Documents
HIV and cervical cancer
17 November 2022
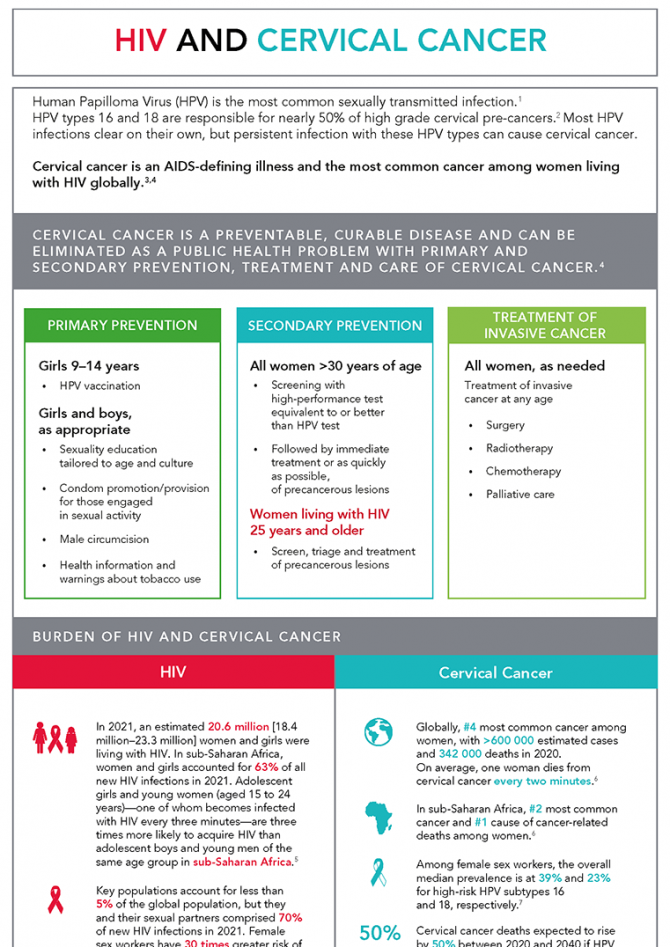
Human Papilloma Virus (HPV) is the most common sexually transmitted infection, and two types of HPV (16 and 18) cause nearly 50% of high-grade cervical pre-cancers. HIV and cervical cancer are inextricably linked. Women living with HIV are six times more likely to develop cervical cancer, which is one of the AIDS-defining illnesses and the most common cancer among women living with HIV globally. Cervical cancer is a preventable, curable disease and can be eliminated as a public health problem with primary and secondary prevention, treatment, and care of cervical cancer, in combination with addressing social, health and other inequalities and integrated approaches. This document is also available in Arabic




Feature Story
United for ending cervical cancer, HIV and inequities for women and girls
17 November 2022
17 November 2022 17 November 2022On this Day of Action, as we celebrate a two-year anniversary of the launch by the World Health Organization (WHO) of the Global Strategy to accelerate the elimination of cervical cancer as a public health problem, we are reminded that despite the availability of the knowledge, tools and technologies, cervical cancer still kills more than 342 000 women a year (in 2020) globally. Every two minutes one woman loses her life to cervical cancer - a disease that is preventable and curable.
The high burden of cervical cancer is driven by gender, social and economic inequalities and health disparities in access to HPV vaccines, screening, care and modern prevention and treatment technologies. Because of those inequalities, women and girls in low- and middle-income countries (LMICs) remain most affected. Nine out of 10 women who die of cervical cancer reside in LMICs. Cervical cancer is the number one cause of cancer-related death among women living in sub-Saharan Africa.
The WHO Global Strategy to eliminate cervical cancer launched by the WHO on 17 November, 2020 was supported among many by the UN partner organizations including IAEA, UNAIDS, UNFPA , UNICEF, and Unitaid. The UN Joint Action Group comprised of these six UN entities each bringing in its unique mandates and resources, is committed to supporting countries efforts in meeting by 2030 the global cervical cancer elimination targets – whereby 90% of girls are fully vaccinated against HPV by age 15, 70% of women are screened with a high-performance test between the ages of 35 to 45, and 90% of women identified as having cervical disease receive treatment. If these targets are met, 300 000 deaths from cervical cancer could be averted by 2030, 14 million by 2070, and over 62 million by 2120.
