Feature Story
United Nations Secretary-General’s report on HIV
28 May 2025
28 May 2025 28 May 2025The United Nations Secretary-General António Guterres will present his report on HIV to the 79th United Nations General Assembly at the UN in New York on 5 June 2025.
The report, The urgency of now: AIDS at a crossroads – progress report on the 2025 targets and strategic directions for the future, contains a review of progress towards realizing the targets and commitments set out in the 2021 Political Declaration on HIV/AIDS and an outline of the work that still lies ahead.
It comes at a critical moment in the global HIV response, when urgent action is needed to protect the hard-won gains and accelerate progress towards ending AIDS as a public health threat.
UNAIDS has been supporting countries to gradually reduce their reliance on external assistance.
The current Global AIDS Strategy 2021–2026 has led the HIV response with a bold vision of ending inequalities that continue to fuel the epidemic. The midterm review of the Strategy, published as part of the annual Global AIDS Update in July 2024, highlighted key achievements and remaining challenges to inform the development of the next phase of the response.
Under the current strategy, fewer people acquired HIV in 2023 than at any point since the late 1980s. Over 30 million people were receiving life-saving antiretroviral therapy, reducing AIDS-related deaths to their lowest level since the peak of 2004. Significant gains have been made in sub-Saharan Africa, underscoring the power of existing interventions to end AIDS as a public health threat by 2030. As the United Nations approaches its eightieth anniversary, the results of the HIV response stand as a powerful testament to the impact of multilateral action and must be protected.
Amid recent challenges and the fragility of the HIV response, the world is falling behind in achieving the 2025 HIV targets. Obstacles to accessing treatment, insufficient prevention programming, a failure to adequately support the work of communities, rising inequalities and a lack of political will and financial support threaten the response.
The next Global AIDS Strategy, for the period 2026–2031, led by UNAIDS, is being developed at a time when the response to the HIV epidemic is at a crossroads. The strategy will be among the most important in 40 years of response to the pandemic. Developed in a context of instability for many countries, in particular with regard to HIV-related funding, the strategy will be crucial for accelerating the achievement of the 2030 Agenda for Sustainable Development and setting the foundation for a sustainable response to HIV post-2030.
This report is also available in Arabic, Chinese, French, Russian and Spanish.
2025 Report of the Secretary-General

Feature Story
An urgent call to support youth-led organizations
28 May 2025
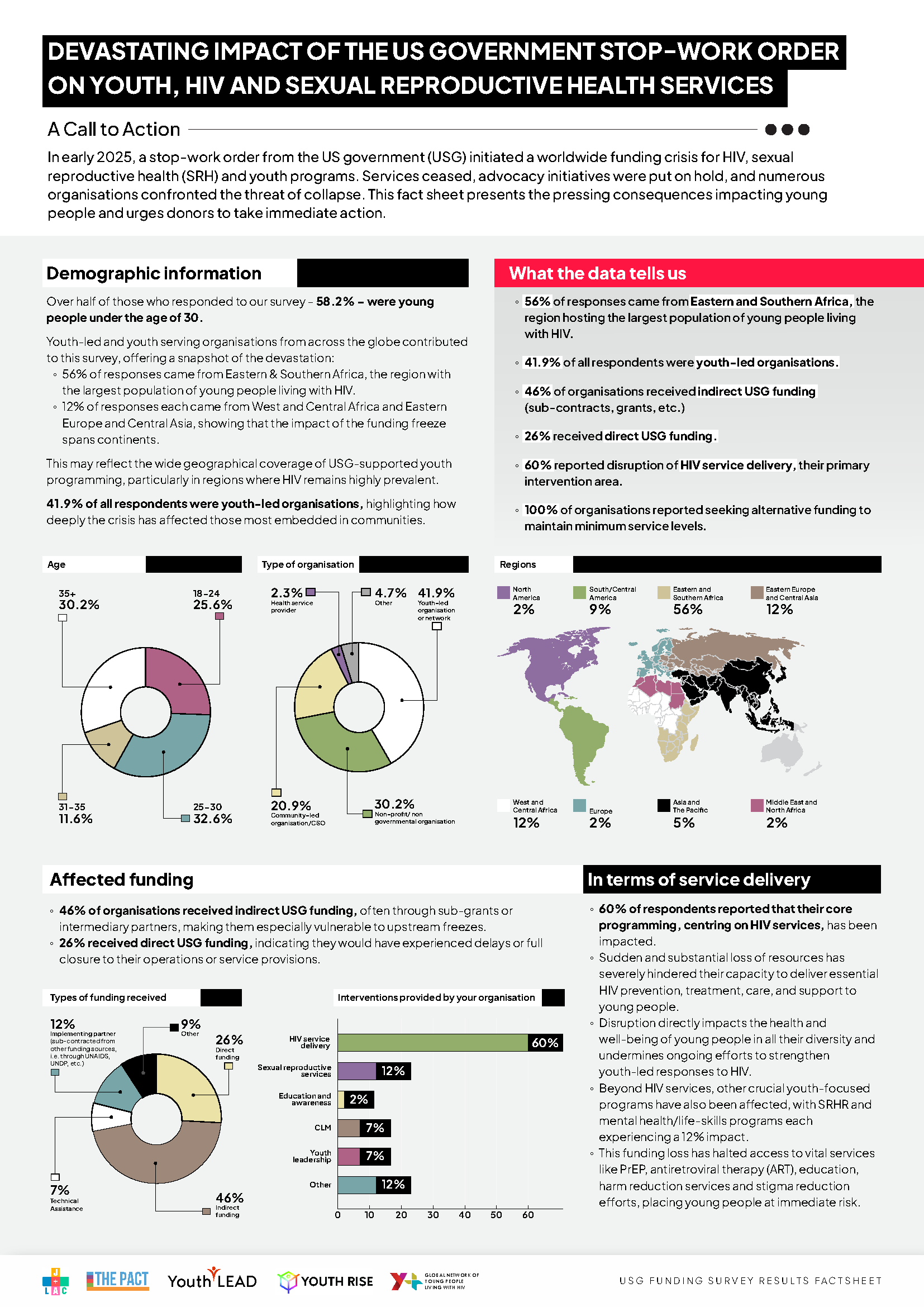
28 May 2025 28 May 2025The sudden stop-work order from the US government in early 2025 triggered a global funding crisis for HIV, sexual reproductive health (SRH), and youth programmes. This abrupt halt has left countless youth-led and youth-serving organizations struggling to survive, with devastating consequences for young people worldwide. The impact is profound, and the need for immediate action is critical.
