Feature Story
A big year ahead for TB
19 March 2018
19 March 2018 19 March 2018The year 2018 is critical for the international community as it pushes progress towards ending the global tuberculosis (TB) epidemic by 2030 as part of the Sustainable Development Goals.
In September 2018, United Nations Member States will come together in New York for the United Nations High-Level Meeting on Tuberculosis to show their political leadership and commitment to ending TB by 2030. Some of the main challenges in the response, including the need for equity and to ensure vulnerable groups have access to TB services, will be addressed at the high-level meeting, as will the need to make TB testing and treatment available through primary health-care services and the urgent need to mobilize resources.
In preparation for this historic event—the first ever United Nations high-level meeting on TB—leaders from across the globe converged in New Delhi, India, on 14 and 15 March, for the End TB Summit, part of which was the 30th Stop TB Partnership Board Meeting.
A large number of global leaders on TB gathered at the meeting. J. P. Nadda, the Union Minister of Health and Family Welfare, India, said during the event, “We will ensure that commitments to end tuberculosis made are fulfilled. Achievement of the goals will need innovations as well as new implementation ideas. India stands committed to support neighbouring countries in the fight against the disease.”
In 2016, the estimated funding gap for TB programming was US$ 2.3 billion. In addition, there was a US$ 1.2 billion shortfall in TB research and science. The urgent need for increased investments in innovation will be highlighted in the lead-up to the high-level meeting as part of efforts to bring 21st century diagnostics and treatments and a vaccine to the response to TB.
“Leaders across the globe need to seize this opportunity, make bold commitments and take a resolve to see the end of tuberculosis on a fast track. Actions to follow the commitments will need bold actions by health ministries, other ministries, the private sector, civil society and communities,” said Isaac Folorunso Adewole, the Minister of Health of Nigeria.
TB has been around for thousands of years, yet TB still remains a major global health crisis. The World Health Organization estimated that in 2016 around 1.3 million people died of TB and that a further 400 000 people living with HIV died from TB/HIV coinfection (reported globally as AIDS-related deaths).
“We cannot eliminate tuberculosis with only a top-down approach. We must work together to empower communities to support the fight against tuberculosis. This movement must go far beyond the medical community,” said Soumya Swaminathan, the Deputy Director-General of the World Health Organization.
People living with HIV are particularly affected by TB. One in 10 TB cases occurs among people living with HIV and one in four TB deaths is associated with HIV. Despite being preventable and curable, in 2016 TB was the ninth leading cause of death worldwide.
“There are a lot of people still not accessing treatment. We need to look at strategies to increase access to care, particularly for those most marginalized and not accessing care right now,” said Tim Martineau, the Deputy Executive Director, a.i, at UNAIDS.
UNAIDS and the Stop TB Partnership have a long-standing collaboration working together to advocate for, monitor and support programmes for people and countries affected by the joint global TB and HIV epidemics. The Stop TB Partnership Board provides leadership and direction, monitors the implementation of agreed policies, plans and activities of the partnership and ensures smooth coordination among Stop TB Partnership components.
Related




Feature Story
The need for a holistic approach to women and HIV
16 March 2018
16 March 2018 16 March 2018It has long been recognized that the response to HIV can’t exist in isolation, but must be integrated within a broader health and development agenda. A daylong event set out to understand better how three areas critical to women living with HIV—cervical cancer, hormonal contraception and female genital schistosomiasis (FGS)—intersect.
The importance of taking a holistic approach to girls and women and their sexual and reproductive health and rights was a central theme of the event. Held on the sidelines of the 62nd session of the Commission on the Status of Women, the event highlighted the possibilities of recent technological and medical advances to improve women’s health.
Setting the scene, Ebony Johnson, from the Global Coalition on Women and AIDS, said, “Too often women are unheard, forgotten, underserved, improperly researched—I invite and implore you to go in a new direction so that change truly comes.”
