Feature Story
UNAIDS, ASEAN join hands to support work on gender and HIV
07 November 2009
07 November 2009 07 November 2009
(from left): UNIFEM Regional Director East and South East Asia, Dr Jean D’Cunha; UNAIDS Director of the Asia Pacific Regional Support Team, Prasada Rao; Executive Director of the ASEAN Foundation, Filemon Uriarthe Jr; and APN+ Regional Coordinator and Director, Shiba Phurailatmam.
Credit: UNAIDS
Studies in Asia indicate that most women in the region acquire HIV because of their partners who engage in unsafe behaviours. It is estimated that more than 90% of women living with HIV acquired the virus from their husbands or boyfriends while in long-term relationships. An effective AIDS response must address intimate partner relationships to prevent HIV infections in the female partners of men with high-risk behaviours.
In an effort to fill this gap in the AIDS response, UNAIDS and the ASEAN Foundation signed an agreement in Bangkok to support work on gender and HIV in the Asia Pacific region.
The partnership began in 2007 when the United Nations Development Fund for Women (UNIFEM) and UNAIDS joined hands with the ASEAN Foundation in order to strengthen joint work on the gender aspects of HIV.
In 2008 the partnership expanded to include the United Nations Development Programme (UNDP); the Asia Pacific Network of People Living with HIV/AIDS (APN+); the Coalition of Asia Pacific Regional Networks on HIV/AIDS, also known as the Seven Sisters, and the International Community of Women with HIV/AIDS (ICW). The partnership at country and regional levels also included researchers, civil society, people living with HIV and national AIDS commissions.
The project is not only to understand what needs to be done but to pave the way to programmes that work on the ground.
Prasada Rao, UNAIDS Director of the Asia Pacific Regional Support Team
The agreement, which cements this commitment further, was signed in the presence of UNAIDS Director of the Asia Pacific Regional Support Team, Prasada Rao; Executive Director of the ASEAN Foundation, Filemon Uriarthe Jr; UNIFEM Regional Director East and South East Asia, Dr Jean D’Cunha; and APN+ Regional Coordinator and Director, Shiba Phurailatmam.
Speaking on the occasion, Mr Rao said, “The project is not only to understand what needs to be done but to pave the way to programmes that work on the ground.” He added that a range of strategies was needed, including scaling up efforts with key populations at risk in urban areas and through reproductive health programmes for rural women.

Dr D’Cunha stressed the importance of working on gender power dynamics, especially for positive women whose voices must be heard. “All the issues are interconnected and cannot be tackled by any one agency,” he said.
Mr Phurailatham stressed the need to approach women who are considered “low-risk” through their “high-risk” partners. He also stated that it was all the more important that laws criminalizing HIV were changed, as "laws that hamper HIV prevention, criminalize those men at risk can only have a negative impact on the lives of those women."
According to the agreement, funding from the ASEAN Foundation will be leveraged to aid the resources provided through UNAIDS, UNIFEM and UNDP.
HIV and Intimate Partner Relationships
In July this year representatives of AIDS commissions, UNICEF, WHO, the Global Fund to Fight AIDS, Tuberculosis and Malaria and 90 delegates from 15 Asian countries unanimously agreed that intimate partner relationships had to be included in national HIV policies and programmes. A report titled HIV Transmission in Intimate Partner Relationship in Asia was an outcome of this unanimous decision.
The report recommends that HIV prevention interventions be scaled-up for men who have sex with men, injecting drug users and clients of female sex workers. It also suggests that structural interventions should be initiated to identify and address the needs of vulnerable women and their male sexual partners.
UNAIDS, ASEAN join hands to support work on gende
Key populations:
Cosponsors:
Partners:
UNIFEM
Global Fund to Fight AIDS, TB and Malaria
Asia Pacific Network of People Living with HIV/AIDS (APN+)
International Community of Women with HIV/AIDS (ICW)
Coalition of Asia Pacific Regional Networks on HIV/AIDS
Press centre:
50 million women in Asia at risk of HIV from their intimate partners
Feature stories:
HIV transmission in intimate partner relationships in Asia (11 August 2009)
External links:
ASEAN
APN+
International Community of Women with HIV/AIDS
Publications:
HIV transmission in intimate partner relationships in Asia (pdf, 784 Kb.)

Feature Story
UNAIDS participate in Netherlands Multi Party Initiative
06 November 2009
06 November 2009 06 November 2009UNAIDS Executive Director, Mr Michel Sidibé took part in a meeting earlier this week organized by the Netherlands Multi Party Initiative on HIV/AIDS. The meeting was co-organized by the Dutch NGOs “STOP AIDS NOW!” and Aids Fonds under the banner AIDS in a Time of Financial Crisis, to explore together how to face the challenges posed by the global financial crisis.
The event was opened by the Dutch AIDS Ambassador Marijke Wijnroks.
Speaking at the meeting, Mr Sidibé congratulated the Netherlands for their outstanding leadership and stressed the key role the country is playing in the global AIDS response.
“We see the Netherlands as a strong likeminded partner. Together we have achieved much in the battles against discrimination and forwarding the human rights agenda,” said Mr Sidibé.
We see the Netherlands as a strong likeminded partner. Together we have achieved much in the battles against discrimination and forwarding the human rights agenda.
UNAIDS Executive Director Michel Sidibé
“But for every 2 persons who are placed on antiretroviral treatment, 5 people are newly infected – we look forward to a continued strong relationship with the Dutch government to break the trajectory of the epidemic,” Mr Sidibé asserted.
Also participating in the meeting was the Dr Michel Kazatchkine, Executive Director of the Global Fund to Fight TB, Malaria and HIV, Mr Ewout Irrgang, chair of the Multi Party Initiative and Mrs Kathleen Ferrier, vice chair for the Multi Party Initiative.
The Netherlands Multi Party Initiative on HIV/AIDS consists of members of parliament across party lines in the Dutch Parliament. It was established in February 2007 by Kathleen Ferrier, MP.
The primary goal of this informal network is to ensure HIV as well as sexual and reproductive health and rights and related issues are kept on the agenda. The group also raises awareness at the national, regional and international level through the Dutch Parliament, the Council of Europe and the European Parliament.
UNAIDS participate in Netherlands Multi Party Ini
Partners:
Press centre:
UNAIDS congratulates Dr Marijke Wijnroks on appointment as Netherlands AIDS ambassador
Publications:
Donor total contributions 2008 (pdf, 15.5 Kb.)
Donor core contributions 2008 (pdf, 17 Kb.)
Resources for AIDS: urgent action needed (pdf, 492 Kb.)
Global Task Team on Improving AIDS Coordination Among Multilateral Institutions and International Donors (pdf, 784 Kb.)
Related