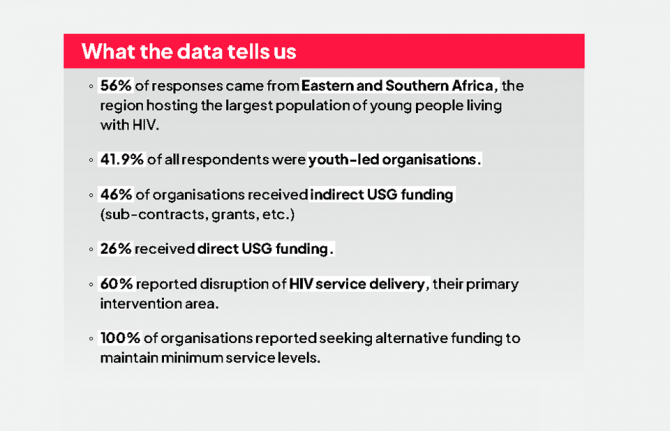
A survey conducted by Y+ Global, Youth LEAD, Youth RISE, The PACT, and J+LAC in March 2025 among organizations delivering HIV and SRH youth programmes reveals the stark reality faced by youth-led and youth-serving organizations. Forty-five youth-led and youth-serving organizations from around the globe completed the survey, with 56% of responses coming from Eastern and Southern Africa, the region hosting the largest population of young people living with HIV. Sixty percent of respondents reported disruptions to their core HIV services, severely hindering their ability to provide essential HIV prevention, treatment, care, and support. These disruptions directly impact the health and well-being of young people in all their diversity and undermine ongoing efforts to strengthen youth-led HIV responses.
Beyond HIV services, other crucial youth-focused programmes have also been affected, with SRH, mental health, and life-skills education programmes each experiencing a 12% decrease. Furthermore, activities like youth-led advocacy and engagement in policy and decision-making discussions have also been impacted, leaving youth voices under represented and unheard in the HIV response as well as other development areas.
The survey also warns about the abrupt policy changes occurring as a consequence, including the integration of HIV-specific clinics into general health systems, and the surge of restrictive laws targeting organizations working on gender, diversity, and sexual and reproductive health and rights, using the term “foreign agent” to criminalize their work. These changes are causing the collapse of service delivery models and increased barriers to youth-led organizations, further reducing accessibility for young people.
“The funding cuts are not just numbers on a spreadsheet; they represent real lives, real services, and real hopes lost. Youth-led organizations are the lifeline for so many young people, especially those most at risk,” shared Maximina Jokonya, Executive Director of Y+ Global. “We need urgent action from donors and governments to recommit and reinvest in youth leadership and safeguard the future of the HIV response,” she added.
Despite these setbacks, youth-led organizations are showing incredible resilience by launching crowdfunding campaigns, seeking alternative national and international partnerships, and continuing peer outreach with limited resources. Still, the long-term sustainability of these efforts is threatened by the funding crisis.
Youth and the next Global AIDS Strategy
Amidst this crisis, UNAIDS convened two global youth consultations in the context of the Global AIDS Strategy 2026 - 2031 development process to gather young people’s views and priorities for the future of the HIV response. More than 120 young people from diverse young key and vulnerable population groups participated in this consultative process. The key messages resulting from these consultations are unequivocal: young people demand involvement in decision-making spaces of the HIV response and in the development of alternative funding strategies, such as the sustainability roadmaps. They also demand a leading role in the implementation and monitoring of these decisions, as well as the positioning of human rights, gender equality, mental health, and innovation at the centre of the HIV response.
Call to action
Youth-led organizations are making an urgent call to all donors, partners, and policymakers to act now to save youth-led responses by reinstituting traditional funding support, increasing domestic and emergency funding solutions to maintain the operational stability of youth-led organizations, and supporting youth leadership in the HIV response.
Survey results
Our work
Related

Feature Story
“We must do everything we can to keep the lights on for the HIV response” says UNAIDS Country Director for Ethiopia Tina Boonto
26 May 2025
26 May 2025 26 May 2025Ethiopia, with a population of 130 million, is Africa’s second most populous country. Despite steady economic growth approaching low-middle income status, the country faces a daunting number of challenges, from economic pressures and development needs to recurring natural disasters such as droughts and floods, as well as conflict and other man-made crises. These factors mean Ethiopia still relies heavily on external aid-particularly for food security and humanitarian assistance.
On top of these existing burdens, HIV remains a significant public health challenge. The country is home to an estimated 610 000 people living with HIV, with over half a million currently on life-saving antiretroviral treatment-most of which is funded by international donors. Recent cuts in US funding have put Ethiopia’s HIV response at risk, threatening to reverse years of progress and placing additional strain on an already fragile health system.
We sat down with Tina Boonto, UNAIDS Country Director for Ethiopia, to discuss the impact of the funding crisis, the government’s response, the resilience of communities, and what needs to happen next to protect Ethiopia’s HIV response.
Q: What is the current situation, and how has the recent US funding crisis impacted the HIV response?
Ethiopia has made significant progress in its HIV response in recent years and is on track to reach the UNAIDS 95-95-95 targets with 90% of people living with HIV in the country being aware of their HIV status; 94% of those diagnosed with HIV receiving antiretroviral (ARV) therapy; and 96% of people on ARV therapy achieving viral suppression. The US Government through PEPFAR and the Global Fund have been the primary funders for the HIV response, supporting treatment for over 530 000 of the estimated 600 000 people living with HIV in the country. However, the sudden cuts had a devastating impact. Critical services have stopped, people have lost their jobs, and many clinics have closed their doors. People living with HIV now face uncertainty about their access to medication, testing, and prevention services.
In Bahir Dar, for example, programmes for key population have stopped, outreach workers have lost their jobs, and peer support groups have been terminated. It’s heartbreaking to see the situation on the ground. Clients arrived at clinics to find them closed, and many were left without guidance or support.
Women are anxious about the availability of medication and prevention tools like condoms. Without these, the risk of HIV transmission increases, and the health of those already living with HIV deteriorates. Some cannot even afford basic necessities like food, let alone treatment.
Q: How are communities responding to the collapse of HIV services?
Despite the collapse, communities are showing incredible resilience and a fighting spirit. Peer educators, youth groups and mothers are stepping in where formal systems are failing. For example, in the Afar region, a case manager working with people living with HIV continued his outreach work despite funding cuts. He was able to get funding from the health bureau and shared “even if the money is not enough, I’m happy to continue to help reach people living with HIV, providing pregnant women information on how to prevent transmission to their babies”.
But while these community-led efforts are inspiring, they cannot replace the need for sustainable funding. Community members often live below adequate income levels, and they need support for basics like transport and food. UNAIDS is encouraging the government to consider a social contract with community organizations-similar to Ethiopia’s successful Health Extension Worker model-so that peer outreach workers can be formally supported and paid for their essential outreach work.
The reason why we are pushing for outreach workers to be supported is because stigma and discrimination remain significant barriers. Even after 40 years of the HIV epidemic, people living with HIV in Ethiopia still experience stigma, which deters them from seeking care at public facilities. Many fear being discriminated against or not receiving adequate services. This is why the role of community peer outreach is so vital. Without armies of community outreach workers, especially in high-burden areas, it’s impossible to have a successful HIV programme.
