
Feature Story
Mountaintop moment: Ensuring a sustainable AIDS response beyond 2030
27 June 2024
27 June 2024 27 June 2024Key figures in the AIDS response came together at the 54th meeting of the UNAIDS Programme Coordinating Board (PCB) to discuss how to ensure that the gains from the HIV response can be sustained beyond 2030.
During the PCB’s thematic segment, participants heard that the aim of sustainability is not to maintain the HIV response in its current form but to ensure the durability of the impact of the HIV response. This will require a shift in focus to long-term sustainability.
“Until there’s a cure or a vaccine, we will need to sustain the AIDS response beyond 2030, in every part of the world, in the north and in the south,” said Winnie Byanyima, UNAIDS Executive Director. “Sustainability is at the heart of the vision of the Sustainable Development Goals (SDGs), with the commitment that the needs of the present are met without compromising the ability of future generations to meet their own needs.”
Remarks echoed by Florence Anam, co-Director of the Global Network of People Living with HIV (GNP+), “People living with HIV will be here in 2031 and beyond so for us the sustainability of the HIV response is a journey of transformation and not a destination with an end date,” she said. “It matters that at the center of this process of change, mechanisms are in place for all who need treatment and prevention services and that this care is inclusive, devoid of stigma and discrimination.”
The strategies and delivery mechanisms required for scaling up prevention and treatment services and to ensure a stable enabling environment to reach the 2030 target will differ from those that will be needed for long-term sustainability. Leveraging societal enablers will be especially critical for sustainability, including minimizing HIV vulnerability and ensuring access to services in future decades. Rather than build incrementally on what is already in place, sustainability will demand transformations in human rights based, people-centred policies, programmes and systems.
In addition, sustainability requires action on the political, financial, and programmatic front – and across sectors. Not only health, but also gender equality and education so that the economic and societal drivers of new infections are tackled.
Michelle Bachelet, former President of Chile, in a video statement, said, “The combination of shared responsibility and country leadership is essential. Developing countries need to own the response and increase their self-reliance but global action is required to create an enabling environment for this to happen.”
Countries are being advised to prioritize the careful and effective integration of the HIV response in national health systems, with appropriate attention to reforms or modifications required for key and vulnerable populations. This transformation will increase efficiency, promote equity, maximize resource utilization and contribute to the dual goal of achieving and sustaining HIV epidemic control and strengthening human rights based, people-centred systems for health.
Together with its co-sponsors, partners such as PEPFAR and the Global Fund, and other stakeholders, the Joint United Nations Programme on HIV/AIDS are supporting countries to develop roadmaps to sustain their national AIDS responses.
"Sustainability road maps are critical, starting with the vision,” said Peter Sands, the Global Fund Director. “Strategic financing then needs to support the path to that vision, focused both on continuing to raise resources as well as using those that are available more efficiently. To optimize HIV and primary health care integration requires well- coordinated partnerships between governments, private sector companies, international organizations, and non-government organizations.”
John Nkengasong, U.S. Global AIDS Coordinator and head of PEPFAR, also stressed that gains in the HIV response are fragile and need to be sustained. "Today we find ourselves at a crossroads to 2030 where we go somewhere or we go nowhere,” he said. “2030 is critical because at that point the global community regardless of where people are sitting, either say we have done our best and we don’t know what else to do or do we say, ‘Yes, we can get to the finish line’...2030 is a mountaintop moment.”
Finally, sustainability will also require adapting measures and approaches in diverse settings, highlighting the importance of tailoring planning and implementation for specific contexts.
Related





Feature Story
Four Albanian cities commit to ending the AIDS epidemic by 2030
19 June 2024
19 June 2024 19 June 2024Four Albanian cities—Kolonja, Durrës, Pogradec, and Shkodra—have signed the Paris Declaration on AIDS committing to ending AIDS as a public health threatby 2030. By signing the declaration, the Mayors committed to achieving the 95-95-95 targets by 2025 and called on other municipalities in Albania, including the capital Tirana, to join this effort.
The Albanian cities are the latest additions to the list of more than 550 other cities around the world that are part of the Fast-Track Cities initiative which aims to fast-track action at local level to improve the quality of life of people living with and affected by HIV.
In order to fulfill their commitments, the cities have developed different plans of action based on their local circumstances. For instance, the Municipality of Durrës plans to increase investments in methadone maintenance therapy, aiming to expand the number of people benefiting from such services by 10% each year.
The Municipalities of Pogradec and Kolonja are focused on raising awareness among migrant populations to increase HIV testing rates in these regions. As border cities with a significant male population migrating for work, ensuring these communities are well-informed and have access to necessary health services is crucial.