Feature Story
Antiretroviral treatment for prevention
06 November 2009
06 November 2009 06 November 2009People living with HIV who are following an effective antiretroviral therapy regimen can achieve undetectable viral loads – the amount of virus in a body fluid such s blood, semen or vaginal secretions – at certain stages of their treatment. Research suggests that when the viral load is undetectable in blood the risk of HIV transmission is significantly reduced. However, antiretroviral therapy for prevention has not proven to completely eliminate the risk of transmitting the virus.
To explore the issue WHO earlier this week convened a meeting to review the scientific data available on the use of ART for prevention and also explored the implications of this approach for individuals and communities as well as take into consideration human rights and ethical and public health implications.
Participating in the meeting, UNAIDS Deputy Executive Director, Dr Paul De Lay, provided closing reflections. Dr De Lay said the meeting had raised the hard fact that many people living with HIV - including many who need treatment today - are unable to access HIV testing and counseling and to initiate timely treatment, as a result of a range of social, cultural and economic barriers.
These are exciting and challenging times. The diverse perspectives heard in this meeting reflect the best of the AIDS response, and continuing this dialogue - this committed questioning and the research agenda coming from this meeting - will undoubtedly lead to more lives saved and fewer new infections.
Dr Paul De Lay, UNAIDS Deputy Executive Director
Dr De Lay congratulated the participants in their effort to identifying scientifically sound and innovative ways to accelerate progress toward universal access to HIV prevention, treatment, care and support, and maximizing the effects of ART both for extending full and productive life for people with HIV, and also for primary prevention.
"These are exciting and challenging times. The diverse perspectives heard in this meeting reflect the best of the AIDS response, and continuing this dialogue - this committed questioning and the research agenda coming from this meeting - will undoubtedly lead to more lives saved and fewer new infections" continued Dr De Lay.
UNAIDS strongly recommend a comprehensive approach to HIV prevention that plans and delivers an evidence informed and human rights based combination of programmes and policies, tailored to meet the needs of those most at risk, and including practical programmes to reduce underlying causes of vulnerability, such as gender inequality and HIV related stigma and discrimination.
Antiretroviral therapy will play several roles in combination prevention strategies, along with other key strategies including, but not limited to, social and behavioral change communication to delay sexual debut, promote mutual fidelity and reduction of the number of sexual partners, promote safer sex including correct and consistent male and female condom use, harm reduction programmes for people who use drugs, prevention of vertical transmission, and other biomedical, behavioural and structural prevention programmes.
The WHO hosted antiretroviral treatment (ART) for Prevention was held in Geneva from the 2 to the 4 of November, 2009.
Antiretroviral treatment for prevention
Cosponsors:
Press centre:
Antiretroviral therapy and sexual transmission of HIV
Publications:
Intensifying HIV Prevention: UNAIDS Policy Position Paper (2005) (pdf, 3.80 Mb.)
Practical Guidelines for Intensifying HIV Prevention (2007) (pdf, 1.67 Mb.)