Q: What lessons can be drawn from this crisis for the future of HIV response in Ethiopia and beyond?
The crisis has exposed the fragility of systems built around a single funding stream. When the money stopped, so did services, trust, and hope. We must build resilience into the system from the start. Community-led organizations must be recognized as essential, and youth-led innovation must be scaled up. Emergency preparedness and integrated, people-centered solutions are crucial, especially as HIV intersects with conflict, displacement, and gender-based violence. HIV must remain central to humanitarian, development and recovery agendas-not as an afterthought, but as a foundation.
UNAIDS is also supporting by working on producing an investment case to prioritize key components of the HIV programme for government funding. There are ongoing discussions about new partnerships with the private sector and exploring alternative financing mechanisms. There is political will. The Ministry of Health is considering adopting the methodology of the HIV Sustainability Roadmap to develop a broader health sector sustainability strategy. UNAIDS is supporting these efforts by helping to produce a sustainability strategy and mobilizing resources alongside other donors
Q: What steps is the Ethiopian government taking to address the funding crisis?
The government recognizes this as a wake-up call and is actively considering solutions to find resources to cover priority health issues, including HIV, tuberculosis, and malaria. However, the scale of the challenge is enormous-external assistance for Ethiopia’s health, humanitarian and development needs amounts to around US$ 2.7 billion annually. The government is exploring options such as introducing a social tax, where all workers would contribute to health funding, but this is still under parliamentary discussion. While these efforts are encouraging, they are not yet sufficient to fill the gap left by international donors.
Q: How is UNAIDS supporting the government and the HIV response during this crisis?
UNAIDS is playing a critical role. In response to the funding crisis, we conducted immediate impact surveys to understand which programmes have stopped or are ongoing, and what the consequences are on the ground. This information feeds into the national plans and sustainability plan.
We are also producing an investment case to help the government prioritize key components of the HIV programme for domestic funding. Our costing data enables us to propose affordable models, like social contracting with community organizations.
We are reviving HIV prevention efforts, including using AI-powered digital platforms and chatbots to reach young people with real-time information. Ethiopia was also piloting long-acting injectable antiretroviral medicine to prevent HIV or ‘PrEP’ before the funding cuts stopped this progress.
Finally, we are working closely with the Ministry of Health, the Global Fund, and community organizations to mobilize resources and advocate for integrated, sustainable solutions.
Q: What is your message to the international community at this critical juncture?
We need global solidarity now more than ever. We are so close to ending AIDS as a public health threat by 2030. Over half a million people in Ethiopia are on antiretroviral treatment—we cannot let them down. The world has come too far, and too many have sacrificed too much to let progress slip away now. We must do everything possible to keep the lights on for the HIV response, both in Ethiopia and globally.
The resilience of Ethiopian communities is inspiring. People are refusing to give up, finding new ways to support each other and keep the response alive. With renewed commitment from the government, partners, and the international community, we can protect the progress made and continue moving towards ending AIDS as a public health threat.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads the global effort to end AIDS as a public health threat by 2030 as part of the Sustainable Development Goals.
Following the US funding cuts in January, UNAIDS is working closely with governments and partners in affected countries to ensure that all people living with or affected by HIV continue to access life-saving services. For the latest updates, please visit unaids.org
Related resources
Watch: Tina Boonto, Ethiopia Country Director: Communities are going out of their way but they need help
Watch: UNAIDS asking government to increase domestic funding for the HIV response in Ethiopia
Watch: "We cannot let people down," says Tina Boonto, Country Director in Ethiopia
Region/country





Feature Story
Towards stigma-free healthcare for people living with HIV in Moldova
23 May 2025
23 May 2025 23 May 2025In the heart of Chișinău, Moldova, medical students, healthcare workers, civil society members, and representatives of the international community took a symbolic step toward a more inclusive, respectful, and stigma-free health system.
To commemorate International AIDS Candlelight Memorial Day and under the theme of “In Their Shoes”, the event was organized by UNAIDS in partnership with the Association of Medical Students and Residents, the Nicolae Testemițanu State University of Medicine and Pharmacy and the Ministry of Health of the Republic of Moldova. The event marked a growing movement to end HIV-related stigma in Moldova’s healthcare system—a transformation already underway in medical education.
Since 2023, the Nicolae Testemițanu State University of Medicine and Pharmacy, with technical support from UNAIDS and financial backing from the Embassy of Sweden, has introduced Human Rights in Healthcare as a compulsory course across all faculties. Rather than remaining a stand-alone subject, human rights principles are now embedded in core clinical disciplines such as surgery, gynecology, oncology, infectious diseases, and family medicine, including training on how to treat people living with HIV and members of key populations.
“Patients today are more informed. They understand their rights,” said Dr Virginia Salaru,
vice-director of the Didactic and Academic Quality Management Department and Associate Professor. “And medical professionals must be ready, not just scientifically, but ethically.”
This reform is timely. Despite progress in HIV prevention and treatment, stigma in healthcare remains a major barrier. According to the Stigma Index 2.0, people living with HIV, especially those from key populations such as people who use drugs, sex workers, men who have sex with men, and transgender people, continue to face breaches of confidentiality, avoidance by medical staff, and discriminatory treatment.
“Despite all our achievements today, despite having antiretroviral therapy, knowledge, and experience, I still hear stories of despair, rejection, and stigma every day. Sadly, people are still dying, not from the virus, but from attitudes and indifference,” said activist Irina Goreaceaia.
“As the authority responsible for public health, we want every person living with HIV to have equal access to diagnosis, treatment, and support,” said Angela Paraschiv, Secretary of State, Ministry of Health. “HIV does not have to be a social condemnation. The health system offers the support people need to live normal lives — with dignity, not isolation.”
In partnership with UNAIDS, the university conducted a curriculum review through a human rights lens. It identified critical gaps including the fact that, while ethics were taught in theory, students were not being prepared to navigate real-world complexities such as stigma, patient diversity, and discrimination. The updated curriculum now trains students in assertive communication, confidentiality, and patient autonomy regardless of HIV status, gender identity, or background.
“Healthcare should be a place of healing, not harm,” said Svetlana Plamadeala, UNAIDS Country Director for Moldova. “Stigma has no place in clinics, hospitals, or maternity wards. Every person living with HIV deserves privacy, respect, and access to care.”
This effort is part of the broader United Nations programme which includes training more than 250 healthcare workers in rights-based approaches and stigma reduction. Called “Strengthening Human Rights on Both Banks of the Nistru River,” the programme consists of a series of student-led initiatives, public awareness campaigns, and community engagement to reinforce these lessons across Moldova’s campuses and clinics.
Early results are promising. Anonymous student evaluations show high satisfaction with the human rights curriculum, and practical implementation has already started across disciplines.
