of her love for football. At the time, she knew very little about HIV, and her interest in the issue was piqued by the fact that her aunt had recently died of AIDS-related illnesses.
“I didn’t understand enough about HIV when my aunt was sick,” recalls Ms Ramokoatsi. “I judged her negatively and didn’t support her. When I learnt more about HIV, I realized how wrong I had been. I made it my purpose after that to support people living with HIV, to give others the support that I hadn’t given my aunt.”
Having experienced sexual abuse herself, Ms Ramokoatsi is acutely aware of the healing power of sports and education and reflects on the difficult transition from face-to-face learning and close-contact activities to virtual and socially distanced programming.
“Before COVID-19 we were in the process of helping several young women who had experienced sexual violence and were slowly opening up to us after taking part in our programmes,” Ms Ramokoatsi explains. “When we were forced to close, we lost touch with some of them. We’ve had to find ways to continue with our programmes and to keep reaching out to our participants, but it hasn’t been easy.”
Ms Ramokoatsi emphasizes the importance of organizations working together in their responses to COVID-19 awareness and health education. “Today, for example, we’re delivering this session thanks to our partnerships,” she says. “I hope more organizations can work like this to share resources and information.”
“I always say that the best part of the game is the opportunity to play. That attitude applies to everything: instead of sitting on the sidelines, get involved. Learn about the situation or the issues around you, whether it’s HIV or gender-based violence or COVID-19. Learn how you can adapt, how you can take care of yourself, and then find a way to help others,” she says.
Our work
Region/country
Related



Feature Story
How the Jamaica transgender community is surviving COVID-19
24 September 2020
24 September 2020 24 September 2020Rose Clark (not her real name) is a 21-year-old transgender woman living in Kingston, Jamaica. Through sex work she’d been able to afford the basics—food, clothes and a small apartment.
Another transgender woman, Carla John (not her real name), worked in a hotel bar on Jamaica’s north coast. It allowed her to live independently of an unsupportive family since she was 19 years old.
COVID-19 upturned their lives. A night-time curfew made it impossible for Ms Clark to work. She was evicted in May. Ms John’s employer shut down operations in April and sent staff home. Since then she’s been living with hostile relatives.
These two are not alone. The Equality Group—a coalition of civil society organizations serving lesbian, gay, bisexual and transgender (LGBT) people in Jamaica—conducted an online survey to gauge the impact of COVID-19 on the LGBT community. It found that a quarter of respondents had lost their job, while three in 10 were unable to pay for food, rent or utilities.
“There’s been a sharp increase in homelessness,” reported Renae Green, Associate Director of Policy and Advocacy at Transwave. “The community has experienced major loss of income and people are unable to pay for housing, food and other basic amenities.”
The transgender community as a whole has several layers of vulnerability—low access to education and employment, small or non-existent family safety nets and high vulnerability to gender-based violence. These are the underlying causes for a 2018 study finding that half (51%) of transgender women in Jamaica were living with HIV.
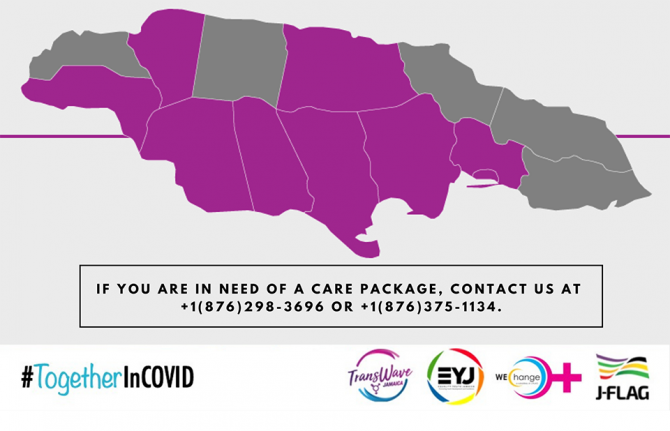
Transwave has collaborated with WE-Change, JFLAG and Equality Youth to run a COVID-19 hotline. It also provided care packages, including non-perishable food items and toiletries, to people in need. Already more than 100 transgender people have benefitted.
Critically, a Trans Emergency Fund was established to raise money to cover or subsidize applicants’ rent for short periods. Both individuals and organizations have made donations. And Transwave manages a virtual support group, providing much needed emotional solidarity during this trying time.