Finally, the Municipality of Shkoder aims to foster a partnership with Podgorica in Montenegro to exchange experiences and best practices in developing the "Healthy Houses" model, which has been successful in the neighboring country. The "Healthy Houses" initiative is a free social service providing psychosocial support to citizens. It focuses on improving the quality of life, reducing risks, and offering support to socially vulnerable groups. The service addresses a range of issues, including HIV, domestic violence, addiction, services for LGBTQ+ peopleand others.
Olimbi Hoxhaj, Executive Director of the Albanian Association of People Living with HIV, hopes that signing the Declaration and the follow-up actions will not only help prevent new HIV infectionsbut will also significantly reduce AIDS-related mortality.
Albania has a low HIV-prevalence epidemic but faces an increasing number of new HIV cases. From 1993 to 2023, 1,716 cases were diagnosed, with 113 new cases in 2023 alone. Most HIV testing occurs in the late stages of infection (about 60% of new cases), meaning official figures do not fully represent the actual infection rate.
The Minister of Health and Social Protection of Albania, Ogerta Manastirliu, emphasized that rapid diagnosis and treatment are key. “The whole fight in this aspect is timely diagnosis so that the treatment can start as soon as possible, and the infection is under control.”
“While the European region continues to face political, economic, and healthcare challenges due to regional conflicts, migration, and other complexities, it is important to secure commitment from municipalities to advance progress towards the crucial HIV targets,” said Eamonn Murphy, UNAIDS Regional Director for Asia-Pacific and Eastern Europe and Central Asia.
Technical assistance to all municipalities in developing their local programs was provided through the cooperation between the International Association of AIDS Care Providers (IAPAC), the Fast-Track Cities Institute (FTCI), UNAIDS and the Global Fund’s regional #SoS 2.0 project, which aims to ensure the sustainability of HIV services in 15 countries in Eastern Europe. "Since 2019, with our support, 21 municipalities from Southeast Europe have joined the Fast-Track Cities initiative," said Tetiana Deshko, Director of the International Programs Department at the Alliance for Public Health.
Learn more
Region/country
Related




Feature Story
Splash of colors: Exhibit at UNAIDS headquarters by members of People Living with HIV Geneva Association
17 June 2024
17 June 2024 17 June 2024Propping up her round thick-framed glasses, Carole Perrette readjusted a painting in the art exhibit at UNAIDS headquarters in Geneva, Switzerland. For one month, more than twenty paintings crafted by her art therapy group will grace the sun-smacked lobby.
Ms Perrette, a painter and art therapist, has been leading workshops at the Geneva Association of People Living with HIV/AIDS (PVA) for its members since 2005 (minus a short break to focus on her career.)
She is thrilled UNAIDS is welcoming a selection of her “students’” pastels and vibrant watercolors.
"Completing a piece of artwork is such an accomplishment that this exhibit is an even greater honor,” Ms Perette said.
For painter and PVA member May* the art and painting therapy sessions allow her to feel free.
“We paint, we talk, we express ourselves and it is very liberating...I forget my daily troubles,” she said.
PVA-Geneva offers art therapy sessions weekly to all of its members. For the Director of PVA, the workshops are a key component of the mental health outreach the association does.
“As you can see from the variety of the paintings on display, people express themselves differently... from glorious sunsets to two fish kissing to renditions of blood cells,” said Rocco Senatore.
“Despite this diversity, the art therapy sessions unite the group, and most champion each other’s work,” he said.
Many eagerly attend the workshops because they do not feel judged. Yvan, a painter and PVA member, said he had difficulties coming to terms with his HIV status. “I kept all of this bottled up for a long time. The art therapy is my support network art wise and morally too.”
During a meet and greet session with the artists and UN staff, Mahesh Mahalingam, UNAIDS Chief of Staff, said that art has been used as a longstanding bridge to raise awareness in the HIV response. “Art and artists like yourselves were instrumental in bringing the world’s attention to HIV in ways that has not happened in any other disease,” he said. “Artists have made this disease humane and out of that it led to a movement that pushed for access to treatment for millions of people.”
Nodding approvingly, Dalia, artist and PVA member, turned to the group afterwards and said, “Just like our art therapy sessions, this is what solidarity is all about.”
*Person did not want to disclose full name.
Region/country




Feature Story
UN Plus relaunches to support and advocate for UN workforce members living with HIV
28 May 2024
28 May 2024 28 May 2024UN Plus, the association of United Nations (UN) staff members living with HIV has been re-established.
