

Feature Story
Seeking justice for HIV-related discrimination in the workplace in Guatemala
18 December 2023
18 December 2023 18 December 2023In the heart of the bustling Guatemala City, Juan used to face the daily grind of life with an unwavering spirit. He had been diagnosed with HIV several years ago and had learned to manage his health effectively. As a dedicated employee at a marketing firm, he poured creativity into every project he touched.
Life seemed to be on an upswing for him until an unexpected turn of events unfolded at the workplace. A colleague stumbled upon Juan's medical records and, in a breach of privacy, discovered his HIV status. Soon, whispers spread through the office, and Juan began to feel the cold stares and hushed conversations whenever he walked by. Ultimately, he was dismissed from his company for "restructuring reasons."
As the discrimination became more blatant, Juan decided it was time to take action. He sought advice from Líderes Profesionales, a network of lawyers specializing in discrimination cases for people living with HIV. With UNAIDS's support, this network is committed to fighting for justice and equality for marginalized communities.
Upon hearing Juan's story, the lawyers at Líderes Profesionales were appalled by the flagrant violation of privacy and the subsequent discrimination. They quickly assembled a legal team dedicated to ensuring justice for Juan. The lawyers explained the legal protections in place for individuals with HIV, emphasizing that workplace discrimination based on health status is a clear violation of the law.
Together with Juan, the legal team initiated a lawsuit against the firm. They filed a complaint citing violations of privacy, discrimination, and failure to provide a safe and inclusive work environment and asked for payment of benefits and compensation for unjustified dismissal.
Líderes Profesionales worked tirelessly to expose Juan's unjust treatment, seeking justice for him and advocating for broader change in workplace policies. They organized workshops to sensitize companies, urging them to implement comprehensive diversity and inclusion training and policy.
As of December 2023, the case is still ongoing. The legal team's goal is to seek compensation for Juan and foster an environment where such discrimination would not be tolerated in the future.
"Juan's experience and five other discrimination-related workplace cases this year inspire us to continue our advocacy work," says Julio Rodríguez, Director of Líderes Profesionales. "We redouble our efforts to support individuals facing discrimination, using each case as an opportunity to raise awareness and push for systemic change."
In Guatemala, 31,000 people are estimated to be living with HIV. HIV-related stigma and discrimination are still pervasive. According to the latest National Stigma Index (2017), 14% of people living with HIV reported losing their job or source of income due to their positive status for HIV, and 13% of people living with HIV reported being denied employment or opportunity to work because of HIV.
"Having access to legal support really represented a turning point for Juan. Empowered by it, he is a more vocal advocate for HIV awareness and anti-discrimination efforts," says Marie Engel, UNAIDS Country Director for Guatemala, Honduras and Nicaragua. "Through his journey, Juan contributes to a more just and inclusive society for all."
Let communities lead
Region/country


Feature Story
Responding to gender-based violence through sorority and information
15 December 2023
15 December 2023 15 December 2023In the quiet corner of a community center in Guatemala City, 29-year-old Emma - fictitious name - sits among other women she does not know. In the faces and gestures of each of them, you can see that they all carry the weight of violence and injustice on their shoulders.
The first subtle rays of sunlight gradually fill the room; calm and comfort invite Emma and the others to feel more relaxed in their hearts and souls. With tired eyes, small hands, and a heart scarred by violence, she looks around, absorbs the energy of the place, and takes a deep breath as she awaits the start of a therapy session and an informative talk about HIV.
As the therapy session began, Emma shyly and cautiously shared her experiences with Wendi Polanco, who, since 2019, has become a helping hand for many women battered by gender-based violence. Through Latiendo Juntas, the organization she leads in Guatemala, Wendi clearly proves that sisterhood works and is transformative.
With support from UNAIDS, Latiendo Juntas coordinates a project to improve access to comprehensive health services, including sexually transmitted infections (STI) and HIV testing and care for women survivors of violence. They also contribute to their resilience and empowerment by raising awareness of human rights, including their sexual and reproductive rights, through group therapy and HIV information talks, which provide facts and a platform for open dialogue, fostering a non-judgmental environment.
"The room becomes a sanctuary where the pain of women like Emma and so many others is recognized," says Wendi. "The community center is a refuge for them, and a network of support among the women is woven with the sun's warmth. I feel relieved when I see how the weight on their shoulders begins to lessen."
Throughout these therapy sessions, Emma and other women discover comfort and empowerment. The therapeutic journeys offered at Latiendo Juntas become a catalyst for their resilience, liberation, and self-care.
