Feature Story
The value of integrating HIV prevention and contraceptive services
05 June 2020
05 June 2020 05 June 2020In 2019, the ECHO trial reminded the world of the very high HIV incidence among women in parts of southern Africa. Those high levels of HIV, and of sexually transmitted infections, were found among women accessing routine contraceptive services.
A new joint report by the World Health Organization (WHO) and UNAIDS sets out the steps needed to improve and integrate HIV prevention and contraceptive services in order to reduce new HIV infections among women.
“We need to reflect on the diverse needs of women, including adolescent girls, women with lower levels of education and key populations, who have often been neglected in contraceptive and broader sexual and reproductive health and rights programming. The new approach means more contraceptive choices, additional HIV prevention choices and complementary community activities beyond facilities,” said Paula Munderi, Coordinator of the Global HIV Prevention Coalition at UNAIDS.
The report clearly states that women at the highest risk of HIV and sexually transmitted infections in southern Africa and women from key populations should be the focus for the most urgent action.
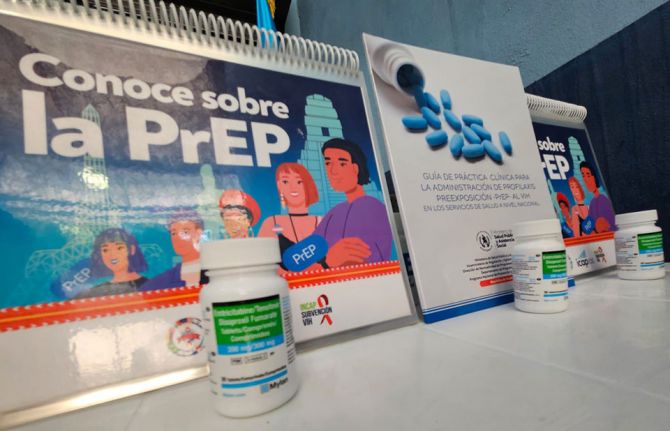
Different approaches in places with different levels of HIV risk are suggested. For example, where there is a high incidence of HIV and sexually transmitted infections, HIV prevention choices, including male and female condoms, and prevention counselling need to be essential elements of contraceptive services and actively promoted. In settings with extremely high HIV incidence in southern Africa, the rapid introduction of pre-exposure prophylaxis (PrEP) within contraceptive services should be considered.
“Sexual and reproductive health and rights and HIV integration have been promoted for more than a decade, yet progress remains limited. Supporting women living with HIV to access contraception in HIV treatment clinics and providing HIV services in contraception services is a critical priority requiring committed funding for concrete action,” said Rachel Baggaley, Unit Head, Testing, Prevention and Populations, Global HIV, Hepatitis and STI programmes at WHO.
In order to understand what women need and want, the report suggests that women be at the centre of decision-making. “HIV prevention and contraceptive choices for women and girls are still not widely available. We need to ensure that the agency and choice of girls and women are promoted by making available a wide range of HIV prevention commodities, ranging from PrEP and microbicides to user-friendly condoms. Women and girls thrive when they are given an opportunity to choose,” said Nyasha Sithole, an advocate for the rights of girls and women from Zimbabwe.
Although people living with HIV who are on antiretroviral therapy and are virally suppressed cannot transmit HIV to their sexual partners, millions of women accessing contraception continue to have unprotected sex with men who do not know their HIV status. As the PopART trial showed, high HIV incidence among young women is also the result of men not accessing treatment. The report proposes concrete steps to strengthen partner prevention, testing and treatment services, including HIV self-tests for men combined with community outreach and gender-transformative prevention approaches.
“Effective integration requires multilayered prevention that can—and should—encompass both sexual and reproductive health and HIV services, including multipurpose prevention technologies. Siloed care, stock-outs and too little input from women themselves are among the long-standing barriers to women’s health care, and COVID-19 exacerbates these difficulties,” said Mitchell Warren, Executive Director of AVAC.
With the physical distancing necessary as a result of the COVID-19 pandemic reducing contact with health services, it will be essential that interactions with health-care providers be optimized through integrating services. “Prevention of HIV and sexually transmitted infections should be the standard of care for contraception information and services provided to women at a high risk of acquiring HIV,” said James Kiarie, Unit Lead, Contraception and Fertility Care, Department of Sexual and Reproductive Health, WHO.