Originally created in 2005 to advocate for the rights and well-being of UN staff members living with HIV around the world, the association paused its operations in 2021 due to global changes and funding challenges. Now, a newly established nine-member advisory committee from various UN entities and regions around the world is working again to ensure that UN staff members living with HIV have access to medications, health insurance benefits, and mental health support, as well as to actively combat HIV-related stigma and discrimination within the UN system.
“I want to express my gratitude for the admirable work that you are doing to revitalize the UN Plus mission,” said Winnie Byanyima, UNAIDS Executive Director. “Together we can make a difference, let’s ensure a safe, supportive UN environment for all, which must include people living with HIV,” she added.
As part of its revitalization efforts, UN Plus members conducted a global survey in late 2023 to understand the experiences and challenges of their colleagues living with HIV. 74 respondents from diverse backgrounds shared their experiences with stigma, discrimination, and health-related issues.
The survey findings underscored that many UN workforce living with HIV still face workplace stigma and discrimination, which negatively affects their professional opportunities and personal well-being. Mental health concerns were also prominent, often stemming from issues related to their HIV status.
UN Plus will work closely with UN agencies, to develop and implement policies that specifically protect the rights of its staff living with HIV. This includes advocating for non-discriminatory hiring practices and career advancement opportunities.
John (JB) Bryant Collier, Chair of UN Plus Advisory Group stated that UN Plus will address those issues through a comprehensive plan informed by the survey findings. “UN Plus is committed to making UN workforce members living with HIV feel supported and empowered wherever they are in the world,” he said.
UN Plus plans to introduce training programs for UN staff members to raise awareness about HIV and HIV-related stigma and discrimination and mental health issues, as well as the importance of supportive workplace environments.
In addition, UN Plus will work to ensure that UN staff members living with HIV have access to the latest treatments and medications and will set up mechanisms for regular monitoring and reporting on their status and well-being, including periodic surveys and feedback sessions to continually adapt and improve the provision of support services.
The relaunch of UN Plus signifies a strong commitment to improving the work environment and overall well-being of UN workforce members living with HIV, and to ensuring they receive the support and resources necessary to thrive professionally and personally.


Feature Story
Meet Azima: Frontline hero of the HIV response in Uzbekistan
27 May 2024
27 May 2024 27 May 2024Azima has lived with HIV since childhood; she was abandoned by her parents and raised by her grandmother.
Today she is recognized as an inspirational community leader in the HIV response, including for the vital role she has played in tackling stigma as the first young woman in Uzbekistan to disclose her HIV-positive status.
"I am strong. I have a bright future ahead. And I will achieve my goals,” says Azima.
She has faced both positive and negative reactions since her disclosure. Throughout, Azima has remained a committed activist. She is especially thankful to her community of peer support, a group of children and young people living with HIV supported by UNICEF.
“In the end, the energy of the people who supported me was so strong that it helped me rise above other people's criticism,” she said.
As a peer educator, Azima works tirelessly to raise awareness about HIV.
Today, Azima is studying psychology at Fergana State University. This choice of future career was encouraged by her grandmother and inspired by a psychologist who worked in her support group.
Because of her HIV treatment, Azima cannot transmit HIV to her husband. Several months ago, she gave birth to an HIV-free baby girl.
She is thankful for her family. “My husband has always supported me,” says Azima.
Azima’s story exemplifies the progress made in Uzbekistan’s HIV response. Antiretroviral therapy is provided free of charge to all in need in Uzbekistan. The country is also making efforts to ensure all women living with HIV receive timely treatment, so that all babies will be born HIV-free. Coverage of pregnant women who receive antiretroviral treatment to prevent vertical transmission of HIV has been around 98% since 2016, according to the Uzbekistan Republican Center to fight AIDS.
“The rate of vertical HIV transmission in 2023 was 0.2%. We aim to reduce this figure to 0%. The Republic of Uzbekistan is on the verge of receiving an international certificate for the elimination of mother-to-child HIV transmission,” said Bahrom Igamberdiyev, Director of the Republican AIDS Center in Uzbekistan.
The country has approved a "Roadmap for Implementing Measures to Achieve the Validation of the Elimination of Mother-to-Child Transmission of HIV for 2024-2026". This roadmap will be implemented with the participation of all partners, allowing Uzbekistan to reach its goal and obtain validation for the elimination of vertical transmission of HIV. An effective HIV response is a priority for both the government and civil society in Uzbekistan.
However, some critical challenges in the HIV response in Uzbekistan, particularly concerning HIV prevention, which are deeply rooted in societal norms and systemic inequalities.
These, according to the recently released Gender Assessment Report for Uzbekistan, include limits on women's decision-making power, leaving many women dependent on male relatives for important life choices, including healthcare decisions.