If anything, COVID-19 has intensified Transwave’s ongoing efforts to shine a light on the hidden issues facing one of Jamaica’s most marginalized groups.
“We are not included in decision-making processes,” Ms Green said plainly. “Decision-makers barely talk about us. We keep having to say “remember trans people”.”
UNAIDS Jamaica provided financial support that was used to ensure that Transwave had personal protective equipment and to supplement care package supplies. The office has also made certain that transgender issues are included in the coordinated HIV civil society response to COVID-19.
This fresh pandemic response has unfolded alongside Transwave’s 2020 strategic planning work, which has been supported by UNAIDS and the United Nations Population Fund.
“There is an urgent advocacy agenda for transgender people that includes all the social determinants to health and human rights,” said Manoela Manova, the UNAIDS Country Director for Jamaica.
“COVID-19 has laid bare just how vulnerable people are when they do not have equitable access to opportunities, justice and health care,” added UNAIDS Jamaica’s Community Mobilization Adviser, Ruben Pages. “That’s why it’s so important and inspiring that Transwave has continued its core work through all this.”
Our work
Region/country




Feature Story
“Physical distance, not social distance”: supporting Jamaican women living with HIV during COVID-19
21 September 2020
21 September 2020 21 September 2020The socioeconomic impact of COVID-19 is clear. People have lost incomes. Children are out of school. Food and housing insecurity are on the rise. And there has been an increase in domestic violence.
But for many women living with HIV in Jamaica, there are added layers of stress. According to the Jamaica Community of Positive Women (JCW+), many of their clients reported having received only one month’s supply of HIV treatment, although they were hoping for the recommended three months. New screening protocols at certain clinics have made some people feel exposed to unfamiliar health-care staff and unexpected disclosure of their HIV status. A few women report not having been able to access contraception on time.
According to the Coordinator of JCW+, Olive Edwards, the pressure of dealing with both pandemics has had a huge mental health impact on women living with HIV.
“Uncertainty is taking a toll,” she said. “It has disrupted life and people are worried. Some are struggling to cope with these feelings of constant uncertainty.
JCW+’s main objective for 2020 was to provide community support for women living with HIV in order to improve treatment adherence and reach viral suppression. When COVID-19 hit in March, they were presented with an added challenge. How would they address women’s new needs?
UNAIDS Jamaica’s COVID-19 emergency response contributed hygiene supplies to care packages. JCW+ used these as an entry point for connecting with clients. Women were provided with soap, household disinfectant and bleach and were shown during peer-share sessions how to use those products, along with masks made by a community mobilizer.
From there, the organization linked women to the Positive Health and Dignity Movement and treatment adherence projects. JCW+ participants prepared personal development plans with a focus on treatment adherence, education, job training and certification goals, where necessary. They keep in contact with the care teams in order to ensure access to optimal health and social support services. They have conversations to keep hope alive and send text reminders to reinforce key health and well-being messages.
“Community needs to be engaged at this time. Managing COVID-19 is about physical distance, not social distance. We felt women needed to meet and talk,” Ms Edwards said. They’ve limited support group sessions to eight people at a time.
According to the UNAIDS Country Director for Jamaica, Manoela Manova, the AIDS response must now strike a delicate balance.
“We must address standing health-care and human rights priorities as well as the immediate physical needs triggered by the COVID-19 response,” Ms Manova said.
Going forward, Ms Edwards says JCW+’s advocacy priorities are ensuring that the HIV response is not neglected because of COVID-19 and ensuring the most marginalized people are caught by state social safety nets.
Ms Edwards asked that UNAIDS continue to “feel the pulse of what is taking place” and support community outreach strategies that are relevant to Jamaican culture.
Our work
Region/country





Feature Story
COVID-19 brings Jamaican people living with HIV closer together
18 September 2020
18 September 2020 18 September 2020COVID-19 has brought new challenges for many people living with HIV in Jamaica:
“I am concerned about going to the clinic too often, but I can only get one month’s supply of antiretrovirals at a time.”
“The place I normally go to meet with my community facilitator is no longer available. Now how do I access care?”
“I haven’t been taking my medicines the way I should. Am I going to catch COVID-19?”
For Dane Lewis, Programme Manager of the Jamaica Network of Seropositives (JN+), addressing the community’s anxieties has cleared a path to more connection and support.