Feature Story
President heralds new era in South Africa’s AIDS response
01 November 2009
01 November 2009 01 November 2009
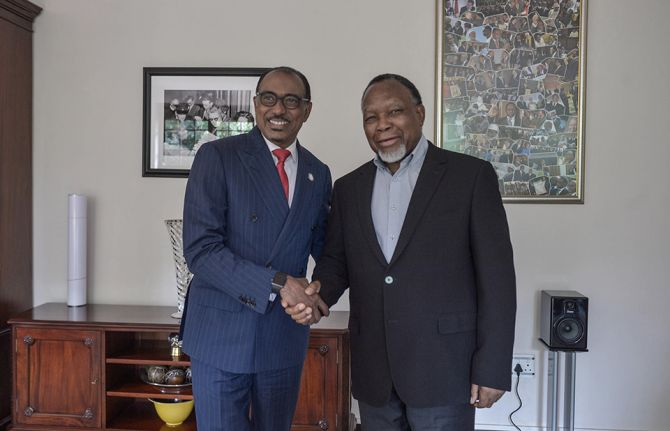
(from left) President of South Africa, Jacob Zuma; UNAIDS Executive Director, Michel Sidibé; and Minister of Health South Africa, Dr Aaron Motsoaledi meet at the opening of the UN General Assembly in New York, 24 September 2009.
Credit: UNAIDS
South Africa’s response to AIDS received a powerful boost with President Jacob Zuma’s landmark speech to the National Council of Provinces on 29 October 2009. The speech heralds the beginning of a new movement to accelerate access towards universal access to HIV prevention, treatment, care and support in the country which has the largest number of people living with HIV. In his speech the President calls on all leaders to work together and use evidence to inform the country’s AIDS response.
Congratulating the President on his bold leadership, UNAIDS Executive Director Michel Sidibé said, “President Zuma has shown extraordinary vision in prioritizing AIDS as an issue of national importance. His call to end denialism and embark on a national mobilization campaign will saves thousands of lives.”
In his speech the President called for a major movement to cut new HIV infections by half and reach at least 80% access to antiretroviral treatment. UNAIDS will support the Government of South Africa in implementing this promise.
Here are some excerpts from speech of President Zuma of South Africa to the National Council of Provinces.
The full speech can be accessed online
President Zuma has shown extraordinary vision in prioritizing AIDS as an issue of national importance. His call to end denialism and embark on a national mobilization campaign will saves thousands of lives.
Michel Sidibé, UNAIDS Executive Director
“Our young democracy faces significant challenges. Though we have achieved much, there is much more that we need to do. Just as we cannot allow ourselves to be overwhelmed by these challenges, we dare not underestimate them. If we are to build the thriving nation for which we have worked so hard, and for which so many have sacrificed so much, we need to appreciate the extent and nature of these challenges.
I would like to highlight two critical challenges, both of which, in different ways, have the potential to undermine our efforts to achieve a better life for our people.
The first of these challenges relates to our economy. The global economy is going through a major economic crisis. The impact of this crisis has been felt by every section of our society. Businesses, both big and small, have been closed. Thousands of workers have lost their jobs. As more families lose their livelihoods and businesses risk collapse, they look to government for assistance….”
“The second challenge that I wish to highlight is no less grave. Indeed, if we do not respond with urgency and resolve, we may well find our vision of a thriving nation slipping from our grasp.
Recent statistics from the Department of Health, Human Sciences Research Council, Medical Research Council, Statistics SA and other sources paint a disturbing picture of the health of our nation. They show that nearly 6 out 10 deaths in our country in 2006 were deaths of people younger than 50 years. If we consider mortality trends over the last decade, we see that the age at which people die has been changing dramatically. More and more people are dying young, threatening even to outnumber in proportional terms those who die in old age.
Honourable Members, South Africans are dying at an increasing rate. The number of deaths registered in 2008 jumped to 756,000, up from 573,000 the year before.
At this rate, there is a real danger that the number of deaths will soon overtake the number of births. The births registered during this period were one million two hundred and five thousand one hundred and eleven (1, 205, 111). The Independent Electoral Commission had to remove 396 336 deceased voters from the Voters Roll during September last year and August this year.
What is even more disturbing is the number of young women who are dying in the prime of their life, in their child-bearing years. In 2006, life expectancy at birth for South African men was estimated to be 51 years. By contrast, life expectancy in Algeria was 70 years and 60 years in Senegal. These are some of the chilling statistics that demonstrate the devastating impact that HIV and AIDS is having on our nation.
Not even the youngest are spared. Some studies suggest that 57% of the deaths of children under the age of five during 2007 were as a result of HIV. This situation is aggravated by the high tuberculosis prevalence. The co-infection rate between HIV and TB has now reached a staggering 73%. Statistics indicate that the numbers of citizens with TB number at 481 584. These statistics do not, however, fully reveal the human toll of the disease. It is necessary to go into the hospitals, clinics and hospices of our country to see the effects of HIV and AIDS on those who should be in the prime of their lives.
It is necessary to go into people’s homes to see how families struggle with the triple burden of poverty, disease and stigma. Wherever you go across the country, you hear people lament the apparent frequency with which they have to bury family members and friends.
Let me emphasize that although we have a comprehensive strategy to tackle HIV and AIDS that has been acknowledged internationally, and though we have the largest anti-retroviral programme in the world, we are not yet winning this battle. We must come to terms with this reality as South Africans.
We must accept that we need to work harder, and with renewed focus, to implement the strategy that we have developed together. We need to do more, and we need to do better, together. We need to move with urgency and purpose to confront this enormous challenge.
If we are to stop the progress of this disease through our society, we will need to pursue extraordinary measures. We will need to mobilize all South Africans to take responsibility for their health and well-being and that of their partners, their families and their communities.
All South Africans must know that they are at risk and must take informed decisions to reduce their vulnerability to infection, or, if infected, to slow the advance of the disease.
Most importantly, all South Africans need to know their HIV status, and be informed of the treatment options available to them. Though it poses a grave threat to the well-being of our nation, HIV and AIDS should be treated like any other disease. There should be no shame, no discrimination, no recriminations. We must break the stigma surrounding AIDS.
In just over a month, we will join people across the globe in marking World Aids Day. Let us resolve now that this should be the day on which we start to turn the tide in the battle against AIDS. Let us resolve now that this should be the day on which we outline those additional measures that need to be taken to enhance our efforts.
Let World Aids Day, on the 1st of December 2009, mark the beginning of a massive mobilisation campaign that reaches all South Africans, and that spurs them into action to safeguard their health and the health of the nation. Though a considerable undertaking, it is well within our means, and we should start now, today, to prepare ourselves for this renewed onslaught against this epidemic.
We have very impressive awareness levels in our country, well over 95%. We should now seriously work to convert that knowledge into a change of behaviour. We have demonstrated in the past that, working together as a nation, we can overcome even the greatest of challenges. We can and will overcome this one.
But we must begin by acknowledging the true nature of that with which we are confronted. We should not be disheartened by what we find. Rather, we should be encouraged to act with greater energy and motivation to overcome.
I have instructed the Minister of Health, as we prepare for World Aids Day, to provide further detail to the nation on the impact of HIV and AIDS on our people. He will do so next week.
The important factor is that our people must be armed with information. Knowledge will help us to confront denialism and the stigma attached to the epidemic.
Informed by this understanding, we expect that the South African National AIDS Council, under the leadership of the Deputy President of the Republic, Mr Kgalema Motlanthe, will develop a set of measures that strengthen the programmes already in place. We must not lose sight of the key targets that we set ourselves in our national strategic plan.
These include the reduction of the rate of new infections by 50%, and the extension of the antiretroviral programme to 80% of those who need it, both by 2011. Prevention remains a critical part of our strategy. We need a massive change in behaviour and attitude especially amongst the youth. We must all work together to achieve this goal.
As we prepare for World Aids Day, and as we undertake the programmes that must necessarily follow, let us draw on our experience of mass mobilization and social engagement. The renewed energy in the fight against AIDS and in mobilizing towards World Aids Day must start now, by all sectors of our society. Working together, we cannot fail.
Whatever challenges we face, we will overcome. Whatever setbacks we endure, we will prevail. Because by working together we can and will build a thriving nation.
President heralds new era in South Africa’s AIDS
Related

