
Feature Story
UNAIDS – A year in review
23 December 2010
23 December 2010 23 December 2010
2010 has been a landmark year in the AIDS response. In November UNAIDS reported that the AIDS epidemic had been halted and that the world is beginning to reverse the spread of HIV. In its flagship report, the 2010 UNAIDS Report on the global AIDS epidemic, UNAIDS reported that the rate of new HIV infections had been reduced by nearly 20% in the past 10 years, that AIDS related deaths had been reduced by nearly 20% in the last five years and that the total number of people living with HIV had stabilised.
Investments made to date in the AIDS response were seen to be bearing fruit as the rate of new infections stabilised or decreased by more than 25% in at least 56 countries around the world, including 34 countries in sub-Saharan Africa, the area which continues to be most affected by the epidemic. In addition, more than 5 million people were estimated to be receiving antiretroviral treatment––a scale up of 30% in just one year.
However, 2010 was also a year in which for the first time resources for the AIDS response did not increase, with donor disbursements lower in 2009 than in 2008. This disappointing news came at a time when demand is continuing to outstrip supply in the AIDS response. For every one person who starts antiretroviral treatment a further two become infected with the virus.
At the XVIII International AIDS Conference which took place in Vienna in June, the 20,000 participants from 193 countries rallied behind UNAIDS’ call for a Prevention revolution and the Treatment 2.0 initiative which will help to ensure a cohesive and resource-maximizing AIDS response.
World leaders gathered at the United Nations for the MDG Summit in September and called for a new model of partnership to strengthen the AIDS response and achieve broader health and development outcomes.
Major developments were brought to light in 2010 in the field of scientific research. These included the CAPRISA study which found a microbicide gel to be 39% effective in reducing a woman’s risk of becoming infected with HIV during sex and the IPREX study which found that a pill taken once daily reduces the risk of HIV infection by an average of 43.8% for HIV-negative men, and transgender women, who have sex with men.
In 2010, UNAIDS’ board endorsed a new vision of “Zero new infections. Zero discrimination. Zero AIDS-related deaths.” The board also adopted the UNAIDS strategy 2011–2015. The intent of the strategy is to revolutionize HIV prevention, catalyse the next phase of treatment, care and support, and advance human rights and gender equality.
Related
 Keeping up the momentum in the global AIDS response
Keeping up the momentum in the global AIDS response
24 April 2019
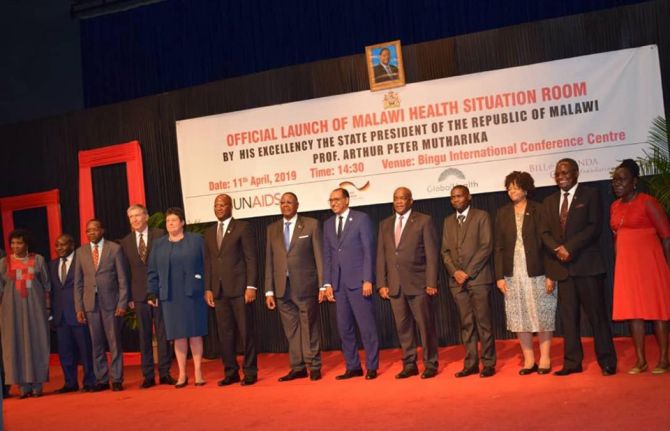 Malawi launches its health situation room
Malawi launches its health situation room
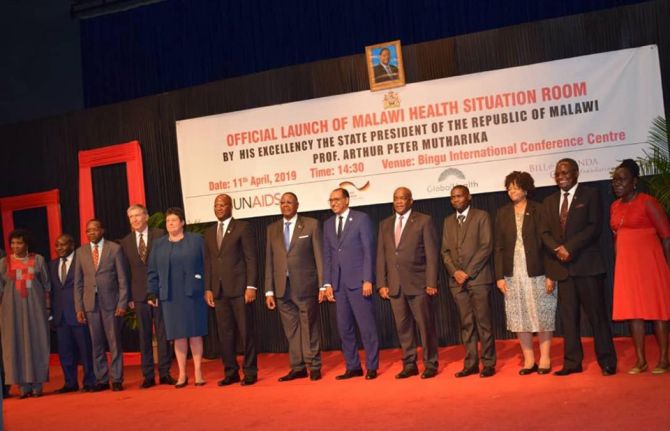
12 April 2019
 Learning lessons on evaluation
Learning lessons on evaluation