The link between HIV and violence against women is a widespread problem, as gender-based violence increases women's vulnerability to HIV infection. Women who experience violence may have difficulty negotiating safe sexual practices, including the use of condoms, which increases their risk of contracting HIV. In addition, fear of violence may deter women from seeking HIV testing, treatment, and support, perpetuating the cycle of violence and silence and limiting their access to critical and essential healthcare resources.
Violence against women in Guatemala is endemic and can be described as a shadow pandemic. The country has one of the world's highest rates of femicide: the intentional murder of women because they are women.
"Addressing the intersection of HIV and violence against women requires comprehensive efforts that include education, empowerment, and dismantling gender-based power imbalances," says Irene Izquieta, UNAIDS Advisor on Rights and Gender for Guatemala, Honduras, and Nicaragua.
Let communities lead
Region/country
Related




Feature Story
UNAIDS commemorates World AIDS Day in Berlin alongside communities delivering life-saving HIV services in Germany and Ukraine
30 November 2023
30 November 2023 30 November 2023Since the beginning of the war in Ukraine, communities of people living with and affected by HIV have been at the forefront of ensuring the continuity of life-saving HIV services, both for those who remained in Ukraine and for those arriving in Germany as refugees.
At a special World AIDS Day event in Berlin co-hosted by UNAIDS and 100% Life Ukraine, community representatives and civil society activists thanked the German government and UNAIDS for their support and spoke about the continued challenges they face.
“Our journey exemplifies how the strength of perceived minorities and real community leadership can drive life-saving programmes and innovations that can impact the lives of millions of people,” said Valeriia Rachinska, Director of Human Rights, Gender and Communities at 100% LIFE Ukraine. “None of this would be possible without the support of international partners and donors. Global solidarity and support from our partners are the chance for a fair and thriving tomorrow for all, especially those living with HIV.”
100% LIFE is the largest patient-led organization in Ukraine which has as its mission to fight for life. The Network works with patients and for patients, including the representation of the interests of people living with HIV in 25 regions of Ukraine.
Since the beginning of the war in Ukraine, Germany has donated €1,050,000 in emergency funding to UNAIDS, empowering the provision of critical support to people living with and affected by HIV in Ukraine, Poland and Moldova. This includes providing temporary accommodation, humanitarian assistance, social protection, primary health care and testing for HIV, hepatitis C, STIs and tuberculosis. The emergency fund also covered the enrollment of people in HIV prevention and treatment programmes, offering comprehensive care and support.
Among the speakers at the World AIDS Day event was Silke Klumb, CEO of the German AIDS Federation, who underlined the importance of the partnership between government and civil society in ensuring continued access to HIV prevention, treatment and care services for people affected by the war in Ukraine.
"Community-led responses have been and continue to be critical in the HIV response, both in Germany and globally. Thanks to public funding Deutsche Aidshilfe has been able to engage in community-led prevention, counselling, testing, care, and support for 40 years now. Upon this foundation and through the broad network in Ukraine, Eastern Europe and Central Asia, Germany’s community-led organizations under the umbrella of Deutsche Aidshilfe were able to act immediately to Russia’s full-scale invasion of Ukraine,” said Ms Klumb. ”Over the last 18 months, we provided support, information, translations to people fleeing the war and linked them to care. Platforms such as self-help conferences and other meetings helped to strengthen the communities of people living with and affected by HIV. Deutsche Aidshilfe is committed to continue putting the communities at the centre of our work.”
During the event, UNAIDS Deputy Executive Director of Policy, Advocacy and Knowledge, Christine Stegling, presented the new UNAIDS World AIDS Day report Let Communities Lead. The report shows how communities have been the driving force for progress in the global fight against HIV. It shows that investing in community-led HIV programmes can have transformational benefits.
“Since the earliest days of the AIDS pandemic, community leadership has driven life-saving access to HIV treatment and prevention. Continued progress against HIV/AIDS in Ukraine - despite the war and its resulting refugee crisis - is the direct result of Ukrainian and German community leadership. A community-led response is well-positioned to maintain continuity of HIV prevention and treatment services, especially in times of crisis,” said Ms Stegling. “Continuity of HIV care is essential for achieving our ultimate goal of ending AIDS as a public health threat by 2030. UNAIDS thanks all community leaders who stepped up in these challenging times and we thank nations like Germany who understand the value of investing in a community-led response to HIV/AIDS - especially in times of war and other crises.”
The event was moderated by Peter Wiessner of Action against AIDS Germany.