Women living with HIV are more likely to have the human papillomavirus (HPV) and are five times more likely to develop cervical cancer, which kills approximately 250 000 women each year. To emphasize the scale of the problem, Vikrant Sahasrabuddhe, of the National Cancer Institute, United States National Institutes of Health, noted that, “In the past 20 minutes of the presentation, 20 women were newly diagnosed with cervical cancer and 10 women died from cervical cancer.”
A disease that mostly affects low- and middle-income countries, where 90% of all new diagnoses and deaths occur, cervical cancer is, however, preventable through the HPV vaccine and treatable if diagnosed early.
New technology has been developed to screen women for HPV DNA or tell-tale proteins that are the signs of cervical cancer. And new tools are allowing early treatment even in clinics with limited resources. The event heard how global partnerships, including the United Nations Joint Global Programme on Cervical Cancer Prevention and Control, which UNAIDS is a part of, are committed to reducing the burden of disease, and how national HIV programmes are at the forefront of efforts to roll-out these new services to women living with HIV in order to lessen the toll that cervical cancer continues to take worldwide.
While giving women the opportunity to control how many children they have, and when, concern has been raised about long-lasting injections of a progestogen, specifically depot medroxyprogesterone acetate (DMPA). Studies have suggested that DMPA may be associated with an increased risk of HIV acquisition. Currently, more than 150 million women worldwide use hormonal contraception and there is a high proportion of women using injectable hormonal contraception in sub-Saharan Africa, where there is also high HIV incidence.
A large-scale trial—the Evidence for Contraceptive Options and HIV Outcomes (ECHO) study—which is hoped to settle the uncertainty of DMPA use and HIV risk association, is ongoing. The difficult decisions that will need to be made should the study confirm the elevated risk for HIV from the use of DMPA were discussed by the participants —the decisions will clearly have to be balanced against the known benefits of a highly effective contraceptive and will affect millions of users.
“Both HIV and unintended pregnancy remain global health priorities. As we discover the potential risk of hormonal injectable contraceptives for HIV acquisition, women need accurate information to be able to exercise informed contraceptive choices,” said Nelly Rwamba Mugo, from the Kenya Medical Research Institute.
FGS, also known as bilharzia, is a disease that is often neglected, but affects some 55 million girls and women. With FGS, bleeding during sex results from lesions in the vaginal walls and ulcers in the cervix. These lesions put women who live with FGS at a higher risk of contracting HIV. However, cheap and effective treatment in childhood of girls who are infected with the parasite that causes FGS can stop its development later in life.
“Genital inflammation increases the risk of HIV acquisition. We need more research on coinfections, treatment of schistosomiasis and related HIV prevention strategies to help form policies that protect women’s health,” said Pragna Patel, from the United States Centers for Disease Control and Prevention.
How to scale up treatment and prevention options, and how to ensure synergy between HIV programmes and schistosomiasis control programmes in a country, were key areas of focus during the day’s discussions.
Throughout the day, how to integrate rights, services and HIV was a recurrent theme. Speakers from UNAIDS, the World Health Organization, research centres and hospitals stressed the need to seek out synergies and collaborate in order to build a cross-cutting AIDS response.
“The symposium provided a great opportunity for a wide range of people, from community activists to laboratory scientists and from young students to scientists and experienced policy-makers, to share and discuss their breadth of perspectives,” said Peter Godfrey-Faussett, Senior Adviser, Science, at UNAIDS.
The event, Improving Women’s Health: HIV, Contraception, Cervical Cancer and Schistosomiasis, was held on 15 March at the New York Academy of Sciences in New York, United States of America.