“JN+ started doing a survey almost immediately. We reached about 70% of our membership. This was an opportunity to reconnect to our base, to see what the needs were. It helped us to re-establish contact and brought our community closer together,” he said. “Ultimately we think this pandemic will help us bring and keep more people in care.”
There are an estimated 32 000 people living with HIV on the Caribbean island. In 2019, just 44% of them were on antiretroviral therapy, while roughly one third (35%) were virally suppressed. While most people access treatment through the public health-care sector, community organizations like JN+ play a key role in supporting people to start antiretroviral therapy and stay the course.
They’ve also been a critical partner during COVID-19. Despite having a multimonth dispensing policy, the Jamaica Government has authorized just monthly dispensing in order to avoid stock-outs.
“Community organizations like JN+ have allayed fears and followed-up so that people continue their treatment,” said UNAIDS Jamaica Country Director, Manoela Manova. “That’s why it’s important that civil society is at the decision-making table and that community workers are classified as essential workers during COVID-19.”
For the organization’s retention navigators, not much has changed. They continue to reach out to clients via the telephone to check in on whether they are taking their medicines as they should. There has been more of a shift for community facilitators, who were traditionally connected to treatment sites. Face-to-face support has largely given way to telephone calls and video chats. Twice a month, online sessions are used to address wide-ranging community concerns. JN+ team members are on hand to do things like drop off care packages or connect clients affected by community lockdowns to new treatment sites. The organization has also helped people register to receive financial support from the state.
“There has been a lot of anxiety about being able to access basic food and sanitation items. People lost jobs because of the pandemic, so anxieties turned into real needs for many. We had to stop doing in-person activities, such as our support groups, and refocus our energies on coordinating the peers to provide care packages. The support and network we offer have been important,” Mr Lewis explained.
The JN+ COVID-19 experience underlines the key role that community organizations play in helping clients to access resources.
UNAIDS Jamaica has been working to support the response at the practical and tactical levels. It provided hygiene products to be widely distributed and also facilitated weekly collaboration between civil society organizations responding to the needs of people living with HIV during COVID-19.
“Community organizations save lives,” said Ruben Pages, UNAIDS Jamaica’s Community Mobilization Adviser. “The JN+ experience shows why it is important to support community organizations that are able to reach marginalized people with unique support that those in need are not able to find anywhere else.”
Our work
Region/country






Feature Story
Shelter for key populations in Kyrgyzstan
15 September 2020
15 September 2020 15 September 2020Ishenim Nuru, which means “Ray of faith” in Kyrgyz, is a community organization that has been operating in the Chui region of Kyrgyzstan for many years. It started as a group of people living with HIV, their relatives and volunteers and then established itself as a nongovernmental organization that continues to work to fulfil its mission of improving the quality of life of people living with HIV.
Today, Ishenim Nuru provides the only shelter in the area for people in key populations. “With the COVID-19 epidemic, the situation has worsened for many people, but it has become extremely difficult for people released from prison who are living with HIV, people with tuberculosis and representatives of key populations—many of whom were left without a roof over their head and without help. Therefore, we decided to open a shelter,” said Elmira Asanovna Dzhorbaeva, the head of Ishenim Nuru.
The shelter is a place where people can come and receive basic services, where they can sleep, eat and wash clothes, explained Ms Asanovna. “In our shelter, people living with HIV and their family members can get, in addition to basic services, referral to medical institutions. We work closely with city and regional AIDS centres, send clients for viral load tests, provide adherence counselling, engage lawyers, restore documents, provide psychological assistance, and even help with employment,” she added.
Currently, the shelter can accommodate only 10 people at a time, but according to Yuri Malyshev, the shelter’s social worker, when the situation becomes bad sometimes up to 30 people live in the shelter. “We put in additional beds, try to find a way out. People with different destinies live here, some have no documents, some cannot apply for a pension, some have recently been released from prison, and everyone should have a chance. Our main condition is for a person to have a desire to change and adherence to antiretroviral therapy.”
To date, the shelter’s activities are supported by a United Nations Development Programme project, with financial support from UNAIDS. According to Ms Asanovna, the organization is actively discussing the sustainability of the shelter in the face of reduced donor funding amid COVID-19. “We are looking for sponsors, writing projects, we are planning to build our own greenhouse, build a carpentry shop and our own bakery, so that clients have work. Of course, we dream that one day the shelter will have its own property, since we are renting a small house. I really hope that all our dreams will come true.”