Related


Feature Story
Holy Disrupters: Interview with Reverend Godson, Presiding Bishop of the Methodist Church of Togo
17 November 2023
17 November 2023 17 November 2023Holy Disrupters: Interviews with Religious Leaders and advocates on HIV and Compassion
Reverend Godson Dogbéda Téyi LAWSON KPAVUVU, Presiding Bishop of the Methodist Church of Togo
UNAIDS speaks to Reverend Godson about his work on HIV and about some of the challenges he is facing
What was your experience working on HIV in the early days?
I had been studying abroad and when I came back in 1992I found that members of my community were dying. But people weren’t talking about what was causing it, they were giving it nick names. It was of course AIDS. During a pastoral meeting I spoke with the Bishop who told me, ‘young man, this thing is a sin, you can’t talk about it openly here, the community won’t accept it’.
This was until two or three years later when some of our colleagues from the church became sick and were dying of AIDS. I went back to the bishop and said now we have to talk about HIV. So, I created a small group and I joined up with the association of people living with HIV in Lomé – it was a safe space where people living with HIV could speak openly.
“Young man this thing is a sin, you can’t talk about it openly here, the community won’t accept it.”
We began to advocate with the government, working with the association and with churches and religious leaders in the country. But theologically, HIV was still spoken about as a sin, so if theologically the narrative isn’t correct, it will damage the whole process. So we corrected the narrative to make it clear that HIV is a virus, not a sin. This was the starting point.
“HIV is a virus, not a sin - this was the starting point.”
From then we created small teams within the communities to support people living with HIV and especially to support the families. To break down the stigma we had to start with the families and then the communities. We published books for academics so they could use them to teach, and we trained the young pastors.
Your work with key populations is well known – how did this come about?
I realized the importance of working with key populations when my uncle died in 2000. He was a gay man who contracted and died of AIDS. I drew on my personal experience with my own family to start working with key populations.
“My uncle died in 2000. He was a gay man who contracted and died of AIDS.”
Today the government has put in place a framework to ensure that everyone living with HIV has access to treatment, but there is still a lot of stigma and discrimination. The loudest voices who have been speaking out are women, the mothers who are saying these are our children, how can we discriminate against our own children. So, we have engaged them in our efforts to break down the stigma around HIV and around key populations.
How has your work changed today?
Treatment is there, Togo has a plan for treatment and treatment is free of charge. But a real issue is adherence and how people can maintain their treatment within the communities amidst the ongoing stigma. We are training mentors and supporting volunteers to encourage people to stay on treatment. It’s how best to support people in their families and within their communities.
“Togo has a plan for treatment and treatment is free of charge. But a real issue is adherence”
The human and social dynamics around HIV in Africa are complex. We have three generations now of children who are living with HIV, many who have been orphaned because of epidemic and having to explain to them that their parents loved them and didn’t want to pass on the virus, this can be hard. I have had experience with young people who have attempted to take their own lives because it’s too much for them, and we are there, the church is there to support them.
“I have had experience with young people who have attempted to take their own lives because it’s too much for them”
We are due to end AIDS among children in Africa by 2025 but to do this we are facing many challenges, not just access to testing and treatment, it’s about poverty, local contexts, social conflicts, military coups and migration. But if you put paediatric HIV at the top and give faith leaders the opportunity to organize women’s desks and children’s activities around that we can start educating children and young people about HIV, how to prevent it and they can have their own language to communicate among themselves.
I’m asking my colleagues from the religious communities to come to the forefront of the fight against AIDS and to integrate HIV into their messages especially around ending AIDS among children in Africa.
Region/country
Related
 Impact of US funding cuts on HIV programmes in Togo
Impact of US funding cuts on HIV programmes in Togo

03 April 2025


Feature Story
Holy Disrupters: Interview with Professor Mohamed Karama, working with Islamic Relief on the HIV programme, Kenya
15 November 2023
15 November 2023 15 November 2023Holy Disrupters: Interviews with Religious Leaders and advocates on HIV and Compassion
Professor Mohamed Karama, working with Islamic Relief on the HIV programme, Kenya
UNAIDS speaks to Professor Mohamed Karama about confronting stigma and his concerns for the future
How has the faith community engaged in the response to HIV?
I am a researcher with the Kenya Medical Research Institute and my background is from the Muslim community. Faith communities have become increasingly engaged, first with HIV then with COVID, and now the faith community are part and parcel of not only health but many other government programmes.
How big of a problem is HIV-related stigma among the Muslim community and how do you deal with that?
Stigma has been very high amongst Muslims because for many years there has been a misconception that HIV is one of the punishments for wrongdoing.