Feature Story
UN Secretary-General urges countries to follow the United States and lift travel restrictions for people living with HIV
31 October 2009
31 October 2009 31 October 2009Geneva/New York, 31 October 2009 — UNAIDS welcomes President Obama’s announcement of the final rule removing entry restrictions based on HIV status from US policy. The removal of HIV-related travel restrictions in the US overturns a policy that had been in place since 1987. Such restrictions, strongly opposed by UNAIDS, are discriminatory and do not protect public health.
“I congratulate President Obama on announcing the removal of the travel restrictions for people living with HIV from entering the United States,” said United Nations Secretary-General Ban Ki-moon. “I urge all other countries with such restrictions to take steps to remove them at the earliest.”
The United Nations Secretary-General has made the removal of stigma and discrimination faced by people living with HIV a personal issue. He called for the removal of travel restrictions for the first time in his address to the General Assembly during the High Level Meeting on AIDS in 2008. “That they should be discriminated against, including through restrictions on their ability to travel between countries, should fill us all with shame,” said Secretary-General Ban in a speech to the Global AIDS Conference in August last year.
At his request, several countries including his home country, the Republic of Korea, are in the last stages of removing travel restrictions. Other countries that are considering removal of travel restrictions include China and Ukraine. In 2008, the UNAIDS board strongly encouraged all countries to eliminate HIV-specific restrictions on entry, stay and residence and ensure that people living with HIV are no longer excluded, detained or deported on the basis of HIV status.
“Placing travel restrictions on people living with HIV has no public health justification. It is also a violation of human rights,” said Michel Sidibé, Executive Director of UNAIDS. “We hope that other countries that still have travel restrictions will remove them at the earliest.”
Nearly 59 countries impose some form of travel restrictions on people living with HIV. The International Guidelines on HIV/AIDS and Human Rights state that any restriction on liberty of movement or choice of residence based on suspected or real HIV status alone, including HIV screening of international travellers, is discriminatory. Travel restrictions do not have an economic justification either. People living with HIV can now lead long and productive working lives, a fact that modifies the economic argument underlying blanket restrictions; concern about migrants’ drain on health resources must be weighed with their potential contribution.
UN Secretary-General urges countries to follow th
Press centre:
Related