Meerim Sarybaeva, UNAIDS Country Manager for Kyrgyzstan, said, “People who need critical support should get it. In the absence of shelters run by the state, this deficiency is being filled by nongovernmental organizations that are mobilizing resources and providing the needed assistance to people during the coronavirus pandemic.”
Our work
Region/country
Related




Feature Story
Cash donations for people who use drugs during COVID-19 in Bangladesh
09 September 2020
09 September 2020 09 September 2020“I cannot provide my family with sufficient food as my earnings have gone down. I feel depressed seeing my family going through economic pain and hunger,” says Kamal Hossain (not his real name), a person who uses drugs who lives in Dhaka, Bangladesh.
The COVID-19 pandemic is affecting the lives and livelihoods of people everywhere. The impact is especially being felt by people who are socioeconomically disadvantaged or marginalized. In Bangladesh, for people who use drugs and who are already struggling with disenfranchisement from the wider community, the hardships they face in making a living and accessing social protection schemes have been exacerbated.
Some of Mr Hossain’s peers worked before the pandemic, but they lost their jobs during the lockdown. Recreation facilities and drop-in-centres where previously they received health and psychosocial support were either closed or only partially operational, and clinical services were disrupted.
To support people who use drugs during the lockdown, UNAIDS made a donation to the Network of People Who Use Drugs (NPUD). With the donation, NPUD provided meals and clothing during the Eid ul-Fitr festival to people who inject drugs and who are living on the street. Food was distributed by members of the local community. For some, this was the only support they had received during the COVID-19 pandemic.
“I received only one meal during the lockdown. I did not receive any government support as I do not have a national identity card. I also received a mask and soap from a civil society organization,” said Rafiq Uddin (not his real name), who is homeless and uses drugs in Dhaka.
Community-based organizations are struggling to support the livelihoods of people from the populations most at risk, including people who use drugs.
“Since NPUD is an organization of people who use drugs, we cannot stay away from this crisis. In this time of difficulty, some leaders of NPUD have come forward to help and UNAIDS’ support has made the first step to make a difference,” said Shahed Ibne Obaed, the President of NPUD.
After receiving the donation from UNAIDS, NPUD reached out to other partners, including CARE Bangladesh, Save the Children (Bangladesh), local humanitarian agencies and volunteer organizations, to provide more comprehensive food support.
“I received some cash from a volunteer organization in my locality. Some of my relatives and well-wishers helped me with food. I also tried to do some income-generating work to support my family, but it was not available on a regular basis,” said Mr Hossain, who is a member of Ashakta Punarbashan Sangstha (APOSH), a community-based organization in Dhaka.
NPUD mobilized enough resources from various sources to continue to support people who inject drugs and people living with HIV in the older parts of Dhaka and beyond. Around 1600 people who use drugs have benefited from the initiative. Coordination between NPUD and other community-based organizations helped to identify beneficiaries. Outreach workers from drop-in centres, APOSH, Prochesta, Old Dhaka Plus, Alor Pothe and others helped to distribute food and clothes. Members of community-based organizations offered their homes as places to prepare and pack food.
NPUD procured personal protective equipment for outreach workers and masks and soap for beneficiaries and set up an online group to share updates and pictures and give information about their activities. The whole initiative was fully voluntary.
“A major concern is the shortage of human and financial resources to support all vulnerable people who use drugs. Wider donor involvement is necessary to generate more funds to support them, especially those who are living on the street, and to ensure sustainability of this initiative,” said Saima Khan, UNAIDS Country Manager in Bangladesh.
Region/country




Feature Story
Guyana’s HIV food bank comes to the rescue during COVID-19
04 September 2020
04 September 2020 04 September 2020For many Guyanese families, COVID-19 has meant far more than mask-use and movement restrictions.
“The disruptive effect on economic activity means that for some there simply is not enough food,” said Michel de Groulard, UNAIDS Country Director, a.i., for Guyana and Suriname.
But for people living with HIV in Guyana, there’s been no need for a hastily improvised nutrition support solution. For almost 14 years the National AIDS Programme secretariat has invested in the development of a food bank specifically for people living with HIV, including those coinfected with tuberculosis.