Despite the Government’s commitment and legislative efforts to address gender-based violence, underreporting remains a significant issue. The prevalence of early and arranged marriages also contributes to the limited autonomy of women, depriving many of them of educational and economic opportunities and impeding access to comprehensive sexual education. Cultural norms limit open discussions on reproductive health and prevention in many social contexts including family and educational settings.
As a result, the latest survey found that only 14% of women between 15 and 49 years old have comprehensive knowledge about HIV. This reduces to 10% for young women between 15 and 25 years old. “Addressing these systemic issues requires comprehensive efforts to promote gender equality, ensure access to sexual and reproductive health and rights, and empower women economically. UNAIDS is working with partners to improve access to education and create an enabling environment for women to realize their full potential,” said Eamonn Murphy, UNAIDS Regional Director for Asia-Pacific and Eastern Europe and Central Asia.
Azima is stepping up her advocacy role, pointing out that openness and education are crucial in fighting stigma and advancing access to prevention, testing and treatment. She advises young women to disclose their HIV status to partners early in relationships and emphasizes the importance of adherence to treatment and of mutual support within families.
Azima will continue breaking stereotypes, promoting awareness, and embracing her journey with courage and determination. Azima exemplifies the learning that HIV responses succeed when we let communities lead.
Related link
Region/country
Related

Feature Story
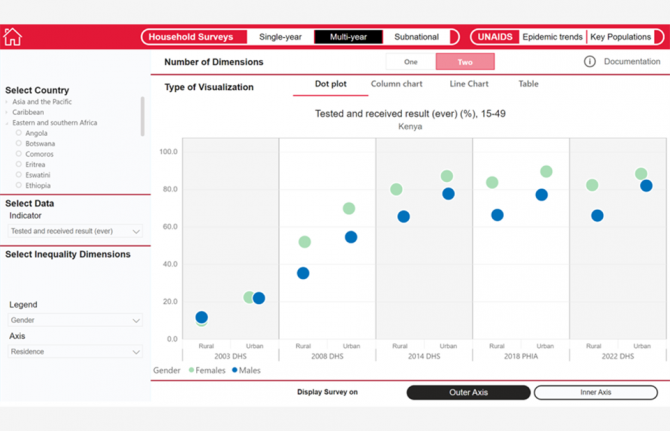
UNAIDS launches inequalities visualization tool
20 May 2024
20 May 2024 20 May 2024Tackling inequalities is how the world will end AIDS, so it is vital to know what type of inequalities exist in each country and how are they affecting the national AIDS responses. That is what a new UNAIDS inequalities visualization tool is set out to measure.
The new tool will allow countries, development partners, civil society, academia, and advocates to see and measure the effects that different dimensions of inequalities have on the HIV response.
“One of the best ways to translate complex data is to show it visually. This tool allows the user to summarize critical inequalities in a snapshot,” said Mary Mahy, Director, Data for Impact Practice at UNAIDS.
Integrated in the UNAIDS AIDSinfo database, which is a repository of all HIV data globally, the new inequality platform brings together data from household surveys like Demographic and Health Surveys (DHS) and Population-Based HIV Impact Assessment (PHIA), plus surveys among key populations and UNAIDS epidemiologicalestimates. The tool measures inequalities by characteristics such as age, gender, wealth, education, geographic location and residence, and allows users to see the combined effects of up to three dimensions of inequality.
Some of the deepest, thorniest pandemic-driving inequalities continue to obstruct progress in the HIV response. Inequalities driving the AIDS pandemic are not inevitable. Policies can overcome them.
For example, in sub-Saharan Africa, adolescent girls and young women are 3 times as likely to acquire HIV as adolescent boys and young men. To help overcome this inequality, countries need to offer prevention services that are adolescent-friendly and targeted at young women at highest risk of HIV acquisition.
Similarly, the new tool shows how access to services differs for residents of urban and rural areas, and how among key populations, younger people usually have lower access to HIV services that their older peers. In Zambia, for example, HIV treatment coverage among rural residents was 9% lower than residents of urban areas. In Malaysia, access to HIV testing among people who inject drugs who were younger than 25 years old was 50% lower than their older peers, and in Thailand, HIV prevalence among male sex workers has been consistently several times higher than female sex workers.
By using the evidence provided by this new tool, countries will be able to identify the inequalities affecting their epidemic and response and make the necessary changes in their policies and programmes to address them. UNAIDS will be updating the data in this tool on an annual basis, allowing countries to measure the effect of their policies and programmes as data become available.
Training videos have been developed to help users learn how to interact with the tool and make the best use of the data available.