Feature Story
Empowering women to protect themselves: Promoting the female condom in Zimbabwe
29 October 2009
29 October 2009 29 October 2009Langton Ziromba promotes female condoms in the casual and friendly space of his barber shop
Courtesy of UNFPA
When AIDS first emerged in the 1980s, it mainly affected men. Today, according to UNAIDS figures, women account for about half of the 33 million people living with HIV worldwide, and 60 per cent of those infected in sub-Saharan Africa. Most of these women acquired the virus through heterosexual intercourse, often through unprotected sex with their husbands or long-term primary partners.
“Women think marriage is a safe haven,” says Beauty Nyamwanza of Zimbabwe’s National AIDS Council. “They think that when you’re married, you don’t have to worry about HIV.”
But what the AIDS-prevention team in the country found out is that marriage can actually increase the risk of HIV among young women. According to research carried out in Kenya and Zambia in 2004 , marriage increases the frequency of sex and hinders a woman’s ability to negotiate condom use or abstain from sex. Married women are often afraid to ask their husbands to use a condom – or to use one themselves – since this implies that they suspect their husbands of infidelity.
Women think marriage is a safe haven. They think that when you’re married, you don’t have to worry about HIV.
Beauty Nyamwanza of Zimbabwe’s National AIDS Council
Thanks to the efforts of Ms Nyamwanza and others, Zimbabwe is one of a handful of countries that has taken advantage of the female condom and made major inroads in promoting its use. The latest device, the FC2, is a strong, flexible, nitrile sheath, about 17 centimetres (6.7 inches) long, with a flexible ring at each end. The closed end is inserted into the woman’s body, and the open end remains outside during intercourse. Like the male condom, it offers dual protection against unintended pregnancy and sexually transmitted infections, including HIV. But it has one critical advantage: it is the only available technology for HIV prevention that women can initiate and control.
Condom promoters in Zimbabwe suggest that married women can present the female condom as a means of child spacing. In this way, the issue of a woman appearing to accuse her husband of having other partners and putting her at risk need not arise.
Building support
Zimbabwe introduced the female condom in 1997, but acceptance was slow. Eventually, the Government requested support from the United Nations Population Fund (UNFPA) to scale up promotion of both male and female condoms through the public sector. Beyond training condom promoters, highly creative ways to educate the public about condom use were employed. Billboards, radio spots and TV commercials helped break down taboos against talking about condoms, and thus helped overcome the stigma sometimes associated with them. In the process of implementing the strategy, the team – which included the Ministry of Health and Child Welfare, the Zimbabwe National Family Planning Council, the National AIDS Council and Population Services International (PSI) – discovered that the female condom can be a tool for empowerment, enabling women and adolescent girls to take the initiative in protecting their own reproductive health and that of their partners.
From 2005, when the strategy was launched, to 2008, female condom distribution by the public sector in Zimbabwe increased five-fold, from about 400,000 to more than two million. Sales of female condoms through social marketing rose from some 900,000 to more than 3 million, and sales of male condoms also increased.
Involving men
One person who has seen the change coming is Langton Ziromba. He owns a small, outdoor barbershop in the Budirio section of Harare. In addition to haircuts, shaves and chats about football and women, Mr Ziromba provides another service to his male customers: information about female condoms, how they are used, and the advantages to both partners. He is one of about 70 barbers and 2,000 hairdressers in Zimbabwe who have been trained to promote the female condom. He sells Zimbabwe’s most popular brand, called Care, and makes a small commission on the highly subsidised price.
This poster is part of a major advertising campaign promoting condoms in Zimbabwe
Photo: PSI Zimbabwe
“Our research shows that for this product to be accepted and used by women, we also need to involve men,” says Margaret Butau of the National Family Planning Council. “We customise the benefits of the female condom according to the target group we are addressing.” Specific points highlighted for men include the fact that the female condom is not constricting like the male condom, it is even less prone to breakage, its use does not require an erection and it can enhance pleasure for both partners. Moreover, it is not necessary to withdraw immediately after ejaculation. And, finally, it could be seen as the woman’s responsibility. “When we point all this out, we find that men become curious about having their partners try the product.”
Providing a model for other countries
The Zimbabwe campaign created by PSI that uses hairdressers to market condoms has served as a model for a similar programme in Malawi. Some 2,400 Malawian hairdressers now sell, and serve as advocates for, the female condom in the country. Their numbers are growing as word spreads. Sandra Mapemba, a national programme officer in the UNFPA office in Malawi, says the impact has been dramatic. “The female condom is actually empowering women to become more assertive and to stand up for their own health issues,” she says. “That’s the most exciting thing for me. Women who are in discordant relationships or women who are HIV-positive come and tell me that now they can actually insist on condom use. Before, their partners would refuse.”
The response has been so positive that UNFPA Malawi is now providing training in condom programming to some 35 international and local NGOs working on HIV-prevention in the country. Over the course of three years, female condom distribution through the public sector alone in Malawi increased from 124,000 in 2004-2005 to nearly a million in 2008.
Programming challenges persist
The success of UNFPA and its partners in promoting the female condom in Zimbabwe, Malawi and also in Zambia has prompted other countries to seek similar assistance. Though global distribution of female condoms nearly tripled from 2004 to 2008 – to a total of 33 million in 90 countries – they still represent only 0.2 per cent of condom use worldwide. Key barriers are cost and availability. Not only are female condoms more expensive than male condoms – they cost as much as $1 per unit in some countries – they are still far less widely available. Through an initiative called comprehensive condom programming, UNFPA is helping countries address these and other issues. The programme is also a platform from which other female-initiated prevention technologies still in development, including cervical caps and microbicides, will be launched.
“Giving women the power to protect themselves could turn the tide of the AIDS epidemic,” says Bidia Deperthes, who leads the comprehensive condom programming initiative for UNFPA. “But we still have a long way to go.” The largest obstacle, in her view, is funding for programming. While the majority of donors willingly contribute essential commodities, including male and female condoms, little money is allocated to laying the groundwork needed to create awareness and demand, and to train women to use condoms correctly and consistently. “It’s all part of one comprehensive package.”
This article was adapted from an upcoming UNFPA publication “Prevention Gains Momentum: Successes in female condom programming”.
Empowering women to protect themselves: Promoting
Cosponsors:
United Nations Population Fund (UNFPA)
Partners:
Population Services International (PSI)
The Global Coalition on Women and AIDS
Feature stories:
Barber Shops and Beauty Salons promote HIV education in Guyana (26 March 2009)
Commission on the Status of Women opens with call for action to achieve universal access and gender equality (02 March 2009)
ICASA 2008: Addressing the vulnerability of young women and girls to HIV in southern Africa (03 December 2008)
Publications:
UNAIDS Technical Meeting on Young Women in HIV Hyper-endemic countries of Southern Africa (pdf, 11.3 Mb.)
2008 Delegates Guide to Women and AIDS: All Women, All Rights (pdf, 506 Kb.)