To address the challenges of stigma we have had to address it from the Islamic scriptures and from the teachings of faith. This is what we have been doing for the last few years, and although stigma still remains, we have been able to break down some of the barriers this way.
“For many years there has been a misconception that HIV is one of the punishments for wrongdoing”
We have been teaching how God prohibits judgement of others, we should never see ourselves as holier than others and we should support the sick. From the Islamic scriptures God says, “I was sick, you didn’t visit me, I was hungry, you didn’t feed me, I was undressed, you didn’t clothe me.” And the people reply, “but you are God how can we do that?”
God says “Your brother was sick, you never visited him, if you had visited him you would have found me there. Your brother was naked, if you had clothed him you would have found me there, your brother was hungry, if you had fed him you would have found me there.” Allah says have mercy on those who live with you on earth so that he the great can have mercy on you as well.
These teachings are very strong, they discourage stigmatization, they discourage looking negatively at the sick, any sickness, HIV included.
What’s the biggest challenge you are facing in Kenya at the moment?
Young people 15 to 24 are sexually very active and increasingly liberalized, unlike before where social containment was very heavy, now it’s no longer the case. So we have to reactivate our HIV prevention programmes and re-strategize how to deal with these new dynamics.
What concerns you about the future?
I want to start with PEPFAR (the United States President's Emergency Plan for AIDS Relief), I’m an epidemiologist and I think that if we slack a little we are likely to lose the momentum, and losing the momentum might be too expensive to rebuild—too expensive to rebuild the motion and to sustain the momentum. The progress we have made in the last 40 years cannot be lost, so much has been achieved to date we mustn’t lose it.
“Losing the momentum might be too expensive to rebuild”
(concerning the reauthorization of PEPFAR)
What can the United Nations do better?
The United Nations also needs to work more closely together as partners with the faith-based community, the technical experts and the researchers. That way not only can we address HIV, but we can also address other pandemics that are likely to come in the future.
Region/country


Feature Story
Holy Disrupters: Interview with Thabo Makgoba, Archbishop of Cape Town
13 November 2023
13 November 2023 13 November 2023Holy Disrupters: Interviews with religious leaders and advocates on HIV and compassion
Thabo Makgoba, Archbishop of Cape Town
UNAIDS speaks to the Archbishop of Cape Town, Thabo Makgoba about his work on HIV and his hopes for the future
What was your experience working on HIV in the early days?
I first started working on HIV in around 1998 when I was a rector in Johannesburg and it was a scary time, I remember the South African television adverts saying ‘AIDS kills’ with a coffin that banged—we were all terrified. Everyone was scared, there was a lot of stigma, parishioners were also dying from fear and lack of knowledge.
"There was an immense fear that life had come to an end…."
Through Archbishop Desmond Tutu and others we knocked on every door and established the Anglican Church of Southern Africa’s AIDS programme called ACSA. We hit the ground running but there was an immense fear that life had come to an end….
How has your work changed today?
Today our work has evolved—from fundraising, to incorporating HIV messages in the liturgy, in the prayers and in the readings. Today we make sure we don’t work in silos, we work with the mining companies, with the other churches and we work from an interfaith context—challenging our governments to do the right thing.
Much has happened in recent years and things have changed. There’s a sense of trust that has developed and partnerships now are much easier. As leaders, we have learned to work together, we’ve learned to work together on the ground, but we’ve also learned to work with our international partners. I’m hugely grateful to PEPFAR. Initially there was a degree of suspicion but once we realized, through UNAIDS, that PEPFAR is there to help us check our own resources and to strengthen our resolve to help people – a great deal of trust has been developed.
“There is nothing more pro-life than PEPFAR.”
I pray that PEPFAR will be reauthorized to ensure that the commitments that we have made are realized. There is nothing more pro-life than PEPFAR. Millions of mothers and children have been saved from dying because of PEPFAR.
UNAIDS has also been essential. UNAIDS has showed us how important numbers and record keeping are, how important data is. We have to be systematic, we have to be thorough in our interventions, understanding that evidence-based interventions are critical.
“UNAIDS has showed us how important numbers and record keeping are, how important data is.”
In faith communities you can drown in the tsunami of problems, you throw yourself into your work without really knowing whether the intervention is working. But through praying, partnering with others, looking at the numbers and seeing the impact on people whose viral load has been reduced has been a great experience—we have learned a lot through working with UNAIDS and PEPFAR.
What does the faith community bring to the response to HIV?
It’s the fact that we are there. We are in every corner, even where governments can’t reach with their 4x4’s we have a little church there, we have a mosque there, we see God’s people every Sunday at the very minimum. We marry we bury we baptize, and we do this work not because we want to be paid or we want constituencies, it is our vocation and our calling.