Feature Story
Improving data on key populations
14 March 2018
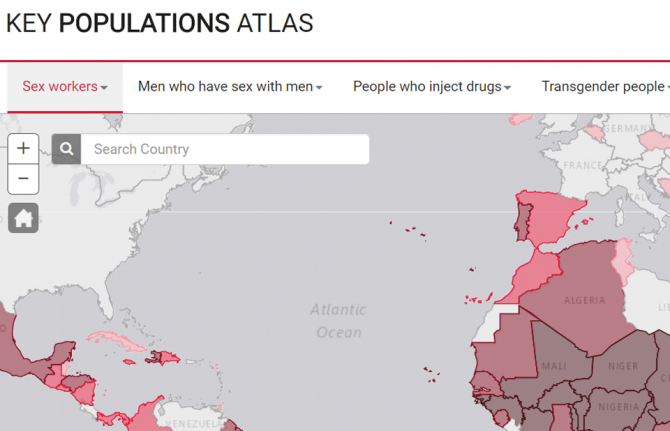
14 March 2018 14 March 2018UNAIDS has relaunched its Key Populations Atlas. The online tool that provides a range of information about members of key populations worldwide—sex workers, gay men and other men who have sex with men, people who inject drugs, transgender people and prisoners—now includes new and updated information in a number of areas. And in addition to data on the five key populations, there are now data on people living with HIV.
Chief among the new data is information on punitive laws, such as denial of the registration of nongovernmental organizations, and on laws that recognize the rights of transgender people. The overhaul of the site was undertaken in consultation with representatives of civil society organizations, including the International Lesbian, Gay, Bisexual, Trans and Intersex Association, which supplied some of the new data on punitive laws.
Data on the number of users of Hornet—a gay social network—in various countries has been made available for the atlas by the developers of Hornet, while Harm Reduction International supplied information on the availability of harm reduction programmes in prisons.
“Having data on the people who are the most affected by HIV is vital to getting the right HIV services available at the right locations” said Michel Sidibé, the Executive Director of UNAIDS. “The Key Populations Atlas allows UNAIDS to share the information we have for the most impact.”
The Key Populations Atlas is a visualization tool that allows users to navigate country-specific subnational data on populations particularly vulnerable to HIV. Data are presented on, for example, HIV prevalence among people who inject drugs in 11 sites in Myanmar, key populations sizes, antiretroviral therapy coverage among gay men and other men who have sex with men in 13 sites in India and specific prevention services and preventive behaviours. Updated data on many indicators that were obtained through the Global AIDS Monitoring exercise undertaken in 2017 is now available on the website.
Over the coming weeks, information on people living with HIV will be expanded, with new indicators being added, and data from the 2018 Global AIDS Monitoring will be added when available later in the year.
Key Populations Atlas
Related



Feature Story
UNAIDS staff share global experience on AIDS through criss-crossing the world
19 March 2018
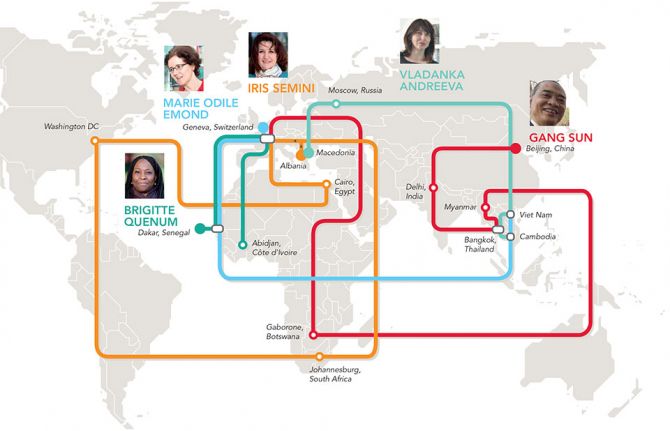
19 March 2018 19 March 2018When Marie-Odile Emond first arrived in Cambodia, she didn’t realize that some of the UNAIDS/International Labour Organization policy on HIV in the workplace she had heard discussed, years back, at the global level would be something she would see implemented.
“It seemed so abstract and yet here I was seeing it in practice,” she said, referring to health and human rights protection for workers, notably sex workers, which involved the Ministry of Labour, the community and the United Nations. “As the Country Director, I facilitated the dialogue and training for that to happen,” Ms Emond said, “and now it serves as an example for other countries.”
She now heads the Viet Nam Country Office, which she said offered another set of challenges and opportunities.