“In countries with high rates of HIV, over 50% of cervical cancer cases are reported among women living with HIV. Women living with HIV are six times more likely to develop cervical cancer and to develop it at younger age than those without HIV. It is unacceptable to claim that we have saved a woman’s life by enabling access to antiretroviral therapy for HIV alone, if we then leave her to die from cervical cancer. Our joint focus is on breaking down silos, building bridges between HIV and cervical cancer programmes, and bringing the two communities together because we know that linkages save lives.” – Winnie Byanyima, UNAIDS Executive Director
“No woman should die of cervical cancer when we have a highly effective HPV vaccine and quality diagnostics. We need prevention and early detection - this is how we ensure that this disease is eliminated globally. Governments and partners need to invest in accelerated access to resilient primary health care that delivers integrated care like routine immunization and sexual and reproductive health. And we must commit robust long-term human resources for adequate and accessible health care workers in communities and at facility level. Funding for health and health equity are prerequisites for cervical cancer elimination around the world.” - Dr Aboubacar Kampo, Director of Health Programme, UNICEF New York HQ
“We have the tools and technologies to end cervical cancer. Now it is a question of access. Unitaid stepped up the moment WHO issued its call to action, and within just a few years we have introduced effective technologies and developed screen-and-treat models that work in resource-limited settings. The last piece of the puzzle is scale up – we need to see a concerted global effort so every last woman can benefit from life-saving preventive care and we can end cervical cancer for generations to come.” – Dr Philippe Duneton, Executive Director, Unitaid
“Despite being one of the leading causes of death from cancer for women in low- and medium-income countries (LMICs), cervical cancer is also one of the most preventable and treatable cancer types. Nuclear applications such as diagnostic imaging can help detect the cancer at an early stage and increase survival rates. Radiotherapy can successfully treat women with cervical cancer, even in advanced cases. With our Rays of Hope initiative, we aim to increase access to these technologies worldwide and close the unacceptable gap of inequality.”- Najat Mokhtar, IAEA Deputy Director General and Head of the Department of Nuclear Sciences and Applications
“On this second anniversary of the Global Strategy for Cervical Cancer Elimination, the UN Joint Action Group (UNJAG)* celebrates the successes achieved. As the world population continues to grow, more girls and women will require life-saving vaccination, screening and treatment. We acknowledge the need for effective mobilization of resources and partners to achieve the 90-70-90 global elimination targets. Going forward we will continue to focus our attention and joint efforts on ensuring full prevention, high quality life-saving services and equity in access to modern technologies for women and girls across the world.” – Petra ten Hoope-Bender, UNJAG Chair, Technical Adviser Sexual and Reproductive Health and Rights, UNFPA.
* IAEA, UNAIDS, UNFPA, UNICEF, UNITAID and WHO
Related




Press Release
UNAIDS and IAEA forge a powerful partnership against the interlinked diseases of cervical cancer and HIV
07 February 2020 07 February 2020GENEVA, 7 February 2020—UNAIDS and the International Atomic Energy Agency (IAEA) have joined forces to increase action against cervical cancer and HIV. In a memorandum of understanding signed following an event to mark World Cancer Day at the headquarters of IAEA in Vienna, Austria, the two organizations pledged to scale up and expand services for adolescent girls and women affected by the two diseases.
Cervical cancer and HIV are inextricably linked. Cervical cancer is the most common cancer among women living with HIV, who are up to five times more likely to develop the disease, and women infected with certain types of the human papillomavirus also face a double risk of acquiring HIV.
"How is it fair that 90% of girls in high-income countries have access to the human papillomavirus vaccine, yet in low- and middle-income countries just 10% have access?" said Winnie Byanyima, Executive Director of UNAIDS. "Like HIV, cervical cancer is a disease of health, gender and socioeconomic inequalities for women and girls all over the world. Services must be expanded and integrated as an investment in the lives of women and girls and to uphold their right to health.”
In 2018, around 311 000 women died of cervical cancer, 85% of whom were in low- and middle-income countries, where vaccination, screening and treatment programmes are limited. The high mortality rate from cervical cancer globally could be greatly reduced by stepping up action in those countries.
Around 70% of women who develop cervical cancer require radiotherapy to effectively treat the disease; however, IAEA estimates that one third of low- and middle-income countries do not offer adequate radiation medicine services to meet patient needs. In Africa, 28 countries do not have a single radiotherapy unit. Part of IAEA’s work is to help countries in the use of nuclear and radiation medicine to treat cervical and other types of cancer.