“In addition to the Human Rights course, the campaigns, flash mobs, and student-led initiatives really opened our eyes,” said Cătălina Repesciuc, a second-year student at the university. “Understanding stigma, especially around HIV, is essential not just in theory, but for how we interact with real patients in everyday practice.”
Katarina Fried, Ambassador of Sweden to Moldova, emphasized that “this initiative combines solidarity, education, and human rights. Our project with the UN reinforces these values on both sides of the Nistru River. The active involvement of students and health authorities shows what social responsibility looks like in action.”
Moldova’s message is clear: healthcare must be grounded in respect, dignity, and rights. And thanks to support from UNAIDS and Sweden, that transformation is already underway — in the classroom, in clinics, and in the minds of the next generation of healthcare professionals.
“You wear a white coat for only a few hours a day, the rest of the time, you are a patient like anyone else,” said Dr Cocieru-Salaru. “Treat your patients the same way you want to be treated. Always ‘walk in their shoes’,” she added.
Region/country

Feature Story
Global leaders convene to accelerate access to long-acting HIV prevention technologies amidst funding cuts
23 May 2025
23 May 2025 23 May 2025The global response to HIV has reached a crucial juncture. Groundbreaking scientific advances, including the development of long-acting HIV prevention technologies like lenacapavir and cabotegravir, offer a transformative opportunity to curb the epidemic.
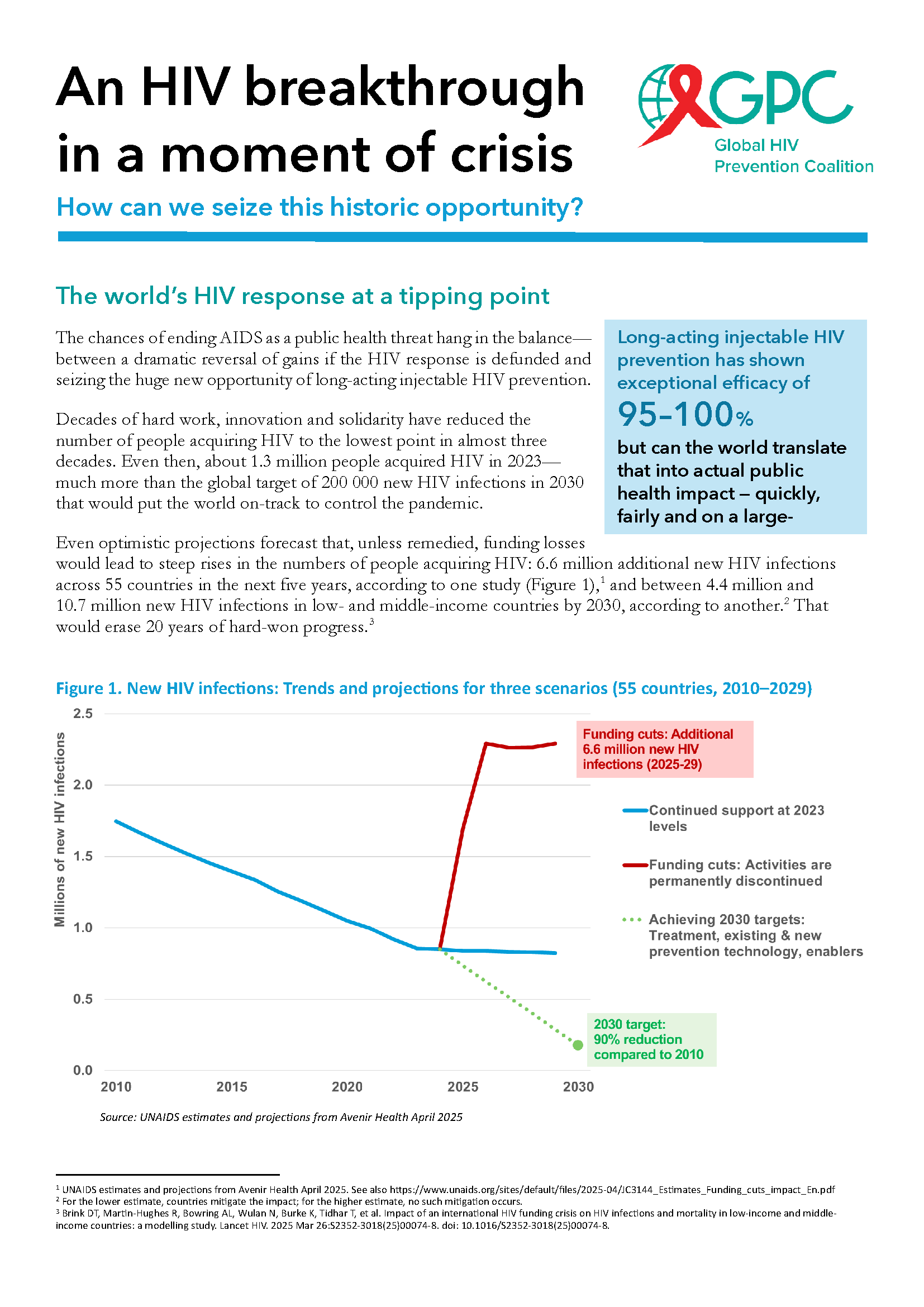
Long-acting injectables, which were hailed by Science magazine as one of the major breakthroughs in science in 2024, have shown exceptional efficacy, with lenacapavir demonstrating nearly 100% protection against HIV infection.
Despite these unprecedented advancements, the HIV response faces a dire threat from severe funding cuts. With more than 1.3 million new HIV infections annually, three times the target for 2025, financial constraints and a lack of sustained political will threaten to undo decades of progress. Global health experts warn that without urgent action to ensure continued investment, the ability to scale these life-saving technologies will be jeopardized, leaving millions at risk.
On the eve of the 78 World Health Assembly, global health leaders, government ministers, pharmaceutical companies, and civil society representatives gathered at UNAIDS headquarters in Geneva for the High-Level Multisectoral Leadership Dialogue on HIV Prevention. This High-Level dialogue, organized by the Global HIV Prevention Coalition and co-hosted by UNAIDS in collaboration with UNFPA, WHO, and UNDP, the Federal Republic of Brazil, and the Kingdom of the Netherlands, focused on accelerating access to long-acting HIV prevention technologies and advancing sustainable prevention systems.
Referring to the current funding crisis, Winnie Byanyima, Executive Director of UNAIDS, warned that “If we continue down this path, we could see an additional 6 million HIV infections and 4 million AIDS-related deaths by 2029. Put simply, we will lose control of the AIDS pandemic. But we have an opportunity today. We have new, long-acting HIV prevention tools that could fundamentally reshape the HIV response, putting us back on the right path.”
Global leaders presented successful national models from Africa, Asia and Latin America, illustrating how innovative prevention strategies are being implemented despite financial challenges. Mariangela Simao, representing Brazil, said “PrEP in Brazil is now a reality. We initially set a target of reaching 50,000 people with PrEP by 2025, but we’ve already surpassed that milestone, with 122,000 people currently using it. Our next goal is to reach 300,000 users by next year. Data shows that HIV incidence is declining in cities with more than 100,000 inhabitants where PrEP coverage is higher.”