The programme started with support from the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and continues to receive Global Fund contributions. From the start there were consistent, major donations from the National Milling Company of Guyana. Since 2017, the Government of Guyana and the Food for the Poor charitable organization have been the primary donors. Importantly, throughout the years the food bank has attracted significant inputs from the private sector. In 2019, there were more than 20 corporate contributors.
Referrals come from the clinical teams attending to people living with HIV. Food support is granted for an initial six-month period, after which the situation is reassessed. In the interim there is a collaborative effort with the Ministry of Social Protection and the Recruitment and Manpower Agency around job placement and other types of social support.
Rhonda Moore worked as an HIV doctor for six years and in three regions before assuming leadership of the National AIDS Programme. She’s seen the difference nutrition assistance makes for people and families on the brink. When people are worried about whether they will eat, they don’t take their treatment properly.
“Food insecurity creates a vicious cycle,” she said. “For people living with HIV it is important to have a healthy, balanced diet along with treatment to control the disease. But when someone doesn’t have food it affects them both mentally and physically. Adherence becomes an issue and the mental health impact also undermines the immune system.”
In the context of COVID-19, the food bank has expanded its reach to HIV-negative members of key populations. The National AIDS Programme is collaborating with community organizations to pair dissemination with the provision of information on COVID-19 and HIV as well as HIV prevention and testing services.
So far, more than 2700 food and personal hygiene packages have been distributed. Rather than have people journey to the food bank, the supplies are now being distributed through the treatment sites in their districts. An open invitation was issued to diagnosed people who hadn’t started or continued antiretroviral therapy to go to their nearest treatment centres for HIV medicines and food—two essentials for surviving COVID-19.
In 2019, Guyana became the first Caribbean country to introduce national nutrition and HIV guidelines. The strategy supports health-care providers, policymakers, social workers and other HIV response stakeholders in responding to the nutrition care and support needs of people living with HIV in diverse conditions. In an epidemic response often dominated by concerns around treatment, Guyana has been proactive about addressing the food insecurity challenge some people living with HIV face either consistently or—as is the case with COVID-19—in exceptional circumstances.
“HIV treatment will fail if people don’t have food—healthy food. The fact that Guyana has been able to respond immediately to alleviate food security challenges and thus protect the well-being of people living with HIV right from the outset of the humanitarian crisis demonstrates the value of making psychosocial support investments integral to our regular treatment programme,” Mr de Groulard said. “It makes countries and communities more resilient, more agile and better prepared to respond to crises.”
Region/country




Feature Story
Sex work during COVID-19 in Tanzania
25 August 2020
25 August 2020 25 August 2020“After COVID-19 kicked in, it has been too difficult to get customers,” says Teddy Francis John, a sex worker from Zanzibar. Since the outbreak of COVID-19, she has faced increased difficulties to earn an income to provide for herself and her two children.
“Everything has become tough and I had to start a small business of selling alcohol—local brew,” she says. The business also helps her meet new clients, as they come to her for drinks and are less vigilant about social distancing guidelines.
Ms John used to live and work in Zanzibar town, but to better earn an income and avoid paying rent, she decided to move to a more rural area. Here, she says, she can more easily find new customers for her local brew.
Rehema Peter is facing a similar situation, just on the other side of the ocean on Tanzania Mainland. She lives in the crowded suburb of Temeke in Dar es Salaam and works as a sex worker and volunteers as a peer counsellor for people living with HIV and for people who use drugs.
Her clients were regulars who used to come to her house, or she would visit those she could trust in their homes. But when COVID-19 broke out, they stopped coming.
“Coronavirus made life very hard. Payment at work used to be little and when COVID-19 came it reinforced the situation. On the side of my partners [clients], they stopped visiting and calling me. The very few who used to visit me often, I called them, but they said they have no money because of COVID-19, as some stopped going to their jobs,” says Ms Peter.
At her job as a peer counsellor she was offered fewer shifts, meaning a lower income. Because she is a former drug user, she has received some support through the Tanzania Network for People who Use Drugs (TaNPUD), which has been supported by UNAIDS to distribute food and hygiene items to people who currently use drugs and people in recovery.
“I just try to be calm and find other means [of income]. I’m searching for additional organizations that can help or support me anyhow. I also try to prepare soap and oil from the knowledge that TaNPUD gave me and I sell it,” says Ms Peter.