Training videos


Feature Story
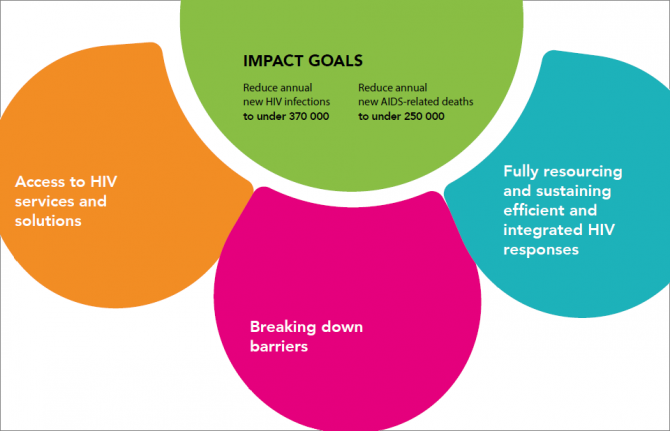
UNAIDS launches new approach to ensure the long-term sustainability of the HIV response
19 January 2024
19 January 2024 19 January 2024As countries work to reach the goal of ending AIDS as a public health threat by 2030, planning is urgently needed for sustaining the gains from the HIV response beyond 2030.
With that in mind, UNAIDS has released the “HIV Response Sustainability Primer” which proposes a new approach to ensure the sustainability of the HIV response. This holistic approach includes programmatic, political, policy-related and financial aspects of the HIV response. The new Primer provides the rationale, the definitions, and an in-depth explanation of this new sustainability approach.
“The moment is right, the imperative is now, the global HIV community must come together to dialogue about what is needed to sustain the HIV response by and beyond 2030,” says Jaime Atienza, Director of Equitable Financing at UNAIDS. “We are calling on leaders to initiate national conversations about the future state of a sustained HIV response, and the transformations needed to achieve and sustain impact, by and beyond 2030, including looking at the policy changes, donor commitment and investments needed to translate them into results and concrete changes at country level.”
The goal of sustainability is not to perpetuate the HIV response in its current form. Rather, it is to ensure the durability of the impact of the HIV response. This will require a shift in focus to long-term sustainability. Transformative action, starting now, will be needed to make this a reality by and beyond 2030.
For instance, the strategies and delivery modalities required for scaling up prevention and treatment services and to ensure a stable enabling environment to reach the 2030 target will differ from those that will be needed for long-term sustainability. Leveraging societal enablers will be especially critical for sustainability, including minimizing HIV vulnerability and ensuring access to services in future decades. Rather than build incrementally on what is already in place, sustainability will demand transformations in human rights based, people-centred policies, programmes and systems.
Sustainability will require different measures and approaches in diverse settings, highlighting the importance of tailoring planning and implementation for specific contexts. Therefore, this Primer outlines a new approach to planning for and implementing sustainable national HIV responses—to reach global AIDS targets and maintain the gains of the HIV response beyond 2030.
Through country driven and owned processes that leverage specific data, countries will develop HIV Response Sustainability Roadmaps which will chart the pathways for country level strategies and actions to achieve and sustain impact, leaving no one behind. The stages and ways of developing these Roadmaps are also contained in the “HIV Response Sustainability Primer”.
The Sustainability Roadmap will be distinct from, yet complimentary to, National Strategic Planning exercises (NSPs). Each country’s Roadmap should be a living document, allowing for the continual reassessment and evolution of HIV interventions, programmes and policies as contexts and circumstances change.
As a key transformation required for long term sustainability, countries are advised to prioritize the careful and effective integration of the HIV response in national systems, with appropriate attention to reforms or modifications required for key and vulnerable populations. This transformation will increase efficiency, promote equity, maximize resource utilization and contribute to the dual goal of achieving and sustaining HIV epidemic control and strengthening human rights based, people-centred systems for health.
The process for developing the HIV Response Sustainability Roadmaps is aligned with the principles, goals and targets set out in the Global AIDS Strategy 2021–2026 and in the 2021 Political Declaration on Ending AIDS. International partners will support country driven processes through the provision of technical support, including a series of resources described in this Primer.
The proposed new approach to sustainability outlined in this newly released Primer will require all participants, including international actors, to be ready to undergo transformations on the way they have been carrying forward the response to better prepare for the post 2030 world.
To support such actions, sustainability will be at the top of UNAIDS priority agenda in 2024. Together with its co-sponsors, partners such as PEPFAR and the Global Fund, and other stakeholders of the Global HIV community, UNAIDS is resolute in its commitment to supporting countries leverage the tools and analytics, the lessons learned, the science of what works where, to foster open and honest dialogue on the future of the HIV response, the transformations needed to ensure that responses across the globe are not in danger of putting millions of lives and livelihoods at risk and the financing commitments needed for scale and impact.