Global HIV Prevention Coalition co-chair and CEO of AVAC, Mitchell Warren called for choice in HIV prevention.
“Condoms work well for some people and situations. Oral PrEP is safe and effective for those who can adhere to daily pill taking. The monthly dapivirine vaginal ring is a preferred option for some women, as is voluntary medical male circumcision for many men, while harm reduction is highly effective for people who inject drugs. Now, long-acting injectables offer an additional option for the many people who struggle to protect themselves from HIV and want more convenient and discreet prevention options.”
Key panel discussions focused on the cost of inaction, the significance of equity in access, and the role of long-acting prevention in the future HIV prevention toolkit.
The event underscored the urgent need for a multisectoral approach to overcoming structural barriers to prevention, including regulatory, financial, and societal challenges. The discussions highlighted that global solidarity and sustained political will are essential to closing the prevention gap and achieving the UNAIDS 2030 targets of fewer than 200 000 new HIV infections annually.
Ambassador Paul Bekkers, Permanent Representative of the Netherlands to the UN, closed the dialogue with a powerful call to action: “Not acting now means leaving a larger HIV epidemic to the next generation. Or we can put the world on course to achieve HIV epidemic control and eventually the end of AIDS as a threat to public health. As members of the Global HIV Prevention Coalition, we can achieve this together.”
As part of this pivotal moment, UNAIDS and the Global HIV Prevention Coalition launched a new brochure titled An HIV breakthrough in a moment of crisis: How can we seize this historic opportunity?
Our work
An HIV breakthrough in a moment of crisis; How can we seize this historic opportunity?





Feature Story
Global health leaders: Pandemic Agreement can help fight inequalities and AIDS
22 May 2025
22 May 2025 22 May 2025Global health leaders called for the Pandemic Agreement adopted at the 78th World Health Assembly to deliver where past efforts failed—equitable access to life-saving technologies and services during times of crisis.
The call took place during an event organized by the UNAIDS’ convened Global Council on Inequality, AIDS and Pandemics featuring senior South African diplomat, Precious Matsoso, Co-Chair of the Intergovernmental Negotiating Body for the Pandemic Agreement, UNAIDS Executive Director Winnie Byanyima, former Health Minister of Brazil Nísia Trindade, and Spain’s Health Secretary Javier Padilla Bernáldez.
The panel reflected on decades of experience from the global HIV response, how its lessons were not learned during the rollout of COVID-19 vaccines, and what needs to change before the next global pandemic crisis.
“This agreement makes it clear that a principle of pandemic response will be sharing what has been paid for publicly. This is so important for us,” Ms Byanyima told participants. “Twelve million people in Africa died waiting for HIV antiretrovirals; they say that 1.3 million lives could have been saved during COVID-19 had the vaccines been shared equitably. This agreement has laid a foundation for building on that experience and ensuring that never again will millions around the world be dying when a life-saving technology is there.”
Precious Matsoso, a former Director-General of South Africa’s National Department of Health, said that the Pandemic Agreement is “not the end in itself, but the beginning of a process” in addressing inequalities in pandemic preparedness and response, and that even while countries are ratifying the agreement, they can act on its principles and provisions.
“You don't have to wait to ensure that there is personal protective equipment for your health workforce, you don't have to wait to start strengthening your health system,” she said. “If you want products to be approved, if you want research and development to happen, if you want diversified local protection ... you don't have to wait. You can start having those measures put in place in different countries.”
Former Minister Trindade stated that, in September 2021, 76% of the world’s COVID-19 vaccine supply was concentrated in only 10% of the world’s countries. Brazil and the G20 have launched a Global Coalition on Local and Regional Production, Innovation and Equitable Access that aims to strengthen the capacities of countries to develop and manufacture health technologies for neglected disease, like Dengue, and diseases that impact vulnerable populations, like HIV.
“As technology and the scientific basis of [disease control] have advanced, at the same time, inequalities [in access] have enlarged,” Trindade said. “Diseases that were not seen as neglected became neglected, because it's not a problem of the disease, it's a problem of power, economic interest and so on.”
Ms Byanyima noted that innovative technologies for the AIDS response, such as long-acting injectable antiretroviral medicines for HIV prevention and treatment, have been slow to rollout, and global targets for pre-exposure prophylaxis, known as PrEP, will not be reached.
A promising long-acting antiretroviral from Gilead Sciences, lenacapavir, requires only two injections per year to prevent HIV infection. Gilead has signed agreements with six companies to make and sell generic lenacapavir. UNAIDS has called for more manufacturers in the Global South, and especially sub-Saharan Africa, to be granted licences, and for the generic version to be sold in more countries in order to accelerate access.
“There is this amazing technology that Gilead has invented,” Ms Byanyima said, “However, it's not yet available. And it could take years and years to become available. This is not a way to fight and win against a pandemic.”
Secretary Padilla Bernáldez said that the technology transfer provisions in the Pandemic Agreement could help accelerate access. “The pandemic agreement is going to be the framework that we are going to use when talking about lenecapavir,” Mr Padilla said. “These words on technology transfer [in the Pandemic Agreement] are maybe not the ideal that we would have chosen, but for sure, they are going to make us able to go further.”
Moderator Matthew Kavanagh, Director of Georgetown University’s Center for Global Health Policy & Politics, called on countries to make the most of the opportunities created by the historic agreement. “The Pandemic Agreement is not everything we would want, but it is the beginning of a powerful movement ... a sign that global health, despite reports of its death, is far from dead,” he said. “We can keep pushing towards something that is equitable, powerful, and improves people's health.”
Watch the full event:

Feature Story
‘My greatest fear is that we will return to the dark days of the epidemic’
21 May 2025
21 May 2025 21 May 2025UNAIDS Country Director reports on the impact of funding cuts to the HIV response
The HIV response in Zambia, known as a model of success in sub-Saharan Africa, is now facing major challenges following the abrupt and significant cuts to US funding. It has led to widespread disruption: clinics have closed, prevention services have been scaled back, and thousands have lost access to lifesaving medication. Yet the Zambian government and partners are stepping in to protect the progress made.
In this interview, UNAIDS Country Director for Zambia, Isaac Ahemesah, details the fallout from these funding decisions on health services, vulnerable communities, and the country’s ability to sustain progress against HIV-and outlines what is urgently needed to avert further health crisis.
“In 1997, life expectancy in Zambia was about 46 years due to HIV and AIDS. In 2023, it was nearly 66 years because of the investments made and the strong partnership.”
Q: How have the US funding cuts impacted the HIV response in Zambia?