“We marry we bury we baptize….We are in every corner, even where governments can’t reach with their 4x4’s”
Whether you are a Christian, Muslim, a Jew or a non-believer, you are a child of God and you need healing. We don’t exist for ourselves, we exist in order to show the love and care of God in the communities.
“We smile at you so please smile at us, because together we have made this possible.”
We must ensure that no more children are born with HIV, we must work together to ensure that every child living with HIV has immediate access to treatment and we must ensure that those children will be alive and thrive. That way in 2025 they will come here saying “you have allowed us to live, and we smile at you so please smile at us, because together we have made this possible.”
Region/country


Feature Story
Government leaders reaffirm their commitment to accelerate HIV prevention efforts to reduce new HIV infections
10 November 2023
10 November 2023 10 November 2023With just two years left to attain the 2025 HIV prevention target of fewer than 370 000 new HIV infections annually, the world is not on track. In 2022, 1.3 million people became infected with HIV – the urgency to accelerate progress cannot be overemphasized. The Global HIV Prevention Coalition co-convened by UNAIDS and UNFPA ensures a strengthened and sustained political commitment for primary prevention across key policy makers and programme implementers. It includes countries such as Botswana, Cameroon, Eswatini, Lesotho, Malawi, Rwanda South Africa, and Zimbabwe – which have reduced new HIV infections by more than 70% since 2010.
However, there were disparities across populations and regions. No significant declines were seen among key populations (sex workers, men who have sex with men and people who inject drugs).
Globally, 4,000 new HIV infections occurred among adolescent girls and young women aged 15-24 years, every week – 3,000 of these occurred in Sub-Saharan Africa. Approaches and investments for HIV prevention are currently insufficient to meet global targets.
The directors of National AIDS Coordinating Agencies, Ministry of Health HIV leads from the Global HIV Prevention Coalition focus countries and development partners were convened by the HIV Prevention Leadership Forum, with support from UNAIDS and UNFPA, to reinforce their commitment to stopping new HIV infections. This is part of efforts to ensure effective implementation of expanded HIV programmes with a focus on key and priority populations .
During the meeting, each country identified commitments that they will drive and will be held accountable for in 2024 as well as technical level actions necessary for programme optimization. Donors and global technical partners identified opportunities for technical and financial resources available at country level to supplement national resources to drive the action plans.
The first lady of Namibia and UNAIDS Special Advocate for Adolescent Girls, and Young Women, Her Excellency Monica Geingos urged the country leaders in the HIV response to adapt solutions tailored to their national needs culturally, socio-economically, and politically. Whilst strengthening global collaboration, leaders should strengthen partnerships across sectors within the countries. Success in HIV prevention is possible, however, not only does it require leadership at government level, but also communities must lead.
The Global Prevention Coalition co-chair and former Minister of Health of Botswana, Prof. Sheila Tlou encouraged government leaders to follow the science, make data-driven decisions and ensure community leadership and participation in HIV prevention programming. This will secure gains made, bridge disparities and expedite progress needed for success in HIV prevention.
Dr Ruth Laibon Masha, Co-Chair of the HIV Multi-Sector Leadership Forum and Director, National Syndemic Disease Control Council, underscored the need to secure gains made by extraordinary leaders from multiple sectors who have played a crucial role in advancing the HIV movement and achieving significant progress. “By continuing to lead from the front we can work together towards the goal of delivering a future free of new HIV infections and AIDS-related deaths. It’s time to recommit and finish the race against time “, she added.
Vice Minister, National Disease Control and Prevention Administration (NDCPA) affirmed China’s commitment towards strengthened multisectoral leadership and promotion of a nationally led HIV prevention and health agenda.
Quotes
“In this moment, community leadership counts, country leadership counts in making the commitments of this meeting and our Action Plans a reality”
“While scientists, policymakers and funders will continue to drive and be essential to this work, it’s community leadership and mobilization that will end this epidemic. But no matter how good the science or community leadership, HIV will not end if we don’t have significant policy change to reverse criminalization and lessen stigmatization of affected populations. If we can’t protect human rights, then we can’t end HIV. This is never just about the virus—it’s about people, and the people must lead.”
Our work



Feature Story
Indian partners reflect on a year after sex workers’ human rights affirmed
05 October 2023
05 October 2023 05 October 2023In 2022, the Indian Supreme Court ruled that sex workers were covered by Article 21 of the Constitution which assures every person the right to life. It recognized that sex workers are entitled to equal protection under the law.