“Cervical cancer is one of those cancers that are perfectly treatable and curable if you live in Vienna, Buenos Aires, Rome or Paris,” said IAEA Director General Rafael Mariano Grossi. “If you happen to live in a country with limited access to radiotherapy that is something that can kill you.” He added that the partnership with UNAIDS was very important to maximize efforts in the important mission to help countries tackle cancer.
As part of the new agreement, UNAIDS and IAEA will work together to support national strategies and programmes to develop integrated workplans for HIV and cervical cancer. In addition, they will mobilize resources to expand prevention, diagnosis and treatment services, train health professionals and raise awareness around the links between HIV and cervical cancer.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)




Press Release
Go Further partnership reaches over half a million HIV-positive women with cervical cancer screening in its first year
25 September 2019 25 September 2019The United States’ PEPFAR program, the George W. Bush Institute, Merck and UNAIDS are aiming to end AIDS and cervical cancer in Sub-Saharan Africa within a generation through an innovative public-private partnership
NEW YORK, 25 September 2019—On the margins of the 2019 United Nations General Assembly, former President George W. Bush and Ambassador Deborah L. Birx announced that the Go Further partnership to end AIDS and cervical cancer has reached over half a million HIV-positive women with cervical cancer screening and treated thousands of women for pre-invasive cancerous lesions in its first year. The partnership aims to reduce new cervical cancer cases by 95 percent among the estimated 3.8 million HIV-positive women who live in eight high-burden African countries.
At the Bloomberg Global Business Forum, President Bush, Mrs. Laura Bush, and Ambassador Birx met with His Majesty King Mswati III of Eswatini, The Right Honourable Dr. Thomas Thabane of Lesotho, His Excellency President Peter Mutharika of Malawi, The Honorable Michael Bloomberg, CEO of Bank of America Brian Moynihan, and others.
"We strongly believe that by helping these leaders save lives in their countries it makes the world a better place and makes America more secure," President Bush said. "We have many leaders here all of whom are taking the lead, all of whom are responsible, all of whom are measuring results. It's important for the American people to know that the results are astounding."
"The future of each of your countries depends on all of your citizens—men and women—taking care of their health," Mrs. Bush added.
“Go Further is helping women in Africa to lead longer, healthier lives,” said Ambassador Birx, M.D., United States Global AIDS Coordinator and Special Representative for Global Health Diplomacy, who leads PEPFAR. “By leveraging the robust health care delivery platforms in Africa strengthened through over $85 billion in total U.S. government global HIV/AIDS investments, we will protect millions of HIV-positive mothers, daughters, aunts, and grandmothers—who are alive and thriving with HIV treatment—from the threat of cervical cancer.”
Launched in May 2018, Go Further is an innovative public-private partnership between the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), the George W. Bush Institute (Bush Institute), the Joint United Nations Programme on HIV/AIDS (UNAIDS), and Merck (known as MSD outside of the United States and Canada). For maximum impact, the partnership focuses on reaching HIV-positive women in countries with among the highest HIV prevalence and cervical cancer incidence rates in the world.
“Go Further builds on the Bush Institute’s longstanding initiative to support women in Africa by scaling efforts to save more lives,” said Holly Kuzmich, Executive Director of the Bush Institute. “Healthy and empowered women contribute to healthier families, communities, and countries, and this partnership is proud to invest in high-burden nations to improve women’s health and economic futures, reduce suffering, and expand the reach of care.”
An estimated 100,000 women are diagnosed annually with cervical cancer in Sub-Saharan Africa. Without treatment, 62 percent of these women would be expected to die from the disease. Additionally, women who are HIV-positive are five times more likely to develop invasive cervical cancer. To address these risks, Go Further is increasing access to the human papillomavirus vaccine to prevent cervical cancer, expanding the availability of vital cervical cancer screening, and providing treatment for women most vulnerable to developing cervical cancer. With minimal additional investment, these low-cost interventions can save millions of lives and help secure global gains against HIV/AIDS.
“At Merck, we are committed to addressing the health care needs of women in the developing world and are proud to partner with PEPFAR, the Bush Institute, and UNAIDS on Go Further,” said Carmen Villar, Vice President, Social Business Innovation, Merck. “Through this partnership we are addressing cervical cancer in HIV-positive women in Sub-Saharan Africa, one of the populations most heavily impacted by cervical cancer, not only through screening and treatment but also through prevention.”