Feature Story
Private sector in West and Central Africa explore strategic partnerships for improved health outcomes
27 October 2009
27 October 2009 27 October 2009
Over 150 participants from 10 WCA countries came to the workshop
Credit: UNAIDS
A strategic combination of private sector know-how and technologies with public sector expertise and funding could lead to improved health and a more efficient AIDS response in West and Central Africa. This was the message from a one day workshop held in Ghana focusing on the role of the private sector in Global Fund processes that brought together 60 companies, 10 national business coalitions tackling HIV and employers federations, as well as trade unions and development partners from all over West and Central Africa.
The workshop was organized at the initiative of UNAIDS and with the support of the Global Business Coalition on HIV/AIDS, TB and Malaria (GBC), the Global Fund to Fight AIDS, TB and Malaria (Global Fund), the International Labour Organization (ILO), the German Development Cooperation (GTZ), and Partenaires contre le Sida (PCS). The October 22 workshop followed a two day event on malaria organized by the GBC.
If we work together to ensure that the resources, know-how, and technologies of the private sector are strategically combined with public sector funding and expertise, we can significantly improve the health and well-being of people in West and Central Africa, and around the world .
John Tedstrom, President and CEO of Global Business Coalition on HIV/AIDS, TB and Malaria
“If we work together to ensure that the resources, know-how, and technologies of the private sector are strategically combined with public sector funding and expertise, we can significantly improve the health and well-being of people in West and Central Africa, and around the world,” said John Tedstrom, GBC’s President and CEO. “By sharing best practices, and collaborating with the Global Fund to ensure that help is delivered to the areas of greatest need, we may finally have the ability to slow down and eventually defeat AIDS, TB and malaria.”
During the lively discussions, participants shared ideas and identified opportunities to partner with the Global Fund both as fund recipients, and as co-investors, in order to scale-up community HIV, TB and malaria programmes. Businesses also discussed how to deploy their resources, skills and expertise to support oversight and governance of the Global Fund mechanisms and processes at the local level. Technical support providers described how and where private sector actors could obtain relevant support at each of the various stages of the Global Fund processes.

The Ministry of Health in Ghana gave the keynote speech
Credit: UNAIDS
The Minister of Health of Ghana, Benjamin Kumbuor gave a keynote speech at the event. He highlighted the importance of working hand in hand with the private sector to support the implementation of HIV, TB and malaria programmes, and that Ghana serves as a good example of this. According to the Minister, the momentum seen in his country should extend across the continent and serve as catalyst for greater impact in reducing the social and economic burden of these epidemics. It also means working collectively to yield greater return on investments and more impact on the ground. UNAIDS agrees. “We need smarter investments in the AIDS response, to ensure that we can achieve more with less,” said Léopold Zekeng, UNAIDS Country Coordinator in Ghana. “As long as there are five people newly infected for every two people starting HIV treatment, we will not change the trajectory of the epidemic. The Global Fund is a strategic and responsive investor in AIDS, and UNAIDS is working in close partnership supporting the Fund’s full grant cycle – from the development of AIDS grant proposals, to programme implementation, to monitoring and evaluation.”

A group photo with all key partners involved in the organization of the workshop: from left to right, GBC CEO, Ghana AIDS Commission Director, Minister of Health, UNAIDS Ghana Coordinator and the UN Resident Coordinator in Ghana.
Credit: UNAIDS
Private sector in West and Central Africa explore

Feature Story
Going beyond social taboos: Parliamentarians begin inclusive dialogue with key groups in Pakistan
27 October 2009
27 October 2009 27 October 2009
Peer outreach workers, Infection Control Society of Pakistan, Karachi.
Credit: UNAIDS/P. Virot
In a move to counter social exclusion and change discriminatory practices, a dialogue has begun in Pakistan between the government, parliamentarians and communities often overlooked by policymakers. An historic meeting was held late last month when a number of parliamentarians began a dialogue with community members on the challenges facing transgendered people, people who use drugs and people living with HIV. This meeting was a first, and aimed to create an enabling environment for policy changes related to HIV.
Among the general population in Pakistan HIV prevalence is less than 0.1%, however results from the recent HIV Second Generation Surveillance in the country indicate that injecting drug users and the transgender community are the two populations with the highest rate of HIV infection in the country, with an estimated 20% and 7% prevalence respectively. HIV infection is not the sole concern of these populations who can also be caught up in a cycle of social and economic exclusion exposing them to marginalization and violence, limited access to health and others services, and, for drug users, a lack of drug substitution programmes.
Leadership shown by a few, through a courageous dialogue with parliamentarians represent a voice of change for countless others.
Oussama Tawil, UNAIDS Country Coordinator for Pakistan
The dialogue, held at a parliamentary sub-committee level, brought together parliamentarians from across party lines; associations and groups representing people living with HIV such as the Red Ribbon Initiative, Pak Plus and New Light AIDS Control Society; the Sathi Foundation for transgenders; as well as Nai Zindagi, an organization that provides services for drug users.
It was also an opportunity for parliamentarians to discuss with senior police, narcotics control and health officials who were present the need for changes in policy and practice towards key groups. Discussions ranged from an urgent call to push through pilot substitution therapy which is still awaiting final government clearance, to introducing a special focus on transgender within police training and investigations on sexual violence and abuse perpetuated against them.

Outreach Work among drug users. Nai Zindagi, Lahore.
Credit: UNAIDS/P. Virot
The government of Pakistan already endorses harm reduction within a wider approach to drug prevention and control, and non-governmental organizations collaborate closely with the Ministry of Health on needle exchange programmes.
Discussions also touched on issues affecting the general population. People living with HIV in Pakistan risk losing their employment or at times refusal by health workers to provide care to them; and people working overseas such as in the Gulf States have faced deportation back to Pakistan once detected HIV positive.
The Pakistan government’s response to HIV began in 1987 with the establishment of a Federal Committee on AIDS by the Ministry of Health, soon after the first case of AIDS was reported. Today the country’s National AIDS Control Programme is implemented through federal and provincial implementation units.
Funding gap
However Pakistan is currently facing a considerable gap in funding the scale-up of community-based efforts which represent the backbone of the national AIDS response. The country benefits from donor support, in particular from the World Bank, UK and other bi-laterals to scale up HIV prevention, treatment, care and support. Despite applications for resources from the Global Fund to Fight AIDS, TB and Malaria in recent years, grants on HIV have yet to be secured though needs are clear.