Resources
Related


Feature Story
UNAIDS – planning for sustainability of the HIV response up to and beyond 2030
30 April 2024
30 April 2024 30 April 2024There are more people than ever before living with HIV and in need of lifelong treatment (39 million in 2022), with this number set to rise in the coming years. Ensuring long-term resourcing is vital.
However, resources for HIV are severely constrained. In 2022, US$ 20.8 billion was available for HIV programmes in low- and middle-income countries––2.6% less than in 2021 and well short of the US$ 29.3 billion estimated to be needed by 2025. In addition, UNAIDS estimates that in 2022 there was a 90% shortfall in funding for HIV prevention among key populations most affected by HIV, including men who have sex with men, sex workers and people who inject drugs.
As countries work to reach the goal of ending AIDS as a public health threat by 2030, planning is urgently needed to protect and build on the HIV gains made to date, increase efforts to reach people most affected by HIV, and to sustain the HIV response into the future.
This is why UNAIDS has developed an HIV sustainability framework which includes transformations in policy, programmes and systems to sustain the HIV response beyond 2030. To ensure success in sustaining the HIV response, UNAIDS is supporting all stakeholders on long-term planning.
“As the global community pushes towards the ambitious goal of ending AIDS as a public health threat by 2030, a crucial conversation is needed now on how to sustain the hard-won gains of the HIV response well beyond 2030,” said Winnie Byanyima, Executive Director of UNAIDS. “A paradigm shift is needed to ensure the long-term sustainability of the HIV response, a journey that demands transformative action starting today.”
To support countries and partners in implementing the Sustainability Framework as outlined in the UNAIDS HIV response sustainability primer, UNAIDS has released a new Companion Guide which includes country-specific analytical resource packages and a sustainability assessment tool. These resources will serve as tools to help countries and partners develop roadmaps and navigate the path towards sustainability.
The companion guide offers flexible stepwise methodology, allowing each country to tailor the sustainability framework to its unique context. With practical tools and insights, it serves as a compass for initiating and guiding the roadmap development process.
“Developing sustainability roadmaps is key to the HIV sustainability framework and will empower countries to navigate the complex terrain of sustainability,” said Angeli Achrekar, Deputy Executive Director for Programme, UNAIDS.
The country analytical resources package features granular data tables, graphics, and essential fiscal and macroeconomic metrics, broader health system analytics and additional qualitative information. The package serves to facilitate sustainability dialogues essential for planning that fits each country's epidemic characteristics and broader economic and health system landscape.
Central to this journey is also the sustainability assessment tool. This tool empowers stakeholders to identify and address risks across political, structural, financial, and programmatic domains. It also facilitates the discovery of new strategies to enhance the HIV response and drive continuous improvement towards 2030 and beyond.
“Through its intuitive interface, the sustainability assessment tool will help countries understand how to ensure that their HIV response is sustainable – identify the big milestones needed and to organize how to get there,” said Christine Stegling, Deputy Executive Director, Policy, Advocacy and Knowledge Branch, UNAIDS.
Sustainability to 2030 and beyond will require strong political leadership across multiple sectors, and the active engagement of people living with HIV and of key and vulnerable populations. Resources will need to be mobilized from both domestic and international sources, and flexibility and resilience will be required as epidemics evolve, and shifts occur in changing economic, political and social contexts.
UNAIDS will work side by side with countries and partners to enable them to successfully implement the new sustainability framework, so that all people living with and affected by HIV can continue accessing the lifesaving HIV services they need, have their rights protected, and be able to thrive.
Related





Feature Story
How communities led in the HIV response, saving lives in Eswatini at the peak of a crippling AIDS epidemic
25 April 2024
25 April 2024 25 April 2024This story was first published by News24.com
Eswatini is one of the countries which has been most affected by HIV. At the peak of the epidemic in 2015, almost one out of three people were living with HIV. In 1995, when there was no antiretroviral treatment for people living with HIV, 73 000 people were living with HIV. 2400 people died of AIDS that year. Worried about the rising number of infections and deaths, communities of people living with HIV mobilized to press that antiretroviral treatment be made available for people living with HIV.
One of the key campaigners for access was Hannie Dlamini. Dlamini is now 50 years old and has been living with HIV for 32 years, after finding out about his HIV positive status at the age of 18. He was one of the first people in Eswatini to publicly declare his positive HIV status in 1995 at a time when the stigma and misinformation around HIV was rife.
Dlamini rallied together other people living with HIV as well as non-governmental organizations working to end AIDS in Eswatini, to ensure that everyone living with HIV and in need of treatment had access to it. They formed a community-led organization called Swaziland AIDS Support Organization (SASO) as a support group for people living with HIV. SASO also provided healthy living information for people living with HIV.