“To save a woman’s life by providing access to treatment for HIV, yet she dies from cervical cancer because she hasn’t had access to cancer screening is unacceptable,” said Gunilla Carlsson, Executive Director a.i. UNAIDS. “The Go Further partnership is critical to ensure that HIV and cervical cancer services are integrated and available to the women and girls that need them most."
The Go Further strategy builds on seven years of collaboration between PEPFAR and the Bush Institute and evolves the partnership to save more lives.
Learn more about Go Further at www.gofurther.org, and follow the partnership on Twitter, Instagram, and Facebook.
The U.S. President’s Emergency Plan for AIDS Relief
PEPFAR is the United States government’s response to the global HIV/AIDS epidemic, which has invested over $85 billion since 2003 – the largest commitment by any nation to address a single disease in history. Through the compassion and generosity of the American people, PEPFAR has saved 17 million lives, prevented millions of HIV infections, and helped transform the global HIV/AIDS response. For more information, please visit www.pepfar.gov, and connect with PEPFAR on Twitter, Facebook, Instagram and YouTube.
George W. Bush Institute
Housed within the George W. Bush Presidential Center, the George W. Bush Institute is an action-oriented, nonpartisan policy organization with the mission of developing leaders, advancing policy, and taking action to solve today’s most pressing challenges. For more information, please visit www.bushcenter.org.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
PEPFARDavid Haroz
tel. +1 202 445 3269
harozd@state.gov
Bush Institute
Miriam Spradling
tel. +1 972 639 6099
mspradling@bushcenter.org
UNAIDS
tel. +41 79 514 6896 / +41 22 791 42 37
communications@unaids.org
Press centre
Download the printable version (PDF)


Feature Story
The little-known links between cervical cancer and HIV
31 May 2019
31 May 2019 31 May 2019Cervical cancer is the most common cancer among women living with HIV. The likelihood that a woman living with HIV will develop invasive cervical cancer is up to five times higher than for a woman who is not living with HIV. The overall risk of HIV acquisition among women is doubled when they have had a human papillomavirus (HPV) infection.
So, what can be done? This is one of the questions that will be discussed at a number of events addressing cervical cancer at the 2019 Women Deliver conference, which will take place in Vancouver, Canada, from 3 to 6 June.
Like HIV, cervical cancer is a disease of gender and other inequalities. These two interconnected diseases starkly expose the links between inequity and social and health injustice. Ninety per cent of 311 000 cervical cancer deaths globally per year occur in low- and middle-income countries, with the highest burden borne by sub-Sahara African countries that have the highest burden of HIV. In Zambia, rates of cervical cancer are almost 10 times higher than in Australia, for example, and women are 10 times more likely to die of cervical cancer in eastern and southern Africa than they are in western Europe.
Cervical cancer is preventable and curable if diagnosed and treated early. Effective methods of primary prevention of cervical cancer, notably the HPV vaccine, are available, but not to everyone. Currently, just 10% of girls in low- and middle-income countries access the HPV vaccine, compared with 90% in high-income countries.
Scale-up is happening and efforts to prevent and treat cervical cancer are showing dramatic results in areas where programmes have been rolled out at sufficient scale. Australia is set to become the first country in the world to eliminate cervical cancer by successfully implementing a combined approach to HPV vaccination and cervical cancer screening and early treatment at a wide scale. In Scotland in the United Kingdom, where the immunization programme was introduced some 10 years ago, there has been a 90% decrease in precancerous cells, which has led to a dramatic reduction in preinvasive cervical disease. Remarkable achievements, which should be universal.
“To save a woman’s life by ensuring that she has access to antiretroviral therapy for HIV, yet she dies from cervical cancer, is unacceptable,” said Shannon Hader, UNAIDS Deputy Executive Director, Programme. “UNAIDS’ focus is on breaking down silos and building bridges between HIV and cervical cancer programmes because we know that synergies save lives.”
Despite their increased risk of cervical cancer, women living with HIV do not receive regular screening or treatment for cervical cancer, even with the World Health Organization (WHO) recommended simple, low-cost visual inspection or effective simple, early treatment methods.
According to recent large studies, only 19% and 27% of women living with HIV aged 30–49 years in Malawi and Zambia, respectively, have ever been screened for cervical cancer.
A smart investment is to integrate cervical cancer screening and treatment services into HIV and sexual and reproductive health services. HIV platforms are ready-made entry points for low-cost cervical cancer services and wider health service coverage for young women and girls.