The court instructed both central and state governments that sex workers should not be arrested, penalised, harassed or victimised during brothel raids. (Running a brothel is illegal in India. Individual sex work is not.) Nor should the possession of condoms and other safer sex commodities be treated as evidence of an offence. And the police should be sensitised to the community’s rights.
Moreover, the court also stressed the vital need to uphold the basic protection of human decency for the children of sex workers who, “bearing the brunt of social stigma… are removed to the fringes of the society, deprived of their right to live with dignity”. This ruling will help ensure that the children of sex workers can access essential services, including healthcare and education.
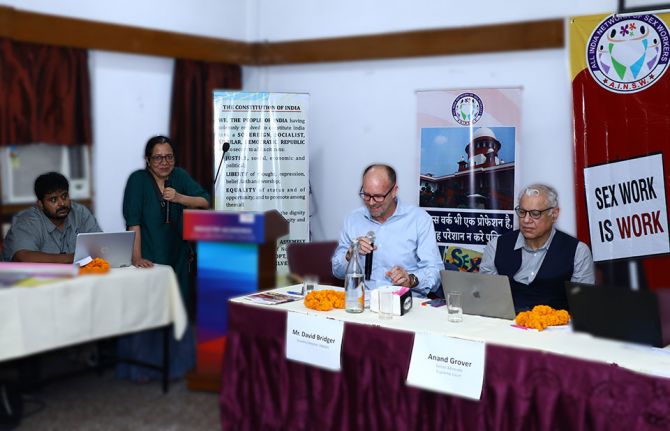
To commemorate this landmark judgment, the All-India Network of Sex Workers (AINSW) conducted a three-day National Consultation titled ‘Sisterhood and Solidarity with Sex Workers: One Year Since the Historic Supreme Court Ruling of 2022’. AINSW has been working on the issues of sex worker rights since 2011 across several states.
“Laws make a difference,” said David Bridger, UNAIDS Country Director to India in his keynote address. “The Supreme Court ruling was historic because with this, India joins a handful of countries like Canada and New Zealand that have explicitly instituted legal protection for sex workers. Recognizing the equal worth and dignity of every person is not only ethical, but also critical for ending AIDS.”
While giving an overview of the Supreme Court ruling, Senior Advocate, Anand Grover, noted that sex workers have taken steps which have contributed to the decline of HIV in India by negotiating condom use with their clients. A 2021 study found that 98% of sex workers used condoms. The work to educate and empower this community to have safer sex is paying off. HIV prevalence among female sex workers is now just under 2%. Protecting the safety and human rights of key populations expands their access to HIV services, accelerating progress in the response to HIV.
Mr Grover called for a full understanding of the law and how it impacts the lives of sex workers. He also stressed the importance of community participation in law and policy development, noting that the Court itself called for sex workers to be involved in decision-making processes linked to issues which affect them.
Shyamala Natraj, Executive Director of the South India AIDS Action Programme (SIAAP), briefed the audience about what went into making the 2022 ruling possible. She said the judgment was the result of strategic and consistent advocacy which centred on the lived experiences of sex workers.
In 2020, for example, the National Human Rights Commission issued an advisory recognising sex workers as entitled to the same social protection as other informal workers for the first time. Sex workers had been among the hardest hit during the COVID-19 pandemic. Not only did they experience an abrupt loss of income, but some were excluded from state social safety net responses. The fallout was extreme, including hunger, homelessness, debt, depression, and even suicide.
The SIAAP shared an example from Usha Ram (not her real name) from the town of Theni: “I did not have money to pay rent. The house owner forced me to vacate and humiliated me in front of my neighbours for doing sex work. I was on the streets with my children and did not even get the advance back.”
Ms Natraj encouraged the community to assert their human rights and secure access to the services that would ordinarily be provided to them under the law, including the issue of Aadhar (identification) cards, rations, poverty alleviation support and proof of residence documentation.
But despite the Supreme Court’s ruling that “sex work is a profession” with the same human rights as others, and that sex workers should not be harassed by the police, inequalities, stigma, and discrimination persist. Many sex workers are still reporting police harassment; some say they are still charged for soliciting clients.
To safeguard the human rights of sex workers, experts reiterated the need to implement the Supreme Court judgment at the grassroots level. UNAIDS and its cosponsors are committed to working with communities, policy makers and law enforcement to increase awareness and to ensure the universal upholding of sex workers’ human rights.
Our work
Region/country



Feature Story
Cities leading the way to achieving key targets in the HIV response
27 September 2023
27 September 2023 27 September 2023Gathered in Amsterdam for the annual Fast-Track Cities conference between 25 ─ 27 September 2023, cities shared their various initiatives toward achieving key HIV targets.