Zambia has long relied on international aid, including substantial support from PEPFAR. Three years ago, the US government’s commitment stood at approximately US$ 402 million, which was subsequently reduced to US$ 392 million, and most recently to US$ 367 million. Despite these reductions, the contribution remains significant, not only to the HIV response, but to Zambia’s overall health sector. To put it in perspective, of the US$ 600 million in total US support to Zambia for development last year, US$ 367 million, around 60%, was allocated to HIV.
However, the abrupt funding cuts led to the termination of key programmes. More than 11 000 health workers supporting the HIV response, and approximately 23 000 health workers providing services for malaria, tuberculosis, and other health needs, were impacted.
Several essential initiatives were stopped. These include the closure of 32 wellness centres that served over 20 000 key populations, including LGBTQ+ people, sex workers, and people who inject drugs, across seven of Zambia’s ten provinces. These centres offered critical services such as HIV testing, treatment, and support.
All DREAMS programmes, which supported adolescent girls and young women in 22 districts, have also been shut down. This has cut off access to HIV prevention, life skills, and economic empowerment activities for thousands of vulnerable girls.
HIV prevention services have also been disrupted. Sixteen standalone centres providing voluntary medical male circumcision - a proven HIV prevention method - have ceased operations. Nearly half of Zambia’s pre-exposure prophylaxis (PrEP) services, which help prevent HIV infection, were funded by the US and have now been discontinued.
Community-led monitoring programmes, which ensured quality and accountability in HIV care, have also been terminated. Furthermore, the Smart Health electronic medical records system, along with platforms used for forecasting and quantifying medical supplies, is no longer operational, making it increasingly difficult to manage patient care and maintain drug inventories.
Q: What will happen if the DREAMS programme is not reinstated?
Currently, Zambia records approximately 23 000 new HIV infections annually, with about 8700 occurring among young people aged 15 to 24. Notably, 60% of infections in this age group happen among girls.Without support for prevention and treatment interventions, new HIV infections could surge to 180 000 per year by 2030. Among young people, infections could rise to over 60 000 annually by 2030.
Gender-Based Violence (GBV) remains a growing concern in Zambia, and each GBV case carries a heightened risk of HIV transmission. Addressing this requires a coordinated, multi-sectoral approach that extends beyond HIV alone to include family planning and reproductive health services. National partners are working to reinvigorate this multi-sectoral response so that all relevant sectors-education, gender, internal affairs, and others-actively share responsibility for the HIV response.
Given the challenges, there is a pressing need to pursue local initiatives and mobilize alternative funding sources to support adolescent girls and young women, safeguarding their health and rights.
Q: Are there concerns about supplies of HIV medicines?
Yes, there is significant concern. At present, Zambia has sufficient antiretroviral (ARV) medication to last until the end of the year. However, the US has announced an additional US$50 million cut in funding for medicines and health commodities, effective from next year, due to concerns about drug theft. This will make it extremely difficult to ensure an uninterrupted supply of ARVs, particularly for the most vulnerable populations. There have already been reports of people living with HIV receiving reduced quantities of medication - less than the standard three- to six-month supply - due to ongoing uncertainty and challenges in stock management.
Q: What is UNAIDS doing to support Zambia during this crisis?
At the onset of the US funding freeze, UNAIDS immediately partnered with the Ministry of Health to convene national leadership and all key stakeholders. This was critical to coordinate a unified and effective response to the sudden disruption. We quickly led an impact assessment to understand how the freeze was affecting Zambia’s HIV response on the ground. This provided the data needed to guide urgent decisions.
One of our first steps was to work with the government and partners, we helped define a minimum package of essential HIV services that could realistically be maintained with the reduced resources available. We costed this package at about US$ 147 million and presented it to the Cabinet and Presidency for consideration in the national budget.
At the same time, we supported the development of the HIV Sustainability Roadmap, which explores alternative domestic financing options. This includes innovative approaches such as leveraging health insurance schemes and introducing total market strategies-for example, making PrEP and vaginal rings available through pharmacies.
We also worked closely with the Ministry of Health to revise policies to better fit the current context. For example, we supported allowing longer antiretroviral therapy refills—for up to six months–—to reduce the burden on both patients and the health system. We also helped adjust HIV testing protocols to manage limited supplies more effectively and piloted new service delivery models outside traditional health facilities to expand access.
At the operational level, we partnered with WHO, UNICEF, UNFPA, and others to monitor weekly stock levels of HIV commodities, ensuring timely responses to shortages. We support civil society organizations, especially those representing key populations, in transitioning clients from closed wellness centers to public health facilities, helping maintain continuity of care.
To address broader systemic challenges, UNAIDS contributed to the restructuring plan for the Zambia Medicines and Medical Supplies Agency to improve accountability and strengthen the supply chain.
Our Resource Allocation Forecasting Tool was used to estimate the real cost of sustaining Zambia’s HIV response, which we estimated at around US$ 150 million annually. This tool helps the government and partners plan budgets more effectively.
UNAIDS acts as the central hub for information-sharing and advocacy around the impact of US funding cuts. We regularly present needs assessments to the UN Country Team and support ongoing fundraising discussions to urgently mobilize resources to sustain services.
Finally, we have supported training for health workers to promote respectful, non-discriminatory care for key populations now accessing mainstream health services. This is vital to ensure no one is left behind despite the challenges.
Q: What is the solution to ensure sustainable financing for Zambia’s HIV response, and avoid such a crisis in the future?
The key to sustainable financing lies in increasing domestic funding and reducing reliance on external donors. While the recent US funding cuts were abrupt and challenging, this situation was not entirely unexpected. For years, Zambia and other countries have been encouraged to take greater ownership of their HIV responses. The real surprise was the speed and scale of the funding reductions.
To protect its HIV response, Zambia must now mobilize domestic resources. This includes engaging local philanthropic organizations, expanding the role of national health insurance schemes, and ensuring that HIV services are fully integrated within these systems. Innovative models like risk pooling and market-based access to prevention tools, such as making PrEP and vaginal rings available through pharmacies, will also be key to expanding reach and ensuring continuity.
On the global level, the HIV response must increasingly pivot toward long-acting treatment and prevention options, such as injectable PrEP and antiretroviral treatment. These innovations can help simplify adherence and improve outcomes.
Zambia is also exploring total market approaches, where the private sector helps supply prevention and treatment services. In addition, local production of ARVs could help reduce costs and improve supply chain stability.
Critically, the country has already shown that essential HIV services can be maintained on smaller budgets, provided resources are used efficiently. But for long-term sustainability, the government must take the lead. This means prioritizing HIV in the national budget and exploring innovative domestic revenue sources, such as earmarked taxes on alcohol, tobacco, or health products.
While international partners will remain important, the responsibility for a predictable, sustainable HIV response now rests squarely with Zambia itself—to protect the lives and health of its 1.4 million citizens living with HIV, and to ensure that no one is left behind.
Q: What’s your message to the international community?