An important lesson learned from the AIDS response is that civil society and communities have to be at the centre. Networks of women living with HIV and women’s rights and youth movements are formidable allies. They have fought for an AIDS response rooted in human rights, social justice and sexual and reproductive health and rights and can mobilize, advocate and create demand for services. Civil society must also keep us on track to end stigma and discrimination, including in health-care settings. Communities can also provide direct services for HIV, cervical cancer and other diseases.
Shared responsibility and country leadership and ownership are critical. With collective efforts of governments, communities, donors, the private sector, innovators and researchers, important synergies can be made, and lives saved.
UNAIDS is working with partners to ensure that policies are informed by evidence, that ambitious targets are set and that adequate levels of human and financial resources are available. UNAIDS is using the political and programmatic platforms of the Fast-Track approach as part of the initiative to scale up the prevention and treatment of cervical cancer and HIV.
UNAIDS is working in partnership with initiatives such as WHO’s global call to action towards the elimination of cervical cancer and is part of a renewed Partnership to End AIDS and Cervical Cancer with the United States President’s Emergency Plan for AIDS Relief and the George W. Bush Institute.
“It is high time to make both AIDS and cervical cancer history!” added Dr Hader.
2019 Women Deliver conference
Related


Feature Story
It’s time to make cervical cancer history
04 February 2019
04 February 2019 04 February 2019Cervical cancer is preventable with the human papillomavirus vaccine. And if detected and treated early, it’s also curable. So why are so many women still developing and dying from cervical cancer?
In 2018, there were an estimated 570 000 new cases of cervical cancer and 311 000 deaths from it worldwide. Much like HIV, cervical cancer is a disease fuelled by social, economic and political inequities. Lower-income countries bear the highest burden, with nearly 80% of all cervical cancers and 90% of deaths.
If cervical cancer prevention, screening and treatment are not urgently scaled up, experts estimate that by 2040 there could be a 50% increase in deaths over 2018 levels.
HIV and cervical cancer are tightly intertwined. Cervical cancer is the most common cancer among women living with HIV. Women living with HIV are up to five times more likely to develop invasive cervical cancer than other women. In sub-Saharan Africa, cervical cancer is the number one cancer killer of women.
Despite the increased risk, many women living with HIV do not have access to regular screening or treatment for cervical cancer. A 2016 study in Malawi showed that only 19% of women aged 30–49 years living with HIV had ever been screened for cervical cancer. In the survey, among the poorest women living with HIV, only 2% had ever been screened for the disease.
“It is unacceptable that women around the world are dying from cervical cancer because they do not have access to life-saving vaccines, screening and treatment,” said Ani Shakarishvili, a Special Adviser at UNAIDS. “We save a woman’s life by ensuring that she has access to antiretroviral therapy for HIV, yet she dies from cervical cancer. Services must be integrated and available to all, without exception.”
Linking cervical cancer screening and HIV services is cost-effective and saves lives. UNAIDS is working with the United States President’s Emergency Plan for AIDS Relief and the George W. Bush Institute to incorporate cervical cancer screening and care into clinics where women are already accessing HIV services in eight countries across sub-Saharan Africa. The partnership aims to reduce cervical cancer incidence by 95%.
The World Health Organization has recently announced that it will be accelerating global efforts to eliminate cervical cancer as a global public health problem and will continue to take a leading role, including by developing a global strategy towards eliminating cervical cancer, a move warmly welcomed by UNAIDS.
“As in the global AIDS response, we must approach cancer prevention and treatment as an opportunity to lead a broad coalition demanding health as a fundamental, universal human right,” added Ms Shakarishvili.
On 4 February, World Cancer Awareness Day, UNAIDS is recommitting its support to the global call to action to eliminate cervical cancer and address inequalities by raising awareness and increasing access to prevention, detection and treatment for girls and women at risk, including women and girls living with HIV.
Related


Feature Story
Cervical cancer and HIV—two diseases, one response
01 October 2018
01 October 2018 01 October 2018Cervical cancer—an illness that can be prevented by vaccination against the human papillomavirus (HPV) and that is curable if detected and treated early—is developed by more than 500 000 women each year, half of whom die of the disease. If cervical cancer prevention, screening and treatment efforts are not urgently scaled up, it is projected that this number could double by 2035.