“I have found it really interesting to alternate between global, regional and country offices, because each offers a window to a part of our strategy,” Ms Emond said. Rattling off the many countries she has worked in at UNAIDS, she laughed and said, “Oh, and before UNAIDS, I worked in Armenia, Burundi, Liberia and Rwanda.”
In her opinion, meeting so many committed people from all walks of life and building bridges with them has been enriching. It’s made all the difference, according to her, in the AIDS response. “I play the coordinator, but I also had an active role in making people believe in themselves,” Ms Emond said.
Country Director Vladanka Andreeva said that her moves within UNAIDS were a huge change each time. She has served across two regions in different roles and credits her professional growth to her colleagues and the various communities she has interacted with.
“In every new post there was a challenge to quickly adapt to it, establish relationships with stakeholders and make a contribution,” she said. “You really have to hit the ground running.” Her role as the Treatment and Prevention Adviser in the UNAIDS regional office in Bangkok, Thailand, before going to Cambodia, really stands out for her. Ms Andreeva provided technical advice and assistance to strengthen HIV programmes across the region. This involved facilitating knowledge and sharing best practice, in and between countries, on innovative delivery models to scale up access to evidence-informed services.
She added that, from the former Yugoslav Republic of Macedonia to Cambodia, “my family and I explored the cultural heritage of our host countries, tasted some of the most delicious pho, tom yum and amok, and made friends from all over the world.”
She thanked her husband and daughter for being fantastic partners in the journey, since moving every four to five years is no small task. UNAIDS staff move routinely from one duty station to another, criss-crossing the world throughout their careers.
Her real pride is seeing her 17-year-old daughter, who was six when they started living abroad, become a truly global citizen, with such respect for diversity.
Gang Sun echoed many of Ms Andreeva’s points. “Because we interact with so many stakeholders, from the private sector to government to civil society, I have learned to always show respect and always listen,” he said.
For him, the journey started in the field in China, India and Thailand, followed by Myanmar and Botswana, before starting his new job at UNAIDS headquarters in Geneva, Switzerland, in 2017. He described that adapting to different cultures has kept him on his toes. “Overall, in my career I have seen every challenge as an opportunity and I have gained in confidence,” he said.
What fascinated him the most was the differences between working in high HIV prevalence countries and in countries where the epidemic was concentrated among key populations. In his new role at headquarters, he now taps into his expertise gained along the way as well as that of so many colleagues within UNAIDS and the World Health Organization.
“Despite all my experience, I still have more learning to do,” Mr Sun said.
The Côte d’Ivoire Country Director, Brigitte Quenum, jumped at the opportunity to go to the field after more than five years in Geneva. As the Partnerships Officer with francophone countries at UNAIDS headquarters, she said she learned a lot about how the UNAIDS Joint Programme functioned. That has helped her in her current role working hand in hand with Cosponsors, financial partners and civil society.
Before working in Geneva, she worked in the western and central Africa regional UNAIDS office in Dakar, Senegal. “I have gone full circle, and that has been very rewarding, because I know how the entire organization functions,” Ms Quenum said. Reflecting on the recent change in her life, aside from adjusting to the muggy coastal weather and the sheer population size of Abidjan, Côte d’Ivoire—the city has as many people as all of Switzerland—she said, “Being on the ground gives one’s job more of a sense of urgency, but I think it’s because we have daily contact with the multiple communities we’re serving.”
More in this series: It’s about the people we serve: UNAIDS staff connecting the world
Related




Feature Story
Human touch and targeted screening help to reduce HIV outbreak in Athens
16 March 2018
16 March 2018 16 March 2018Greece experienced a large increase in 2011 in the number of new HIV infections among people who inject drugs. The number of new diagnoses in Athens usually hovered around 11 per year, but shot up to 266. For the first time, injecting drug use and sharing needles became the main source of new HIV infections in Greece, according to the Medical School of the National and Kapodistrian University of Athens.
In response, the university, along with the Greek Organisation against Drugs and other nongovernmental organizations, launched a programme to “seek, test, treat and retain”, under the name Aristotle, in order to put a halt to the outbreak.