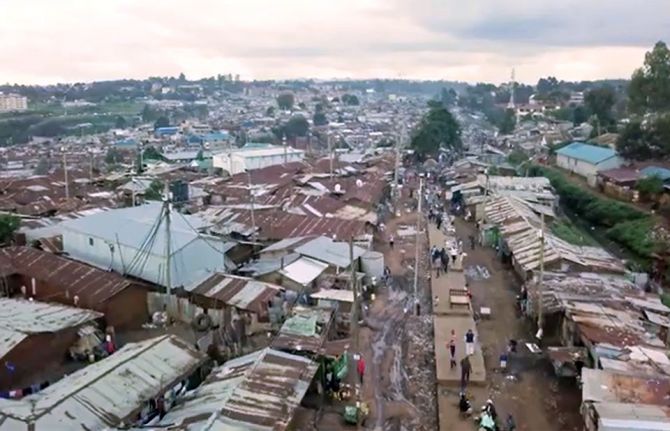
In Nairobi, Kenya a situation analysis conducted at a granular level helped the county to better understand the gaps in the HIV response and to identify priority actions. The data showed that there was a lack of health service points, especially for key populations and young people living in informal settlements. In addition, stigma and discrimination also keeps people away. Zipporah Achieng, a young person living with HIV navigating the dusty streets of Kibera, one of several informal settlements, can attest to this. “Before, life was not easy, the healthcare workers were not well trained, and when they saw youth coming to the hospital, they would start judging them, discriminating them.”
The Nairobi City County, with the support of the USAID-funded joint UNAIDS-IAPAC Fast-Track Cities project, developed activities to create awareness, address vulnerabilities, and reduce discrimination with a focus on young people. Informal settlements house up to 60% of Nairobi’s population despite covering less than 10% of the city. Over a period of five years, community members worked hand in hand with healthcare providers in the establishment of 30 friendly health centres for young people and men who have sex with men and sex workers. As a result, stigma against people living with HIV has been reduced while the uptake of HIV and other health services increased significantly during this time.
Ms Achieng is now a peer educator. She goes out in the community sharing her experience and getting people to come to the clinic. “Now I know what is right and what is wrong, I’m happy because life has changed, life is sweet, there is medicine, there is support, and I’m just happy,” said Ms Achieng.
Nairobi's commitment to fast-tracking HIV services for young people and key populations not only contributed to the city's own public health goals but also set an inspiring example for other urban centres in the country.
Discussions about sex and HIV in Indonesia remain taboo and information limited. As a result, HIV-related knowledge is low, especially among young people. In 2018, UNAIDS created an online chatbot named Tanya Marlo and integrated it in the popular messaging application LINE. “Before Marlo, finding reliable information about HIV and sexual health was really hard. It was difficult to get the right information”, says Arisdo Gonzalez, a user of the online application.
Support provided by the Fast-Track Cities project allowed this pilot to grow into a key tool to reach young people and increase HIV prevention and testing.
Last year alone, 200 000 engagements were recorded on social media and on average 100 users are directed to counselling every month. “Tanya Marlo has been an absolute hit among young people in Indonesia,” said Tina Boonto, UNAIDS Country Director in Indonesia. “Young people feel that they can chat with Marlo anytime, anywhere, and in secret, nobody has to know about it.” To ensure its sustainability and further development, a community group, YKS, has taken over the management of the application.
Kyiv joined the Fast-Track Cities initiative in 2016 and had made remarkable progress towards key HIV targets until Russia declared war in Ukraine. Many feared that treatment, HIV services and outreach would disintegrate. Thanks to emergency funds and the support of the Fast-Track Cities project, a number of interventions were put in place to help those in need, in particular members of key and vulnerable populations like people who inject drugs and LGBTIQ+ members. “Since the invasion, we have managed to maintain our test numbers, didn’t lose a single patient, and ensured continued access to antiretroviral therapy” said Dr. Vitali Kazeka, Director of the Kyiv AIDS center.
One of Kyiv's notable achievements is the establishment of shelters designed to cater to the unique needs of key populations affected by HIV. These shelters provide a safe and supportive environment while also ensuring access to essential healthcare services, counseling, harm reduction programmes, and education about HIV prevention. “The Fast-Track Cities project makes people living with HIV, and those from key population groups, feel like equal citizens of the city… They see that there are special initiatives that care about them and their future,” said Nataliia Salabai, UNAIDS Fast-Track Cities focal person in Kyiv.