Today, I believe the global HIV response stands at a crossroads. The decisions we make now will either help the world achieve Sustainable Development Goal 3.3—the target of ending AIDS as a public health threat by 2030—or risk a devastating reversal.
If we ease up, we could see a return to the 1990s, when new HIV infections spiraled out of control, HIV-related deaths surged, and the global economy suffered greatly.
All we ask for is a final push— a sustained commitment to support countries in fulfilling their promises to end AIDS as a public health threat. I urge the US government and all other donors to reconsider the recent funding cuts. We need to keep our foot firmly on the accelerator until we reach the finish line.
Otherwise, my greatest fear is that we will return to the dark days of the epidemic, with significant increases in new infections and deaths.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads the global effort to end AIDS as a public health threat by 2030 as part of the Sustainable Development Goals.
Following the US funding cuts in January, UNAIDS is working closely with governments and partners in affected countries to ensure that all people living with or affected by HIV continue to access life-saving services. For the latest updates, please visit unaids.org
Related resources
Watch: Integration of HIV services key
Watch: Final push needed
Region/country




Feature Story
HIV is increasing among men who have sex with men in Cambodia; One organization is trying to turn the tide
21 May 2025
21 May 2025 21 May 2025Chhum Vy, an outreach worker for Men’s Health Cambodia (MHC), lives in Steung Meanchey, a low-income neighborhood in southern Phnom Penh. She has converted her rental house into a makeshift community centre for gay and transgender people who live in the area. To get there you pass through a Buddhist temple compound, then head down narrow streets, just wide enough for a motorbike.
Ms Vy has taped health promotion posters to the walls and arranges HIV testing and prevention tools in a corner of her living room floor. Clients leave their shoes at the door and sit in a circle on the ground for her sensitization sessions.
“I work every day, seven days a week, sometimes in the evening depending on the needs of the client,” she said.
She is on the frontlines, tackling the toughest challenge facing Cambodia’s HIV response. While new infections in the southeast Asian nation are declining among all other groups, they are increasing among gay men and other men who have sex with men. The reasons for this are complicated.
Ron Sopheab said he has lost many gay friends to AIDS. In the early 2000s one of his friends committed suicide when his family kicked him out of the house, refused to even eat with him and allowed him just a small bed outside.
The MHC workers and clients agree that stigma and discrimination against both men who have sex with men and people living with HIV have declined since those days.
“A little remains, but it is at a lower level,” Mr Sopheab said.
However, he noted that gaps in Cambodia’s progressive HIV response can still leave people susceptible to stigma and discrimination. Despite practicing safer sex in his regular life, Mr Sopheab contracted HIV during three months in a detention center where there was no access to HIV prevention tools. MHC provides him with peer support to remain adherent to treatment and gives him transportation support to attend the clinic when needed.
For Pom Rotha, it is extreme poverty that makes her vulnerable. As she is currently living in a rental room and sometimes cannot afford to pay the room fee, she is unable to renew her national identification. That means she cannot access the social support services that are a lifeline for many Cambodians. She survives through sex work and says about 5% of her clients insist on not using condoms.
“I cannot say ‘no’ because I need the money,” she said. “I try to negotiate, but if it does not work… I let it be.”
MHC provides Ms Rotha with pre-exposure prophylaxis, a preventive medicine known as PrEP, to help her avoid HIV infection if she is exposed. She said this is how she has remained HIV-free despite the risks she’s felt forced to take.
But another danger is far more pervasive. Young gay men are using the internet to find sexual partners either on hookup sites or social media. Many of them do not have the information or support they need to protect themselves.
That is why MHC has developed a digital strategy. This approach complements the physical testing, counselling and peer services it offers in ten provinces. Bun Pheng manages the online content and is himself an influencer. His team develops social media materials and campaigns about HIV prevention and MHC services. Every week they host a Facebook Live featuring experts or celebrity guests. A separate team is responsible for reaching out to clients through the gay social networking apps Grindr and Blued. Part of Mr Pheng’s job is to monitor the online comments, answering questions and interacting with the audience.
“If someone needs services, I refer them to an outreach worker to make an appointment where it’s most convenient,” he said.
Clients are offered a range of options to meet them where they are.
They can come in for testing or be mailed a self-test kit (one option tests at the same time for syphilis). MHC provides counselling before forwarding the testing kits and takes those with reactive results to the lab for confirmation. This varied approach is meant to help reach the 8% of people living with HIV in Cambodia who are not yet aware of their HIV status.
Ms Vy shows off a range of HIV prevention options. She demonstrates correct condom and lubricant use. Then she explains the basics of PrEP.
The Khmer HIV/AIDS NGO Alliance (KHANA) sends a mobile van out every night to provide education and testing in hotspot areas where gay men and transgender people go to find partners.
UNAIDS Country Director to Cambodia, Lao PDR and Malaysia, Patricia Ongpin, said more investments are needed for these community-led approaches tailored for men who have sex with men.
“Communities are responding to the realities of people’s lives in a way that state services can’t,” Ms Ongpin said. “To end AIDS we must channel resources to the organizations with the best chance of reaching those who are now being left behind.”
At the end of Ms Vy’s Sunday evening session clients leave with a bow and a handful of condoms.
“Self-stigma is really high,” Ms Vy reflected. “Societal stigma has reduced a lot, but some people still don’t want to access the services. I even had one case where after counselling a person still decided to stay away from services until she died. That is what we are working to address.”
Region/country





Feature Story
Client-centered services speed up Cambodia’s progress to end AIDS
20 May 2025
20 May 2025 20 May 2025Arun Seang* works six days a week in a garment factory in Phnom Penh. In the past when he needed time off to go to the HIV clinic he came up with excuses. Now there’s no need. The National Clinic for AIDS, Dermatology and STDs (NCHADS) is open every day, including weekends.
The scheduling suggestion came from a community-led monitoring exercise and community feedback. It was initially implemented as part of an Australia-supported project managed by UNAIDS. When the experiment ended, the clinic maintained a seven-day week due to its popularity.
This is one of several approaches taken to make HIV prevention and treatment services in Cambodia more user-friendly. “The staff are really nice,” Mr Seang said following his Sunday afternoon treatment consultation. “They are welcoming and also, they maintain confidentiality. I feel very safe coming here.”
Integrated community support
Cultivating a sense of trust in the delivery of HIV care has been key to Cambodia’s progress toward ending AIDS. The country is one of the front-runners to reach the 95-95-95 global targets. Currently 92% of people living with HIV are aware of their status. Almost all diagnosed people are on HIV treatment and more than 98% of those on treatment have a suppressed viral load.
These results were unimaginable when Sovann Reatrey learned she was HIV-positive, 26 years ago. “In the early days it was completely different,” she said. “Before there was a lot of stigma and discrimination. Many healthcare providers gossiped about people in the clinic and kept their distance. Now there is a welcoming environment, good communication and close physical interaction.”