Their first challenge was finding people who inject drugs and identifying if they were HIV-positive.
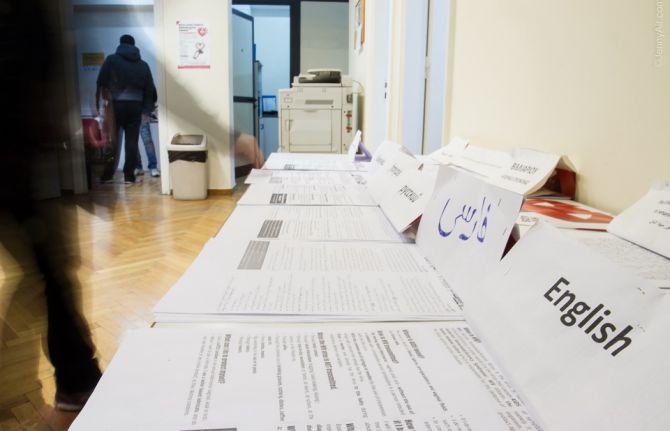
“Many lived on the streets, some had been in prison and in many instances they were migrants with no knowledge of Greek,” said Vana Sypsa, Assistant Professor of Epidemiology and Preventive Medicine at the National and Kapodistrian University of Athens and a lead on Aristotle, along with Angelos Hatzakis, Meni Malliori and Dimitrios Paraskevis.
She explained that because of the economic recession, people lost their jobs and shared injecting equipment with other people, and homelessness crept up. In addition, she added, sterile syringes were hard to come by and opioid substitution therapy centres had long waiting lists. The Aristotle programme used a coupon system so that peers could recruit people to come in for an HIV test in return for a stipend.
Ms Sypsa explained that the centre provided food, as well as condoms and syringes. Positive Voice, an association of people living with HIV, helped with HIV counselling, while Praksis focused on facilitating language services and identity papers for migrants.
Nikos Dedes, the head of Positive Voice, said that it played an active role during the diagnosis and referral part of the programme. “We guided them through the maze, which increased the retention of people,” he said. Mr Dedes believes that Aristotle contributed to raising awareness of HIV among people who inject drugs. “For many, HIV was a wake-up call to dealing with their drug addiction,” he said.
The programme had five rounds of recruitment in 2012 and 2013, with some participants taking part in more than one round. Aristotle’s services were provided to more than 3000 people. About 16% of the participants tested positive for HIV and had the opportunity of immediate access to antiretroviral therapy, with social workers arranging appointments. They also had priority access to opioid substitution therapy.
Ms Sypsa said that even before the end of the programme, there was a 78% decline in new HIV infections in Athens.
“Aristotle averted 2000 new HIV infections and we noted a decrease in high-risk behaviour among people injecting drugs at least once a day,” Ms Sypsa said.
She added that aside from containing an outbreak, all those involved in the programme were proud to have changed the lives of many people, linking them to HIV care and treatment.
The programme’s success drew a lot of attention. After the end of the programme, “People kept stopping by the site, looking for Aristotle employees. We had become a reference point for them,” she said.
Five years later a new programme is being started, but this time with an aim to increase care and treatment for HIV and hepatitis C for people who inject drugs.
And Mr Dedes is ecstatic, because this time Positive Voice is an integral part of the programme, with a budget. A new partner has also joined—the liver patient association Prometheus will spearhead the response to hepatitis. Mr Dedes said, “This is a true testament to the success of the programme—incorporating people from the communities.”


Feature Story
Much more than just sterile needles
12 March 2018
12 March 2018 12 March 2018The biggest question I always ask clients is, "Are you willing to change?". Charles describes his role at the Saskatoon Tribal Council Health Centre as "here to help". "We have the resources that can and will help, if and when people want and need them. I know where to point people to for housing, food and shelter. If they want detox, I know where to go—I’m very familiar with the treatment centres and I’m very familiar with the treatment cycle."