Cervical cancer is an AIDS-defining illness, since women living with HIV who become infected with HPV are more likely to develop pre-invasive lesions that can, if left untreated, quickly progress to invasive cancer—women living with HIV are four to five times more likely to develop invasive cervical cancer. HPV infection has been found to significantly increase the risk of HIV transmission for both men and women.
Thanks to HIV treatment, many more women living with HIV are living long and healthy lives, but it is imperative that women living with HIV do not succumb to other illnesses, including cervical cancer. “It makes no sense to save a woman’s life from AIDS, only to let her die from treatable or preventable cancer,” President George W. Bush, whose George W. Bush Institute is leading efforts to end AIDS and cervical cancer, said in October 2015.
Nine out of 10 women who die from cervical cancer live in low- and middle-income countries. Given that the burden of HIV is primarily felt in low- and middle-income countries, and particularly by adolescent girls and young women, responding to both cervical cancer and HIV together in those countries is vital. Unfortunately, however, most low- and middle-income countries with a high prevalence of HIV have limited programmes for cervical cancer prevention and control.
There is a growing awareness of the need to maximize synergies between the AIDS response and efforts to prevent, diagnose and treat cervical cancer through HPV vaccination, education, screening and treatment. Likewise, existing HIV programmes can play a strategic role in expanding cervical cancer prevention services.
Reducing deaths from cervical cancer requires a wide-ranging approach that includes the following:
- Health education, including age-appropriate comprehensive sexuality education.
- HPV vaccination for adolescent girls.
- Screening all women at risk of developing cervical cancer. Screening programmes should include HIV counselling, testing and treatment, as well as other sexual and reproductive health services and treatment of precancerous cervical lesions and invasive and advanced cervical cancer.
- Ensuring access to palliative care, when needed.
“All women living with HIV need access to information on HPV and should be offered cervical cancer screening and treatment if necessary,” said Michel Sidibé, Executive Director of UNAIDS.
In May 2018, the United States President’s Emergency Plan for AIDS Relief, the George W. Bush Institute and UNAIDS launched a joint effort through a US$ 30 million partnership to accelerate efforts in eight sub-Saharan African countries to ensure that women and girls living with HIV are a priority in national cervical cancer prevention and control programmes.
“Thanks to the generosity of the American people, the United States President’s Emergency Plan for AIDS Relief has saved the lives of millions of HIV-positive women around the world,” said Deborah Birx, United States Global AIDS Coordinator and Special Representative for Global Health Diplomacy, at the launch of the partnership in May 2018. “We must ensure these same women—mothers, daughters, aunts and grandmothers—who are living with HIV and thriving do not succumb to cervical cancer.”




Feature Story
The need for a holistic approach to women and HIV
16 March 2018
16 March 2018 16 March 2018It has long been recognized that the response to HIV can’t exist in isolation, but must be integrated within a broader health and development agenda. A daylong event set out to understand better how three areas critical to women living with HIV—cervical cancer, hormonal contraception and female genital schistosomiasis (FGS)—intersect.
The importance of taking a holistic approach to girls and women and their sexual and reproductive health and rights was a central theme of the event. Held on the sidelines of the 62nd session of the Commission on the Status of Women, the event highlighted the possibilities of recent technological and medical advances to improve women’s health.
Setting the scene, Ebony Johnson, from the Global Coalition on Women and AIDS, said, “Too often women are unheard, forgotten, underserved, improperly researched—I invite and implore you to go in a new direction so that change truly comes.”
Women living with HIV are more likely to have the human papillomavirus (HPV) and are five times more likely to develop cervical cancer, which kills approximately 250 000 women each year. To emphasize the scale of the problem, Vikrant Sahasrabuddhe, of the National Cancer Institute, United States National Institutes of Health, noted that, “In the past 20 minutes of the presentation, 20 women were newly diagnosed with cervical cancer and 10 women died from cervical cancer.”
A disease that mostly affects low- and middle-income countries, where 90% of all new diagnoses and deaths occur, cervical cancer is, however, preventable through the HPV vaccine and treatable if diagnosed early.
New technology has been developed to screen women for HPV DNA or tell-tale proteins that are the signs of cervical cancer. And new tools are allowing early treatment even in clinics with limited resources. The event heard how global partnerships, including the United Nations Joint Global Programme on Cervical Cancer Prevention and Control, which UNAIDS is a part of, are committed to reducing the burden of disease, and how national HIV programmes are at the forefront of efforts to roll-out these new services to women living with HIV in order to lessen the toll that cervical cancer continues to take worldwide.