02 April 2019

Feature Story
Leaders call on countries to optimize resources for the AIDS response
17 December 2010
17 December 2010 17 December 2010
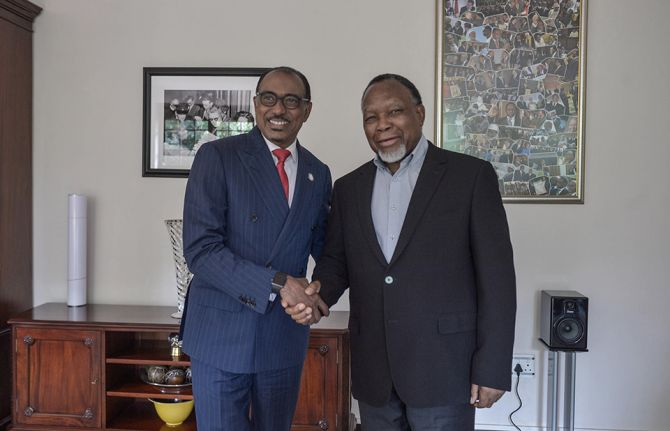
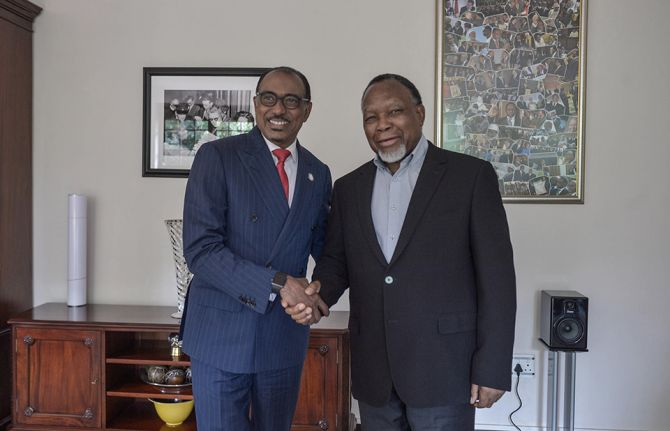
Mr Michel Sidibé, UNAIDS Executive Director (left) and Dr Luis Sambo, WHO Regional Director for Africa, at the meeting “Optimizing Resource Use and Alternative Health Funding Mechanisms: Prospects for AIDS Funding” held in Dakar, Senegal, on 16 December.
Ministers of Health and Finance from West and Central Africa joined representatives from civil society, the private sector and the United Nations for a discussion on financing and sustaining the AIDS response in a resource-constrained environment. Participants in the meeting, co-hosted by the Joint United Nations Programme on HIV/AIDS (UNAIDS) and the World Health Organization (WHO), reflected on the impact of the global financial crisis, risk management, alternative funding sources, and optimizing the use of available resources.
According to UNAIDS estimates, international donors and national governments together mobilized US$ 15.9 billion for the global AIDS response in 2009. However, the gap between investment need and resource availability is widening—in 2009 alone, there was an estimated shortfall of US $10 billion for the global AIDS response.
“Gains in the AIDS response are fragile. Resources for AIDS must be predictable and sustainable in the long term,” said Mr Michel Sidibé, UNAIDS Executive Director, addressing participants at the meeting. “Funding for AIDS is a shared responsibility,” he added, calling on both international donors and national governments to increase their investments in the AIDS response.
Nearly 90% of AIDS spending in low-income countries comes from international sources. A new Domestic Investment Priority Index developed by UNAIDS shows that 13 countries in West and Central Africa spend less than their capacity, commensurate to their disease burden and availability of government resources.
Investments in the AIDS response have yielded results: Between 2001 and 2009, for example, 10 countries in West and Central Africa reduced new HIV infections by more then 25%. In that same period, seven countries in the region stabilized the rate of new HIV infections.
To sustain these gains, meeting participants underscored the importance of consolidating HIV programmes and supporting long-term funding approaches that went beyond crisis management. Accountability around resource allocation would be critical, they noted.
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025