Continued services
Both Ms Peter and Ms John are living with HIV and are on HIV treatment. Due to the advocacy and assistance of UNAIDS and other partners of the Tanzanian government, disruptions to HIV services have been minimal in the country. This is felt by both women.
“During this time, it has become difficult to get services in government health facilities; unless you go to a private hospital where you must have cash. However, there is no problem at all in getting HIV-related services, including my treatment,” says Ms John.
Ms Peter say she can now get three months multi-month dispensing of antiretroviral treatment—even up to six months—since the healthcare staff do not want congestion in the clinics. This has helped both women in adhering to their treatment.
Increased stigma
Both Ms Peter and Ms John have experienced an in increase in the stigma and social exclusion they also face as sex workers and as women living with HIV during the COVID-19 outbreak.
“As some people know that I am living with HIV, they tease me. They say ‘prepare yourself for death. People like you never heal. You must prepare for your final journey’” recounts Ms Peter. She has faced discrimination in the community, but her family stands by her.
Ms John also faced increased gossip and mocking of her because of her work.
“People in my surrounding communities started mocking me and others. They gossiped as to how I would earn a living as there are not going to be customers because of the COVID-19 outbreak.” Says Francis John
Despite the COVID-19 outbreak being declared over in Tanzania and despite their continued efforts to find other means of livelihood, earning an income is still hard for the two women, due to continued social distancing regulations.
“[It] has been very difficult to provide this service and this harmed us economically. I know COVID-19 has affected the whole world but it has affected sex workers more because of the nature of our services; it involves proximity,” says Ms John.
Our work
Region/country
Related




Feature Story
Guyana community organization serves sex workers on the edge during COVID-19
29 July 2020
29 July 2020 29 July 2020The town of Corriverton in Guyana lies far east, on the Suriname border. Miriam Edwards, the Executive Director of the Guyana Sex Work Coalition, hired a taxi early last Thursday to take her team of peer counsellors there. They planned to conduct welfare checks, offer HIV testing and distribute care packages, masks and condoms as part of a project supported by the Office of the United Nations High Commissioner for Refugees (UNHCR). It’s a nearly 200-mile trip from the capital, Georgetown. Since the COVID-19 outbreak, the regular bus hasn’t been available. Other changes to the flow of life have been devastating for sex workers in Guyana.
“Because of the curfew they are not able to work. Plus the children are home full time. They (the sex workers) can’t make any moves. Some are able to look (work) for money, but in doing so they take more risk. Workshops are not their first priority,” Ms Edwards says plainly. “Their main need is food and sanitization.”
COVID-19 has meant fewer opportunities for work and more competition. A Dominican sex worker reported being attacked by a pair of local women. Her face was swollen and stitched when Ms Edwards got to Corriverton.
One Venezuelan woman ventured out during the curfew. She alleges that police officers in the border town detained her and demanded sex. When she refused, one of them hit her with his gun.
Another Venezuelan sex worker had gone missing since the previous weekend. Her documents and clothes were left in her hotel room, but she still hasn’t turned up.
The complications around sex work in Guyana have deepened since COVID-19. At a time when many locals are out of work, migrants have been particularly affected by joblessness. More of them are exchanging sex for money to survive.
According to a recent Response for Venezuelans (R4V) report by UNHCR and the International Organization for Migration, there have been more reports of sex workers facing eviction or being at risk due to job loss.
“This situation increased their vulnerability of becoming victims of human trafficking, exploitation and gender-based violence,” the report says.
Meanwhile, many Guyanese sex workers have found it difficult to access the social support provided for formal-sector workers by the government.
“The problem is that many in authority don’t see sex work as work,” Ms Edwards said.
But some do. According to Rhonda Moore, Programme Manager at the National AIDS Programme, during COVID-19 the HIV Food Bank has expanded its reach to HIV-negative members of key populations. This includes female, male and transgender sex workers.
Ms Edwards points to the need for even more targeted social support, including for single mothers, migrants and those working in the interior.
The Guyana Sex Work Coalition’s strategy has been to pair the distribution of nutrition support and hygiene supplies with offers of HIV testing and safety reminders on COVID-19, HIV and sexually transmitted infections. According to Ms Edwards, this is a time of high stress and uncertainty and her clients are not necessarily able to absorb mass media messages. Text reminders and phone calls have been key approaches to ensuring that individual sex workers are informed and to address their unique challenges. Sometimes they need medication or money for transport. Many of the migrants need a safe space.