While giving women the opportunity to control how many children they have, and when, concern has been raised about long-lasting injections of a progestogen, specifically depot medroxyprogesterone acetate (DMPA). Studies have suggested that DMPA may be associated with an increased risk of HIV acquisition. Currently, more than 150 million women worldwide use hormonal contraception and there is a high proportion of women using injectable hormonal contraception in sub-Saharan Africa, where there is also high HIV incidence.
A large-scale trial—the Evidence for Contraceptive Options and HIV Outcomes (ECHO) study—which is hoped to settle the uncertainty of DMPA use and HIV risk association, is ongoing. The difficult decisions that will need to be made should the study confirm the elevated risk for HIV from the use of DMPA were discussed by the participants —the decisions will clearly have to be balanced against the known benefits of a highly effective contraceptive and will affect millions of users.
“Both HIV and unintended pregnancy remain global health priorities. As we discover the potential risk of hormonal injectable contraceptives for HIV acquisition, women need accurate information to be able to exercise informed contraceptive choices,” said Nelly Rwamba Mugo, from the Kenya Medical Research Institute.
FGS, also known as bilharzia, is a disease that is often neglected, but affects some 55 million girls and women. With FGS, bleeding during sex results from lesions in the vaginal walls and ulcers in the cervix. These lesions put women who live with FGS at a higher risk of contracting HIV. However, cheap and effective treatment in childhood of girls who are infected with the parasite that causes FGS can stop its development later in life.
“Genital inflammation increases the risk of HIV acquisition. We need more research on coinfections, treatment of schistosomiasis and related HIV prevention strategies to help form policies that protect women’s health,” said Pragna Patel, from the United States Centers for Disease Control and Prevention.
How to scale up treatment and prevention options, and how to ensure synergy between HIV programmes and schistosomiasis control programmes in a country, were key areas of focus during the day’s discussions.
Throughout the day, how to integrate rights, services and HIV was a recurrent theme. Speakers from UNAIDS, the World Health Organization, research centres and hospitals stressed the need to seek out synergies and collaborate in order to build a cross-cutting AIDS response.
“The symposium provided a great opportunity for a wide range of people, from community activists to laboratory scientists and from young students to scientists and experienced policy-makers, to share and discuss their breadth of perspectives,” said Peter Godfrey-Faussett, Senior Adviser, Science, at UNAIDS.
The event, Improving Women’s Health: HIV, Contraception, Cervical Cancer and Schistosomiasis, was held on 15 March at the New York Academy of Sciences in New York, United States of America.


Update
Call to break down silos between HIV and cervical cancer prevention
03 October 2017
03 October 2017 03 October 2017The Executive Director of UNAIDS, Michel Sidibé, has highlighted the urgent need to break down silos and integrate HIV and sexual and reproductive health services, including for the prevention and control of cervical cancer, which is an AIDS-defining illness. Mr Sidibé delivered his message at the International Agency for Research on Cancer in Lyon, France, on 3 October.
Leveraging the experience of more than three decades of the AIDS response, Mr Sidibé called for greater mobilization and the breaking down of silos between programmes, movements and services to deliver comprehensive sexual and reproductive health services for women and girls. He also reiterated the need to engage with civil society.
Women living with HIV have an up to five times greater risk of developing cervical cancer, which is the second most common cancer among women living in low- and middle-income countries. Despite cervical cancer being highly preventable with the human papillomavirus vaccine and generally curable with early diagnosis and treatment, more than 528 000 women are diagnosed with it every year and around 266 000 die needlessly, almost 90% of whom live in low- and-middle-income countries.
During his speech, Mr Sidibé highlighted the immense opportunities provided by the Sustainable Development Goals and the 2016 United Nations Political Declaration on Ending AIDS, as well as the resources made available through the Global Fund to Fight AIDS, Tuberculosis and Malaria, which reflect strong global commitment to scaling up integrated services to address coinfections and comorbidities.
Quotes
“It is an unacceptable tragedy that women are dying from cervical cancer because of where they are born, because they are poor and because they do not have access to the life-saving vaccines, diagnostics and treatment available to girls and women in high-income countries.”
“Chronic infections are associated with around one in six cancers worldwide and more than one in three in sub-Saharan Africa. Working collaboratively in a strategic manner across the HIV and cancer fields offers many potential opportunities to reduce the disease burden in some of the world’s most vulnerable populations.”