“When we asked the government [in 2002] for ARVs in Eswatini we did a pilot project with NECHA [National Emergency Response Council on HIV/AIDS], to see if people would use the drugs.” Dlamini says the response was overwhelming, with many people keen to start the lifesaving treatment. “We initially planned to enrol 200 people on treatment but the demand was 630.” said Dlamini.
Today, Eswatini is one of the countries which has achieved the ambitious 95-95-95 targets (95% of people living with HIV who know their HIV status, 95% of people who know that they are living with HIV are on life-saving antiretroviral treatment, and 95% of people who are on treatment are virally suppressed). This achievement has put the country a step closer to ending AIDS as a public health threat, thanks to the work of community-led organizations, authorities and global partners like UNAIDS, the United States President's Emergency Plan For AIDS Relief (PEPFAR) and the Global Fund to fight AIDS, TB and Malaria who are working with the government and local communities to end AIDS.
Eswatini’s HIV response strategy includes ongoing nationwide testing and treatment campaigns, use of self-testing kits to encourage more people to take up testing at the comfort of their homes, antiretroviral treatment, male circumcision and pre-exposure prophylaxis (medicine to prevent HIV) and other prevention measures. Community organizations such as Kwakha Indvodza are also key in encouraging men to take full responsibility for their wellbeing and reducing toxic masculinity and gender-based violence which are some of the drivers of HIV.
The driving role of communities in Eswatini to end AIDS is acknowledged by the health authorities. According to Dr. Michel Morisho, HIV management specialist at Mbabane Government Hospital, the government “could not have achieved the 95-95-95 without communities.”
Dr. Morisho says as part of the country’s strategy to end AIDS, HIV testing and treatment are part of disease management for every patient who presents at health facilities for any illness. “When people come to the hospital for whatever, or check up, we offer an HIV test to allow them to know their HIV status,” he said. Dr. Morisho added that treatment is important to bring down viral load and is helping people living with HIV to stay healthy. Eswatini is striving to achieve 100-100-100 [in the number of people who know their HIV status, are on treatment and are virally suppressed].” People who are virally suppressed cannot transmit HIV, thus helping in HIV prevention efforts.
Young women living with HIV have also stepped up to fight the spread of HIV in the country, volunteering their time as peer educators to educate young people about HIV and supporting people newly infected to stay on treatment to live healthily and long lives. Ntsiki Shabangu is a 28-year-old young woman living with HIV. She was diagnosed with HIV in 2015, at the age of 19. She opened up about her status in 2017 and is now working with the Eswatini Network of Young Positives, a local non-governmental organisation working to end AIDS among young people providing counselling and HIV awareness training . Ntsiki believes that: “When you share your story, you bring hope to young people.”
While Eswatini is on the path to end AIDS, the country is facing other health burdens associated with aging, including non-communicable diseases such as diabetes and cancer. People living with HIV are not often more affected by these illnesses. Some people living with HIV in Eswatini have developed these comorbidities, which presents the need for the strengthening of the healthcare system to provide easily accessible holistic disease management and treatment along with HIV services to improve the quality of life for people living with HIV. As Thembi Nkambule, a woman who has been on HIV treatment for more than 20 years said: “Most of us are sick. Most of us are presenting with kidney issues. We are presenting with hypertension; we are presenting with sugar diabetes. We have a lot of issues.”
To protect the gains that have been made against HIV in Eswatini, the government should invest more resources in building a resilient healthcare infrastructure to strengthen the system to better meet the health needs of people living with HIV and to prepare for future pandemics. Community-led organisations should also be placed at the centre of HIV response and supported, both financially and politically, to reach more people who need HIV services to end the epidemic by 2030 as a public health threat.
Region/country
Related




Feature Story
Navigating HIV services during migration crisis in Eastern Europe and Central Asia
17 April 2024
17 April 2024 17 April 2024Countries affected by the migration crisis in Eastern Europe and Central Asia, prompted by the war in Ukraine and other turmoil in the region, have had to put in place measures so that all displaced people have access to essential HIV services.
Key Figures:
- In 2022, Europe was confronted by the largest refugee crisis since World War II.
- As of February 2024, nearly one-third of Ukraine’s population remains displaced, with 6.3 million Ukrainian refugees globally, primarily concentrated in Europe, 62% of them are women.
- In 2022, around one million Russian citizens emigrated, with many choosing prolonged stays abroad.
- Central Asian countries witnessed the biggest influx of international migrants since their independence.
- Up to 300,000 Belarusians left their country since May 2020.