Needle disposal programme for people who inject drugs. Nai Zindagi, Lahore.
Credit: UNAIDS/P. Virot
Speaking during the meeting, Member of the National Assembly and Chair of the Parliamentary Sub-Committee on AIDS, Dr Donya Aziz said, “Donor support is essential for us at this point, yet, in the long run, we cannot rely on external funds. Public and private sectors must mobilise resources, while policy decisions are needed to ensure services and to address social exclusion in our communities.”
In spite of the challenges ahead, participants at last month’s gathering felt that the breakthrough in challenging mistrust towards communities heralded by this meeting is an important milestone on which progress can be built.
The dialogue is just the beginning and will be followed up with a series of meetings to be held among a larger forum of parliamentarians across party lines and civil society groups. Hopes are high that policy change and attitude change will also follow.
UNAIDS Country Coordinator for Pakistan Oussama Tawil echoes this hope, “Leadership shown by a few, through a courageous dialogue with parliamentarians represent a voice of change for countless others.”
Going beyond social taboos: Parliamentarians begi
Key Populations:
People who use injecting drugs
People living with HIV
Press centre:
India and Pakistan fight AIDS through cricket
Feature stories:
First association for people living with HIV in Pakistan (24 August 2007)
Pakistan cricket team talks about HIV prevention (15 September 2007)
External links:
National AIDS Control Programme, Pakistan
Publications:
Pakistan: Involvement of key policy makers in the fight against HIV (pdf, 113 Kb.)
HIV prevalence among injecting drug users, men having sex with men, and female sex workers in Pakistan, 2004–2007

Feature Story
Eastern Europe and Central Asia HIV conference for joint efforts towards Universal Access
27 October 2009
27 October 2009 27 October 2009
Opening plenary of 3rd EECAAC, Moscow, 28 October 2009.
Credit: UNAIDS
The 3rd HIV/AIDS Conference in Eastern Europe and Central Asia opened in Moscow today with a ceremony attended by senior representatives of Russian Duma, Russian Ministry of Foreign Affairs, Russian Academy of Sciences and the US Ambassador to the Russian Federation.
The meeting brings together political leaders, scientists, health professionals, representatives of civil society and religious organizations as well people living with HIV. There are 2500 participants gathered from 60 countries, of whom 58% are women. The conference organizers hope it will invigorate the response to the AIDS epidemic across the region.
Injecting drug use is the main mode of HIV transmission across Eastern Europe and Central Asia. HIV prevention among drug users and their sexual partners is a vital component of an evidence-informed response.
In a plenary session, UNAIDS Executive Director Mr Michel Sidibé gave an overview of global AIDS response and outlined the way forward for achieving universal access goals. The event, which runs in Moscow until 30 October, is based on the theme “Regional cooperation. Join the Efforts for Universal Access”.
UNAIDS is very concerned that Eastern Europe and Central Asia is the only region of the world where HIV prevalence clearly remains on the rise.
Michel Sidibé. UNAIDS Executive Director
In his address, Mr Sidibé said that there has been tremendous progress in the region with many countries set to achieve universal access target goals. But the UNAIDS head also noted that the AIDS epidemic continues to outpace the response as the estimated number of adults and children living with HIV in the Eastern Europe and Central Asia region has doubled since 2001. Nearly 1.5 million people are living with HIV and the majority of them live in Russia and Ukraine.
“UNAIDS is very concerned that Eastern Europe and Central Asia is the only region of the world where HIV prevalence clearly remains on the rise,” said Mr Sidibé.
“In this region, non-governmental organizations have implemented some of the best services for prevention, treatment and support in the world. In several countries of the region, harm reduction programmes are driven by civil society and we are seeing the first signs of their impact on the epidemic. I encourage the governments of this region to sustain and scale-up programmes delivered by civil society.,” continued Mr Sidibé.

Credit: EECAAC
In the session, Mr Sidibé also highlighted some of the accomplishments that have been achieved in the region, such as the coverage of prevention of mother-to-child HIV transmission programmes that exceeds 95%, hoping that the region would be the first to eliminate HIV transmission from mother to child by 2015.
The Russian federal authorities with support from UNAIDS, The Global Fund to Fight AIDS, Tuberculosis and Malaria, and the International AIDS Society have organised the event. The organising committee is chaired by G.G. Onishchenko, Head of Russian the Federal Service for the Protection of Consumers Rights and Human Wellbeing, and the country’s Chief Sanitary Physician. The conference, first held in 2006, has traditionally been hosted in Moscow and is the leading public forum for dialogue on public health and HIV in the region.
This year’s conference aims to set priorities for the region, with special emphasis on HIV prevention among key groups, including sex workers and people who inject drugs, while taking into consideration the nature of the epidemic in each country across Eastern Europe and Central Asia.
HIV epidemic in Eastern Europe and Central Asia
According to the 2008 UNAIDS report on the global AIDS epidemic, about 1.5 million people were estimated to be living with HIV in Eastern Europe and Central Asia in 2007; almost 90% of them living in either the Russian Federation or Ukraine.
Although HIV epidemic in the Russian Federation is the largest in the region, there are rising numbers in Azerbaijan, Georgia, Kazakhstan, Kyrgyzstan, the Republic of Moldova, Tajikistan, and Uzbekistan.
There is increasing political and financial commitment for HIV prevention, treatment and care in Russia, even in the face of a global financial crisis, with the country set to increase the number of people on antiretroviral treatment by 50,000 in 2009.
Eastern Europe and Central Asia HIV conference fo
Partners:
Global Fund to Fight AIDS, Tuberculosis and Malaria
International AIDS Society
Press centre:
AIDS threat growing throughout Europe: UN, World Bank and Global Fund call on European Ministers to scale up HIV prevention and treatment programmes
Global Fund and UNAIDS Call for Rapid Scaleup of Efforts to Combat AIDS
Speeches:
Multimedia:
Feature stories:
Eastern Europe and Central Asia : News archive
Towards Universal Access in Eastern Europe and Central Asia: Delivering on AIDS today and in the longer term (14 April 2008)
External links:
Visit the official web site of the conference
Publications:
HIV prevalence (%) in adults in Eastern Europe and Central Asia, 2007
Related