Launched in December 2014, the Fast-Track Cities partnership has grown to more than 500 cities and municipalities that have committed to accelerate their local HIV, tuberculosis (TB), and viral hepatitis responses to achieve Sustainable Development Goal (SDG) 3.3 by 2030.
More than half of the world’s population currently live in cities and cities account for a large and growing proportion of people living with HIV, tuberculosis (TB) and other diseases. The risk of contracting, and vulnerability to, HIV and TB infection is often higher in urban areas compared to rural areas, because of urban dynamics such as social networking, migration, unemployment and social and economic inequalities.
In five years, 30 friendly health centres opened in informal settlements in Nairobi
Jakarta, Indonesia: Meet Chatbot Marlo
Despite war, Kyiv HIV outreach remains solid
Our work
Fast-Track Cities' initiatives to end AIDS
Related




Feature Story
Voluntary medical male circumcision shown to be highly cost-effective, highlighting the need to intensify scale up and sustainability
27 September 2023
27 September 2023 27 September 2023UNAIDS’ Global AIDS Update The Path that Ends AIDS underscores 2 main challenges faced by voluntary medical male circumcision (VMMC) programmes: diminished funding and low coverage among men in their twenties and older. Since VMMC was recommended by WHO and UNAIDS in 2007 as key to HIV prevention in high-prevalence settings, about 35 million men have accessed services across the 15 VMMC priority countries. While this shows good progress, the Global AIDS update highlights that VMMC coverage remains far from reaching the 90% global coverage target for impact in many subnational areas of priority countries. Additionally, funding has declined by almost half since 2020 from approximately US dollars 285 million to US dollars 147 million for the 15 countries funded by the United States President’s Emergency Plan for AIDS Relief (PEPFAR). But questions have arisen about VMMC’s cost-effectiveness under growing coverage of other biomedical interventions, such as antiretroviral treatment.
“We need strong political leadership to scale up implementation of VMMC programmes; tackle the inequalities holding back progress; and ensure sufficient and sustainable funding” said Angeli Achrekar, UNAIDS Deputy Executive Director of Programmes. “Countries that are putting people and communities first in their policies and programmes are already leading the world on the journey to ending AIDS by 2030.”
Voluntary medical male circumcision is a simple, safe procedure that has proven to reduce the risk of HIV transmission by up to 60% in heterosexual men. But is it cost effective? For how long must policy makers continue to promote VMMC among adolescent boys and adult men across VMMC priority countries? This is what a group of researchers investigated.
Now published in The Lancet Global Health and using 5 existing mathematical HIV models, the researchers aimed to assess whether providing VMMC for the next 5 years would continue to be a cost-effective use of HIV programme resources in sub-Saharan Africa. The models applied assumptions based on HIV epidemiology in VMMC priority countries focusing on Malawi, South Africa, and Zimbabwe. The impact and cost-effectiveness were projected over 50 years to capture clients’ lifetime HIV exposure and infection.
Findings reveal that a continuation of VMMC was cost-effective even in regions with low HIV incidence; VMMC was cost-effective in 62% of settings with HIV incidence of less than 1 per 100 person-years in men aged 15–49 years, increasing to 95% with HIV incidence greater than 10 per 100 person-years They underscored VMMC’s importance in continuing to avert HIV infections and related healthcare costs over time.
While details of the results varied by country and model (see Box1), overall VMMC was shown to be highly cost-effective and even cost saving in nearly all countries and scenarios.
| Box 1 Varying results across countries
|
The authors concluded that despite the scale-up of antiretroviral therapy and low HIV incidence in some settings, the continuation of VMMC for at least the next 5 years is cost-effective in almost all settings considered in this study.
“Clearly, intensified efforts and commitments are needed to scale up VMMC while at the same time sustaining these services to reach men and boys,'' said Dr Meg Doherty, Director of WHO’s Global HIV, Hepatitis and STI Programmes. “The new Global AIDS report shows a widening gap for men that is important to recognize and address efficiently and effectively for their own health and to reduce new infections.’’
These analyses support a call to action on intensified efforts to reach men and boys in general and for continued funding for VMMC programmes. The discussion on VMMC sustainability is crucial. UNAIDS and WHO are urging countries to intensify their efforts in scaling up VMMC to global coverage targets (90%), at the same time address programme sustainability.
In the 2025 HIV Prevention Roadmap, VMMC remains a core component of combination HIV prevention under the pillar of men and boys. It is not only cost-effective, but also, cost-saving in many settings. Accordingly, continued progress towards male circumcision coverage targets in all the VMMC priority countries must be accelerated

