- Migration from Central Asia to Russia surged in 2023, with notable increases in Uzbek, Kyrgyz, and Tajik nationals entering for work purposes. (ICMPD Migration Outlook Eastern Europe and Central Asia 2024)
- The HIV epidemic is growing in Eastern Europe and Central Asia, with Russia, Ukraine, Uzbekistan, and Kazakhstan accounting for 93% of new infections in the region combined.
Surviving the devastating events of March 2022 in Mariupol, Ukraine, uncertain of what the future held, Svetlana fled her hometown.
"Mariupol was a scene of utter destruction. I had a packed suitcase, but I left it behind, only taking with me a dog and a cat," recalls Svetlana. "With assistance, we managed to reach the Polish border, eventually finding refuge in Lithuania."
Living with HIV since 2000, Svetlana relies on anti-retroviral treatment (ARV) to keep the virus at bay by taking a tablet a day. In haste, she had only taken one pill box.
Upon her arrival in Lithuania, she connected with an online organization that within days helped her to obtain her life-saving medicine from a doctor.
Svetlana is one of 70 participants in 6 countries in the Regional Expert Group on Migration and Health (REG) study that assessed the healthcare access for Ukrainian refugees using qualitative methods. According to Daniel Kashnitsky, the lead REG expert, “insights from specialists and service recipients revealed that all HIV-positive refugees had access to treatment across EU host countries.”
After recovering from the initial shock, the European Union activated the Temporary Protection Directive, establishing legal guidelines for managing mass arrivals, offering humanitarian aid, and ensuring access to life-saving antiretroviral treatment and basic HIV services to those in need.
Outside the EU, in countries like Moldova and Georgia, special regulations ensure free access to HIV services. Moldova's National AIDS Coordinator, Yuri Klimaszewski, underscored that Moldova provided HIV services to refugees like it does for its citizens.
The study also revealed that some refugees struggled in host countries, leading to challenges maintaining treatment adherence. Tatyana (name changed) left Odessa along the Black Sea in April 2022.
But she returned home because she could not find adequate support under the opioid maintenance therapy program in Poland. She found it complicated to reach the service point, the language barriers prevented her from communicating her needs with medical staff, and she lacked community support.
“Despite the unprecedented support shown by European countries to Ukrainian refugees, systemic issues, particularly bureaucratic complexities, require proactive intervention by social workers, community organisations and volunteers to effectively address these challenges,” said Mr Kashnitsky. Additionally, he added, “there is a pressing need to tackle the stigma faced by people living with HIV and other key populations, such as people who use drugs.”
Uladzimir, who left Belarus for Poland in the first days of the war in Ukraine, needed about a month to start receiving ARV treatment. First, he had to obtain "international protection", then confirm his HIV status and wait for an appointment with a doctor. But once all that was cleared, he had access to all the necessary services. For many accessing services is not as straightforward as it is for Ukrainian refugees, according to the REG study “Forced migrants with HIV status: social psychological and medical aspects of adaptation”
Legislation in some countries makes accessing HIV prevention and treatment for migrants challenging. And in some cases, national healthcare systems may lack resources to meet the influx of people and their needs.
As the Russian Federation continues to deport migrants living with HIV, those who remain in Russia due to the inability to return home or for family reasons are compelled to stay in the country illegally. They are deprived of HIV treatment and health services. Some have succeeded by receiving treatment remotely (ARVs sent to them with the help of countries of origin).
Recommended strategies, as outlined by the REG study, include improving the system of informing people about potential risks and available HIV services abroad, establishing health insurance protocols, and supporting community organizations that provide HIV services.
Removing legal provisions that discriminate against migrants living with HIV will also reduce barriers to accessing antiretroviral therapy, resulting in significant improvements for public health in the region.
Eamonn Murphy, UNAIDS Regional Director for Asia Pacific and EECA regions, praises the collaborative efforts involving various stakeholders, including governments of countries of origin and host countries, community organizations, the Joint UN Programme on AIDS, and donors.
However, he says more needs to be done. “There is an urgent need to work on the legalization and standardization of such approaches to ensure all people on the move can access essential services and remain on treatment wherever they are.”
Region/country
- Eastern Europe and Central Asia
- Albania
- Armenia
- Azerbaijan
- Belarus
- Bosnia and Herzegovina
- Bulgaria
- Croatia
- Cyprus
- Czechia
- Estonia
- Georgia
- Hungary
- Kazakhstan
- Kyrgyzstan
- Latvia
- Lithuania
- Montenegro
- Poland
- Republic of Moldova
- Romania
- Russian Federation
- Serbia
- Slovakia
- Slovenia
- Tajikistan
- North Macedonia
- Türkiye
- Turkmenistan
- Ukraine
- Uzbekistan