Feature Story
UNAIDS and International Olympic Committee strengthen partnership
26 October 2009
26 October 2009 26 October 2009
UNAIDS Executive Director Michel Sidibé (left) and the President of the International Olympic Committee, Jacques Rogge. Lausanne, 26 October 2009.
Copyright: IOC/Arnaud Meylan
UNAIDS Executive Director Michel Sidibé earlier today met with Jacques Rogge, the President of the International Olympic Committee (IOC) at its headquarters in Lausanne, Switzerland.
UNAIDS and IOC have a long standing partnership to enhance the role of sports organisations in the AIDS response which was formalized in the Memorandum of Understanding singed in 2004. The two organizations have also collaborated in efforts to raise AIDS awareness with coaches, athletes and sports personalities.
In 2005, an HIV prevention toolkit was developed which features practical information on HIV prevention programming and includes messages from international sports’ stars, some of whom are living with HIV. The tool kit has been translated into French, Portuguese, Chinese, Russian, Swahili and Spanish, with an Arabic version planned for 2010.
The partnership has since developed into a range of joint initiatives including the sponsoring by IOC of several regional workshops on HIV and sport, and a series of events to launch the translated versions of the toolkit.
I look forward to the growing relationship between IOC and UNAIDS. By working together in the spirit of the core values of the Olympic Movement—friendship, excellence and respect—we can be a force for positive change.
UNAIDS Executive Director Michel Sidibé
At the meeting, Michel Sidibé thanked the IOC for the role played by IOC on HIV advocacy leveraging the National Olympic Committees as implementing arms of the IOC in responding to the HIV epidemic.
Praising the work of the IOC, Michel Sidibé stressed the importance of partnerships like this one for the HIV response. “I look forward to the growing relationship between IOC and UNAIDS. By working together in the spirit of the core values of the Olympic Movement—friendship, excellence and respect—we can be a force for positive change.”
The IOC and UNAIDS both try to reach out to as many young people as possible. It is our common goal to use sport as a powerful tool in the education about and the prevention of HIV & AIDS across the globe.
Jacques Rogge, the President of the International Olympic Committee (IOC)
"The partnership between our two organisations has been strong in the past and will be even stronger in the future,” said Jacques Rogge, the President of the International Olympic Committee (IOC). “The IOC and UNAIDS both try to reach out to as many young people as possible. It is our common goal to use sport as a powerful tool in the education about and the prevention of HIV & AIDS across the globe," Mr Rogge continued.
In countries with generalized epidemics, community based sports organizations and non-governmental organizations are particularly vulnerable to the impact of HIV, given that they often rely on people with specialized skills and volunteers who can be difficult to replace should they fall ill.
The partnership between UNAIDS and the IOC was particularly successful around the 2008 Olympic Games in Beijing. The “Play Safe – Help Stop HIV – Play your part in protecting the world around you” campaign for the Beijing games, was jointly planned and executed by the IOC, the Beijing Organizing Committee for the Games of the XXIX Olympiad and UNAIDS.
Highlights of the campaign include HIV awareness raising activities targeting migrant workers at construction sites of the Olympic venues supported by UNAIDS and a private partner. UNAIDS mobilized nine UN agencies, the Red Cross, Marie Stopes International as well as groups of people living with HIV, to train 7,000 Olympic volunteers on HIV prevention and countering stigma and discrimination.
The activities reached close to 100,000 young people that had volunteered for the Beijing Olympics with information about HIV and sexual health. 100,000 high quality condoms packaged in 50,000 leaflets with information on HIV prevention and anti-discrimination were made available in the clinics in the Olympic Villages.
During the meeting Mr Sidibé also congratulated the IOC on having been granted permanent observer status to the United Nations General Assembly in New York. The decision pays tribute to the IOC’s efforts to contribute to the achievement of the UN Millennium Development Goals by using sport as a tool, the IOC and its partners implement various activities across the globe
At the meeting, Mr Sidibé and Mr Rogge also discussed future joint activities at the Vancouver 2010 Winter Games, Singapore 2010 Youth Olympic Games and London 2012 Summer Games.
The forthcoming collaboration between IOC and UNAIDS around the London Games will focus on HIV prevention as well as countering stigma and discrimination around HIV. Together IOC and UNAIDS can make a difference and promote the Olympic values and instil hope.
UNAIDS and International Olympic Committee streng
Partners:
International Olympic Committee
Feature stories:
Olympics 2008: AIDS awareness training for young volunteers in China (25 June 2008)
Carrying the Olympic flame for PLHIV in Tanzania (18 April 2008)
Publications:
Together for HIV & AIDS prevention: a toolkit for the sports community (pdf, 4.81 Mb)