UNAIDS is embarking on a project with the Caribbean Sex Work Coalition to help national networks address sex workers’ knowledge, HIV prevention and social support needs during COVID-19. A major goal of the project is region-wide advocacy to encourage Caribbean governments to include sex workers in their planning and protection.
“Sex workers need to be included in national social protection schemes and many of them need emergency financial support,” said James Guwani, Director of the UNAIDS Caribbean Sub-Regional Office. “To win the battle against COVID-19 or HIV, we must give life to the principle of leaving no one behind.”




Feature Story
Fostering an economy of kindness through traditional bartering in Fiji
17 July 2020
17 July 2020 17 July 2020On an early Fijian morning, Marlene Dutta, coffee cup in hand, is sitting on her back deck surrounded by greenery. Not even the sound of birds in the background can peel her away from her computer screen. She is busy sorting through messages and reviewing the activity on the Facebook page that she created, Barter for Better Fiji, an online community that has revitalized Fiji’s traditional bartering practices and helped communities sustain themselves during the COVID-19 outbreak.
“From the minute myself and the other volunteer administrators of the page wake up, our eyes are on the page”, said Ms Dutta, a business skills development consultant. They are busy monitoring or sharing information from the government about restrictions on items to barter.
In Fiji, where approximately 30% of the country’s gross domestic product comes from tourism, travel restrictions to prevent the spread of COVID-19 have brought about tough times for many.
Reflecting on how she came up with the idea for the Facebook page, Ms Dutta said, “Bartering has always been something that Fijians rely on in their daily lives, amongst their friends, families, amongst communities. We all have a skill, a talent, something that we can grow, a whole host of things stuffed away in our houses. If people could trade items or services to get what they needed, then they may be able to sustain themselves through this time.” From these thoughts, Barter for Better Fiji was born. Ms Dutta is astounded by how popular the page has become. Initially envisioned to only be used by her friends, the page now has a following of more than 180 000 members—a huge amount considering that the country has a population of only around 900 000 people—and thousands of requests for new memberships arrive daily.
Aside from helping members to barter for necessary food or services, or sustaining small businesses by linking them to new suppliers for their trade, the page is also creating a greater sense of community. Members have been able to reconnect with long-lost neighbours, family members and childhood friends. Ms Dutta recounts stories of complete strangers meeting on the page to barter only to find that they are neighbours on the same street or have traditional ties.
“Through the page we hope to foster an economy of kindness. That is behind everything that happens on the page,” explained Ms Dutta. “That in itself has brought this sense of community where people are being purposefully and intentionally kind, compassionate and merciful to each other.”
While the Barter for Better Fiji Facebook page doesn’t specifically target the needs of vulnerable groups or people living with HIV, groups such as the Fiji Network for People Living with HIV, the Rainbow Pride Foundation and the Survival Advocacy Network Fiji have reported that their community members have benefited from the online bartering platform. The page has made bartering the “new normal” for vulnerable groups.
“Whether LGBTQI+ or not, we are all humans at the end of the day, and we need to support each other one way or the other. That’s why I think having such a page is a wonderful initiative,” said one member of the Rainbow Pride Foundation.
Community members have been able to barter items or provide cleaning services in exchange for groceries, while others point to how money saved through bartering has allowed them to venture into other income-generating activities, like backyard vegetable gardens and food stalls. At a time when tourism has seen a decline, some groups, such as sex workers, have found their sources of income vanish.
Lesbian, gay, bisexual, transgender and intersex community members have also faced stigma due to false understandings about how the new coronavirus is spread. Yet members of those groups have proclaimed how the uplifting stories and connections developed among members of the Facebook page have helped them to cope and have positively affected their mental health. It is because of these positive stories, stories of communities coming together to cope with the COVID-19 pandemic, that Barter for Better Fiji is interested in expanding the Facebook page to a website and app.
As Fiji grapples with moving beyond the COVID-19 outbreak, Barter for Better Fiji recognizes its important role in what lies ahead, how that it is more than a platform for bartering but also a space to share heart-warming stories of connection that promote an economy of kindness.
