Feature Story
South Africa expanding access to ARV therapy
17 December 2010
17 December 2010 17 December 2010
South Africa has the world's largest population of people living with HIV; an estimated 5.6 million people in the country are living with HIV, representing nearly one sixth of the global disease burden. Credit: UNAIDS
South African Health Minister Dr Aaron Motsoaledi has announced that South Africa has successfully negotiated a range of price reductions for antiretroviral treatment in a bid to increase access to treatment for people living with HIV.
“It is my pleasure to announce the massive reduction in the prices of antiretroviral drugs which has resulted in the 53.1% reduction in the cost of the total tender,” said Dr Motsoaledi. “South Africa can now afford to treat twice as many people on ARVs compared to that which was previously budgeted.”
In a statement released on 14 December, the Health Minister announced that since World AIDS Day 2009, almost 5 million South Africans had been tested for HIV as part of the HIV Counselling and Testing campaign which was launched by President Zuma in April.
The campaign aims to test 15 million people for HIV by the year 2011, up from 2.5 million in 2009 – a six-fold increase in just two years. Of the 5 million people tested since the launch, over 900 000 were found to be HIV positive.
More people are finding out their status as testing is scaled up which is resulting in more people coming forward to access treatment. These price reductions are essential to ensuring that all people in need have timely access to the lifesaving medication.
Michel Sidibé, UNAIDS Executive Director
UNAIDS Executive Director, Michel Sidibé attended the launch in April and called for reductions in the price of antiretroviral drugs which were at least 25-30% higher than average international prices and posed a key challenge in South Africa’s efforts to expand treatment.
“This is a significant breakthrough for South Africa’s response to the epidemic,” said Mr Sidibé. “More people are finding out their status as testing is scaled up which is resulting in more people coming forward to access treatment. These price reductions are essential to ensuring that all people in need have timely access to the lifesaving medication.”
South Africa funds more than two thirds of its AIDS response. In 2010, South African leaders committed $1 billion US dollars to the AIDS response – a 30% increase over the previous year.
South Africa has the world's largest population of people living with HIV; an estimated 5.6 million people in the country are living with HIV, representing nearly one sixth of the global disease burden. Approximately 18% of adults in South Africa are infected with HIV.
Related

Feature Story
Report of the UNAIDS Executive Director at the 27th Meeting of the Programme Coordinating Board
06 December 2010
06 December 2010 06 December 2010
Mr Michel Sidibé UNAIDS Executive Director delivers his report to the Programme Coordinating Board. 5 December, 2010. Credit: UNAIDS/F. Chironi
UNAIDS Executive Director, Michel Sidibé, delivered his report to the 27th Meeting of the UNAIDS Programme Coordinating Board (PCB). In his report, Mr Sidibé updated the Board on the Joint Programme’s activities since its last meeting in June 2010. He also spoke on recent developments in the AIDS response, the ongoing impact of the global recession, and efforts to make UNAIDS a more effective and efficient organization.
Related
 Upholding dignity for everyone: Ariadne Ribeiro Ferreira
Upholding dignity for everyone: Ariadne Ribeiro Ferreira
21 November 2024

Feature Story
The Prevention Revolution: HIV Prevention on the social media agenda on World AIDS Day
03 December 2010
03 December 2010 03 December 2010
Map by www.trendsmap.com
UNAIDS teamed up with MTV Staying Alive Campaign to put HIV prevention on the global agenda through social media. Over a six week period in the lead up to World AIDS day the ‘#PreventionRevolution’ campaign inspired thousands of online conversations on the need to revitalize interest in HIV prevention.
Under the banner “More than 7000 new HIV infections every day is unacceptable. We need a Prevention Revolution”, the key word or hashtag #PreventionRevolution became one of the most popular on the social media site Twitter during World AIDS Day.
Based on a network approach, where the idea is to mobilize influencers—people who have many connections in a given social network—the prevention revolution community started reaching out to celebrities as well as friends to share the message. UNAIDS in collaboration with partners mobilized people both online and off line, and with support from the United Nations in New York and Cosponsors UNHCR, UNICEF, UNDP, World Bank, UNESCO and UNFPA, thousands of people worldwide joined the conversations.
A series of videos that were produced for the campaign, embedded below, reached over 120,000 views on YouTube.
On World AIDS Day, using the hashtag #PreventionRevolution, people shared personal stories, encouraged each other to use condoms, get tested and educated themselves about HIV. As one person on Twitter put it: “When was your last test? Go get tested! Join the prevention revolution” while another tweeted: “For me it’s every day World AIDS Day—A prevention revolution? It starts at home. Take a stake in the fight!”
Organizations including the Bill and Melinda Gates Foundation, ONE, Oxfam, UN, UNHCR and celebrities Annie Lennox, Craig David, Bianca Gonzalez and the band 30 Seconds to Mars together sent out the message that an HIV prevention revolution is needed to almost 3 million people on World AIDS Day.
Key partner MTV Staying Alive also conducted live interviews via Twitter under the Prevention Revolution and MTV Get Tested banners with musicians Peter Wentz, Travis McCoy and the group Good Charlotte who together have over 3.5 million followers on Twitter.
The campaigns also owes its success to individuals who have 20, 50, 100, or 200 followers of Twitter and Facebook who asked their friends to take part in the call for a prevention revolution. The social media blog Mashable featured the campaign in their social good section and subsequently asked their 2 million followers on Twitter to “Start a #PreventionRevolution this World AIDS Day.”
As the world woke up on 2 December, the conversation was still going, but the message had changed: “World AIDS Day is over – the epidemic is not! We still need a Prevention Revolution.” UNAIDS will now explore ways that this movement can be built upon and leveraged in the coming months.