At NCHADS she helps achieve this. As an Antiretroviral Users Association (AUA) counsellor her work is fully integrated into the clinic’s operations rather than an add-on. Mrs Reatrey consults with patients when they are first diagnosed and throughout their treatment journey.
“It starts as a friendly discussion. I disclose my status and tell them ‘I am also living with HIV’. Some don’t believe me. They say, ‘you look very healthy, but you are like me?’ I reassure them that it’s true. This builds trust and a relationship so they can discuss their concerns openly,” she explained. “The interaction is not as client and healthcare provider, but rather as a friend and neighbour.”
Nhem Salat, another community worker, enrolls people for HIV treatment. “I smile and encourage them to raise any issues they have when they go to see the doctor,” said Mrs Salat. “It’s all about making them feel comfortable.”
One-stop services
The waiting room isn’t hemmed in by walls. Sunlight and breeze rush through. Rows of colorful flags hang from the ceiling. The space is decidedly—perhaps deliberately—open and bright.
Huge posters invoke celebrity and safety. Singer Nicky Nicky, influencers Yaro and Sinora Roath and drag queen performer Rebecca Chan promote HIV prevention and options including condoms, PrEP (medicine to prevent HIV) and self-testing.
In addition to its standard PrEP service, this month the clinic adds long-acting cabotegravir (CAB-LA), an injectable HIV prevention option that lasts for two months, and the Dapivirine Ring (DVR), a vaginal ring which slowly releases antiretroviral medicine to prevent HIV infection.
Multiple posters invite clients to get tested. Sexually transmitted infection screenings and treatments are available. Non-communicable disease services are provided. Mental health screenings are offered to everyone. Next on NCHADS’s to-do list: more work to make the service offering youth-friendly.
By design, the space is everything for everyone.
“This clinic is a one-stop shop so people can access whatever services they need. People living with HIV don’t want to move around to different places to get healthcare,” explained the clinic’s Deputy Manager, Dr Nhem Chantha.
In his examining room, Dr Chantha, explained to Mr Seang that his viral load will be checked annually. “The U=U (undetectable equals untransmittable) message has been integrated into counseling to all clients. We have a Telegram group, and we also share information on social media platforms. This makes the clients understand the benefit of having an undetectable viral load by taking their treatment so they cannot transmit HIV. Because of this, they are very happy and really adhere to the treatment.”
UNAIDS Country Director for Cambodia, Lao PDR and Malaysia, Patricia Ongpin, noted that the emphasis on community-led care and service integration ensures impact and sustainability. “Partners in government and community are working together to find solutions that get the most out of every interaction and investment,” she said. “When services are friendly and convenient, people will use them. Then we will further reduce new HIV infections and deaths.”
*(name changed to protect privacy)
Region/country


Feature Story
UNAIDS at the 78th World Health Assembly
19 May 2025
19 May 2025 19 May 2025At the 78th World Health Assembly UNAIDS is calling for urgent action to avoid millions of avoidable HIV infections and AIDS-related deaths.
As the world faces an unprecedented international funding crisis affecting global health security, UNAIDS is calling on governments and partners attending the 78th World Health Assembly (WHA) to urgently recommit to ending AIDS by 2030. UNAIDS is warning that without immediate action to dismantle barriers to healthcare, strengthen community-led responses, and unlock sustainable financing, decades of progress could be reversed and millions of lives put at risk.
The theme of the 78th World Health Assembly is One World For Health.
During the week, UNAIDS will be advocating for continued global solidarity and sustained political and financial commitment for the global HIV response as part of broader efforts to achieve the Sustainable Development Goals. This includes the need to scale up HIV services, including access to long acting injectables for HIV prevention which are almost 100% effective at preventing infections and could help countries move towards a sustainable HIV response.
UNAIDS will also be pushing for equitable, inclusive and rights-based approaches to pandemic preparedness and response, supported by lessons learned from the gains made against HIV. This means ensuring equal access to medical innovations and the centrality of community systems, data equity, access to innovations and the protection of human rights.
UNAIDS KEY EVENTS AT #WHA78
Wednesday 21 May - 08:30 – 10:00 CET
Ending inequalities in pandemic responses - The pandemic agreement and beyond
The Pandemic Agreement is a significant step forward in pandemic prevention, preparedness and response, based on the principles of equity and the full respect for the dignity, human rights and fundamental freedoms of all persons. The panel will discuss how to ensure that those principles are adhered to as the Agreement is put into practice.
Panel members:
- Precious Matsoso, Co-Chair of the Intergovernmental Negotiating Body for the Pandemic Agreement
- Nísia Trindade, former Minister of Health, Brazil
- Winnie Byanyima, UNAIDS Executive Director
Venue: Kofi Annan room - UNAIDS/WHO D Building
*WHA delegates can use their WHA accreditation badge to enter the UNAIDS building. Other attendees must register in advance here
To follow online click here
Wednesday 21 May - 18:30 – 21:00 CET
“A new era of HIV prevention; Accelerating access to long-acting prevention options through sustainable prevention systems and financing”
This High-Level Dialogue organized by the Global HIV Prevention Coalition and co-hosted by UNAIDS in collaboration with UNFPA, WHO and UNDP, the Federal Republic of Brazil and Kingdom of the Netherlands aims to galvanize political leadership, financing, and coordinated action to drive a transformational HIV prevention push. The meeting will serve as a platform for Ministers of Health, global health partners, pharmaceutical companies, and civil society to explore opportunities to expand access to new long-acting prevention technologies as a powerful addition to existing effective options.
Join UNAIDS leadership, representatives of UN partners and global health stakeholders as they discuss these issues with Ministers of Health, community representatives and leaders of pharmaceutical companies developing long-acting prevention options.
Venue: Kofi Annan room - UNAIDS/WHO D Building
Watch the livestream here
Thursday 22 May - 08:30 – 10:30 CET
The future of domestic health financing is now: Africa’s pathway for sustainable health systems
The panel discussion will explore how best to achieve financial sustainability of the health sector from different perspectives. Topics would include raising more money through innovative means, improving efficiency, strengthening planning and coordination, public-private partnerships as well as discussing the roles of different actors, including donor partners, and the institutional reforms necessary for success.
Co-organised by the Ministry of Health & Social Welfare of Nigeria, the Global Fund, WHO, UNAIDS and other partners
Venue: Ballroom AE, INTERCONTINENTAL GENEVE
Thursday 22 May - 18:30 – 20:30 CET
Communities at the heart of global health and health security: Why sustained funding for community-led health systems matters now more than ever.
Co-organised by UNAIDS, Coalition PLUS, Frontline AIDS and WHO, this event will bring together Ministers of Health, civil society leaders, donors, and global health institutions to explore sustainable solutions to safeguard and scale up community-led health systems amid global crises and decreasing aid.
Venue: Kofi Annan room - UNAIDS/WHO D Building
To attend in person, please register here
To attend online, please register here