Feature Story
Putting condoms on the Fast-Track as an efficient and cost-effective HIV prevention method
03 October 2016
03 October 2016 03 October 2016The UNAIDS Prevention gap report shows that HIV prevention efforts must be reinvigorated if the world is to stay on the Fast-Track to ending the AIDS epidemic by 2030. To achieve the global Fast-Track Target of reducing the number of new HIV infections to fewer than 500 000 by 2020, more political commitment and increased investment in HIV prevention, including condom promotion, are needed.
In 2015, an estimated 1.9 million [1.7 million–2.2 million] adults aged 15 years and over were newly infected with HIV—the vast majority through sexual transmission—and an estimated 500 million people acquired chlamydia, gonorrhoea, syphilis or trichomoniasis. Every year, more than 200 million women have unmet needs for contraception, leading to approximately 80 million unintended pregnancies. Condoms effectively prevent all of these.
Male and female condoms are highly effective and the most widely available prevention tool, even in resource-poor settings, for people at risk of HIV infection, other sexually transmitted infections and unintended pregnancies. Condoms are inexpensive, cost-effective and easy to store and transport, their use does not require assistance of medical or health-care personnel and they can be utilized by anyone who is sexually active. A recent global modelling analysis estimated that condoms have averted up to 45 million new HIV infections since the onset of the HIV epidemic. For many young people worldwide, condoms remain the only realistic option to protect themselves.
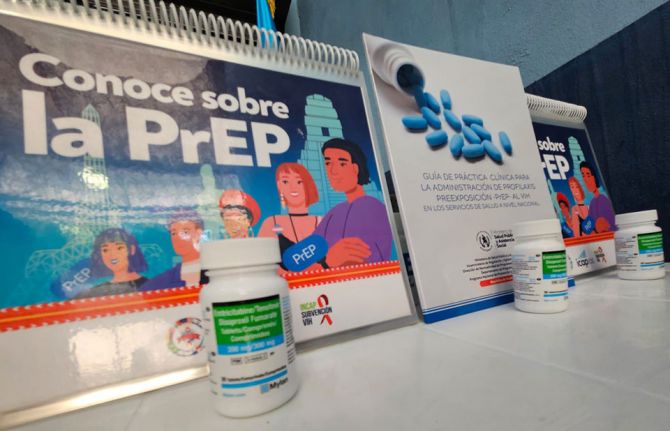
The promotion of consistent use of condoms is a critical component of HIV combination prevention. Condom utilization complements all other HIV prevention methods, including a reduction in the number of sexual partners, voluntary medical male circumcision, pre-exposure prophylaxis (PrEP) and treatment as prevention for serodiscordant couples.
Despite increased use of condoms over the past two decades, studies show that reported use of condoms during a person’s most recent sexual encounter with a non-regular partner ranged from 80% in some countries to less than 30% in others. There is an urgent need for countries to strengthen demand for and supply of condoms and water-based lubricant. Countries agreed in the 2016 Political Declaration on Ending AIDS to increase the annual availability of condoms in low- and middle-income countries to 20 billion by 2020.
Many countries have not yet set ambitious condom distribution and use targets and condoms are suboptimally programmed, with gaps in demand creation and supply. Few condom programmes adequately address the barriers that hinder access and the use of condoms by young people, in particular adolescent girls and young women, gay men and other men who have sex with men and sex workers. In many countries, condoms are not easily available to young people in schools or anywhere outside health facilities. In some contexts, sex workers have unprotected sex with their clients, as carrying condoms is criminalized and used as evidence by the police to harass or prove involvement in sex work. Some programmes only provide a handful of condoms to each sex worker at each visit, but sex workers may have many more clients than condoms supplied. There is also insufficient access to lubricants—less than 25% of men who have sex with men in 165 countries have easy access to free lubricant, and many sex workers, too, desire but lack access to lubricants. Most countries do not plan for the provision of lubricants in their national strategic plans and condom programmes.
International funding for condom procurement in sub-Saharan Africa has stagnated in recent years, and domestic funding has not sufficiently increased. Funding for condom distribution and promotion has even declined. In 2015, there was an estimated gap of more than 3 billion condoms in sub-Saharan Africa against a total need of 6 billion.
To be successful, comprehensive condom programming must address components such as leadership and coordination, supply and commodity security, demand, access and promotion of utilization, and technical and logistic support. It is critical for governments to create an enabling environment among policy-makers and service providers so that users will be made aware of their risks, feel free to demand and access male and female condoms and have the knowledge to use them correctly and consistently. Young people and key populations are strong allies in the promotion of access to condoms. At the last International AIDS Conference in Durban, South Africa, for example, South African youth demonstrated for access to condoms and other sexual and reproductive health services and commodities such as sanitary pads.
Effective condom promotion should be tailored for people at increased risk of HIV and other sexually transmitted infections and/or unintended pregnancy, including young people, sex workers and their clients, injecting drug users and gay men and other men who have sex with men. Many young women and girls, especially those in long-term relationships and sex workers, do not have the power to negotiate the use of condoms, as men are often resistant to their use. Condoms should also be made available in prisons and other closed settings and in humanitarian crisis situations.
There also needs to be a greater leverage of social networks, social media and new technologies to promote condom use and improved focusing. The UNFPA’s CONDOMIZE! campaign to destigmatize and promote condom use is being rolled out in nine countries, led by national governments, with two more national rollouts planned for 2016. The campaign actively involves young people as ambassadors, bloggers and peer educators. In the United States of America, condoms are increasingly promoted and freely distributed in schools in order to address health matters such as unintended teenage pregnancies, sexually transmitted infections and HIV. Cities such as New York and Washington, DC, have established targeted free condom distribution to reach key populations and people at higher risk. In France, condom distribution machines have been placed in schools and the South African Department of Education is in the process of revising its policies in order to allow condom promotion and distribution in schools.
In Zimbabwe, the government has supported large-scale condom distribution through social marketing and free distribution channels. In 2014, 104 million male condoms were distributed in Zimbabwe, one of the highest numbers in the world. Increases in condom use are credited as being one of the reasons that new HIV infections were halved for adults from 2009 to 2015. The South African government has funded a nationwide female condom distribution programme with over 300 distribution sites. In Brazil, public health officials have developed one of the largest condom distribution and promotion campaigns in the world. Despite some objections, the Brazilian government has remained steadfast in its commitment to sharing medically accurate information regarding the benefits of condom use.
Putting condoms on the Fast-Track and achieving 90% condom use by people at risk who are having sex with a non-regular partner would avert an additional 3.4 million new HIV infections by 2020 and would also have a significant impact on preventing other sexually transmitted infections and unintended pregnancies.