Feature Story
UNAIDS Programme Coordinating Board meeting to open
03 December 2010
03 December 2010 03 December 2010
Photo from the PCB held in Geneva, December 2010. Credit: UNAIDS
The 27th meeting of UNAIDS Programme Coordinating Board (PCB) will open in Geneva on 6 December 2010.
Ahead of the meeting, The Netherlands, current PCB chair, hosted a field visit for a delegation from the board composed of Member State participants from Mauritania, Iran, Thailand, Poland, and El Salvador, a non-governmental organization from the Europe region, and Cosponsors UNDP and UNICEF.
During the three-day visit which concludes today, the delegation met officials from the Ministries of Health and Foreign Affairs to hear how the country’s far-reaching policies are developed and implemented. They discussed experiences directly with non-governmental organizations, and visited programmes on the ground including community services that support sex workers and a facility providing harm reduction services for people who inject drugs. A meeting with the Multi-Party Initiative on HIV/AIDS enabled participants to see a broad-political approach in action.
This visit follows a PCB trip to Viet Nam in 2009 and El Salvador in earlier this year. Country visits by a PCB delegation help to orient and inform discussions in the board meeting itself.
A key item on the PCB meeting agenda will be the receipt for endorsement of the draft UNAIDS Strategy for the period 2011-2015. The board will also receive a progress report on implementation of the Second Independent Evaluation of UNAIDS as well as a report of the Task Force on the completion of its work related to the principles and processes for draft decisions and decision making in the PCB.
Next week’s board meeting will be addressed by Dr Françoise Barré-Sinoussi, Co-Chair of the UNAIDS High Level Commission on HIV Prevention and Nobel Prize laureate for Medicine in 2008 for her role in the discovery of the human immunodeficiency virus (HIV). The Executive Director will also present his report.
“Food and nutrition security and HIV: how to ensure food and nutrition security are integral parts of HIV programming,” is the title of the thematic session which will take place on 8 December.
For more information on the board including all background documents visit the PCB web page.
Related

Feature Story
UNAIDS and the African Council of AIDS Service Organizations sign a Memorandum of Understanding
03 December 2010
03 December 2010 03 December 2010
From left Meskerem Grunitzky, Director of the UNAIDS Regional Support Team for West and Central Africa, Dr. Ndoye, Executive Secretary of the National AIDS Council of Senegal and Cheikh Tidiane Tall, Executive Director of AfriCASO. Credit: UNAIDS.
During the civil society consultation on universal access and the Millennium Development Goals with the theme "Sustain the results – strengthen links and interactions," the Joint United Nations Program on HIV/AIDS (UNAIDS) and the African Council of AIDS Service Organizations (AfriCASO) signed a memorandum of understanding on 3 December in Dakar.
The agreement formalizes the longstanding partnership aimed at ensuring effective and quality involvement of African civil society organizations in the promotion of universal access and achieving the Millennium Development Goals in Africa. The memorandum of understanding also extends the collaboration between the parties at the institutional level.

Feature Story
World AIDS Day commemorated across the world
02 December 2010
02 December 2010 02 December 2010
Brazilian President Luiz Inácio Lula da Silva was presented with the UNAIDS leadership award by Mr Michel Sidibé, UNAIDS Executive Director on World AIDS Day, 1 December 2010. Brasilia, Brazil. Credit: UNAIDS/Martino
World AIDS Day was held on 1 December. Here are some photos from across the globe capturing the sprit of Universal Access and Human Rights – the theme of this year’s World AIDS Day.
Related

Feature Story
World AIDS Day at the International Labour Organization highlights world of work and HIV
02 December 2010
02 December 2010 02 December 2010
ILO human red ribbon which was illuminated as part of the Light for Rights global campaign. Credit: ILO
Preventing HIV and protecting human rights in the work place were the themes of the International Labour Organization’s (ILO) event on World AIDS Day. Staff members formed the traditional ILO human red ribbon which was illuminated as part of the Light for Rights global campaign.
Mr Guy Ryder, ILO Executive Director, Standards and Fundamental Principles and Rights at Work Sector, addressed the gathering of ILO staff as well as colleagues from other UN agencies, and civil society organizations. He asserted the determination of the ILO to keep the promise to stop the spread of HIV: “The new ILO Recommendation adopted in June 2010 is a significant step. HIV is central to the ILO’s Decent Work Programme.”
The new ILO Recommendation adopted in June 2010 is a significant step. HIV is central to the ILO’s Decent Work Programme
Guy Ryder, ILO Executive Director, Standards and Fundamental Principles and Rights at Work Sector
Formulated with the aim of enhancing the contribution of the world of work to attaining universal access to HIV prevention, treatment, care and support services, the recently adopted labour standard also contains provisions for anti-discrimination measures at all levels and stresses the importance of confidentiality and employment and income generation for people living with HIV. It is also intended to protect workers against unfair dismissal due to actual or perceived HIV status and mandatory HIV testing.
Dr Sophia K. Kisting, Director of ILO Programme on HIV and the World of Work read the award winning poem ‘Shining with HIV’ written by Bolivian José Willan Montaño Ferrel, which conveyed a strong message on the dignity of having a job and decent working conditions. It was one of the three winning entries in the contest ‘Positive workers write!’, held jointly in Latin America by the ILO and the International Trade Union Confederation (ITUC) .
The event also premiered two videos, “Loggers Learn about HIV/AIDS Prevention in Guyana” and “Business Women on Board with HIV/AIDS Message in Malawi.” Both videos include strong messages on the need to eliminate stigma and discrimination at work.

Feature Story
Affordable TB prevention a must for people living with HIV
01 December 2010
01 December 2010 01 December 2010
Tuberculosis (TB) is a leading cause of death among people with HIV and, in order to mitigate this threat, low-cost preventive therapy is essential. In new guidelines released today, the World Health Organization (WHO) sets out how such therapy can be accessed safely and effectively.
According to WHO, the anti-TB drug isoniazid has a dramatic positive impact and the guidelines, aimed at resource-constrained settings, promote the use of Isoniazid Preventive Therapy (IPT) as a simple and cost-effective method that stops TB bacteria becoming active. A quarter of the nearly two million AIDS-related deaths each year is associated with TB and in some communities up to 80% of people who test positive for tuberculosis are also living with HIV.
WHO is committed to increasing the use of IPT. Coverage is currently extremely low with only 0.2% of all people with HIV having had access to this therapy last year. Additionally, around the globe just one in 20 HIV-positive people has ever been screened for TB.
World AIDS Day reminds us that business as usual is unacceptable and HIV programmes need to significantly expand their efforts to address TB
Dr Gottfried Hirnschall, Director of WHO’s HIV Department
“World AIDS Day reminds us that business as usual is unacceptable and HIV programmes need to significantly expand their efforts to address TB,” said Dr Gottfried Hirnschall, Director of WHO’s HIV Department. “We need to fully implement the WHO Three I’s for HIV/TB strategy in collaboration with all partners”.
The Three I’s are: Isoniazid Preventive Therapy, Intensified TB screening and Infection control for TB. According to WHO, these measures should be delivered as part of comprehensive HIV services.
“In many countries HIV is a major driver of the TB epidemic. TB is preventable and curable and the new guidelines show how to break the chain that links TB and HIV leading to death,” said Dr Mario Raviglione, Director of WHO’s Stop TB Department. “All countries and communities need to implement the new guidelines and WHO can provide the necessary support to ensure that this can happen.”
To encourage access to IPT for the millions in need, the WHO guidelines, which are based on recent scientific evidence used to update 1998 policy, address some of the misconceptions seen to be partly responsible for the IPT’s low coverage. There is no scientific evidence, for example, to support concerns that the treatment causes drug resistance to isoniazid. Also, IPT can be started following simple clinical screening without the need for costly mandatory tests as had been feared.
There are several key recommendations in the new WHO guidelines:
-
All children and adults living with HIV, including those on antiretroviral treatment and pregnant women, should receive IPT.
-
IPT should be provided for 6 to 36 months, or as a life-long treatment in settings with high HIV and TB prevalence.
-
People living with HIV who may have TB symptoms should befurther screened for active TB or other conditions to enable them to access appropriate treatment.
Preventing people living with HIV from dying of tuberculosis is one of UNAIDS’ priority areas.



