Charles is an addictions counsellor at the centre and is himself a former addict.
After almost 16 years as an alcoholic, and six years using drugs, Charles understands the issues first-hand. Charles is particularly aware of the challenges his clients endure as single parents. A single father of three, his deteriorating relationship with his children was the catalyst for him to seek help. "I didn’t really realize I had a problem, because it was so normalized. Alcohol was normal, drugs were normal, it was all normal. I went to treatment in 2007. But I knew it would be a struggle to get out."
Saskatoon is the largest city in the Canadian province of Saskatchewan, a province where young indigenous people are more likely to end up in jail than to graduate from high school and suicide rates are five to seven times higher than among the nonindigenous population. There are high rates of drug and alcohol addiction and complex mental health conditions.
HIV and tuberculosis (TB) are also major health concerns among many indigenous communities. Among First Nations people in Saskatchewan, TB is 31 times the national average and the HIV rate is 11 times the national rate. Around 50% of HIV infections are through injecting drug use.
There are also high levels of stigma and discrimination in the mainstream health-care system, which is why the Saskatoon Tribal Council Health Centre is an important link to health care that the clients feel safe accessing.
At the clinic, Charles sees around six to 18 people a day. His clients come from all over the Saskatoon area, from different backgrounds and different ethnicities, with ages ranging from 18 to 60 years.
"Each and every one of them has a problem with alcohol and drugs. They come from poverty, from homelessness. They can be street people and come from very intense backgrounds. Their stories are unique, sometimes devastating to the core in terms of what they have been exposed to. But they all share one thing, they’re here because they trust us."
The centre is open 365 days a year offering health and support services. The centre offers a needle and syringe programme, providing people with sterile injecting equipment to ensure that people who inject drugs do not share syringes and needles. The clinic also offers a safe space for clients to dispose of used needles and syringes. The centre gets through more than 1.5 million sterile needles every year and has a growing client base of 2600 people, with more joining every day.
The Saskatoon Tribal Council is tackling a chronic drug and mental health crisis among indigenous people. The main objective of the centre is that it is a comprehensive, multidisciplinary drop-in clinic at the heart of Saskatoon’s low-income neighbourhoods, providing a wide range of services to treat HIV and other sexually transmitted infections and hepatitis C, particularly for people of aboriginal ancestry.
The Saskatoon Tribal Council Centre is much more than just a place to get sterile needles. It is a hub, an important centre for resources and connections, a safe space and discrimination-free zone to go for help and advice. It is somewhere clients know they will be welcomed with a warm smile, a hot drink and something to eat. Staff member Twila sums it up, "People need us, and we’re making a difference."
The 61st session of the Commission on Narcotic Drugs (CND) is taking place in Vienna, Austria, from 12 to 16 March 2018. The CND is the United Nations organ with prime responsibility for drug control. In line with its mandates, the CND monitors the world drug situation, develops strategies on international drug control and recommends measures to address the world drug problem.
UNAIDS urges all countries to adopt a people-centred, public health and human rights-based approach to drug use and for alternatives to the criminalization and incarceration of people who use drugs. Evidence shows that harm reduction approaches such as the Saskatoon needle–syringe programme reduce the health, social and economic harms of drug use to individuals, communities and societies. They do not cause increases in drug use. UNAIDS urges all countries to ensure that people who inject drugs have access to harm reduction services, including needle–syringe programmes and opioid substitution therapy.
Commission on Narcotic Drugs


Feature Story
Measuring homophobia to improve the lives of all
08 March 2018
08 March 2018 08 March 2018A new index to measure levels of homophobia that can show the impact that homophobia has on countries has been developed.
Homophobia—defined here as any negative attitude, belief or action towards people of differing sexual orientation or gender identity—has long been known to affect public health. Gay men and other men who have sex with men who face stigma are more likely to engage in sexual risk behaviours, are less likely to adhere to antiretroviral therapy and have lower HIV testing rates. Knowledge of levels of homophobia, especially in low- and middle-income countries, is scant, however.
The new index, published in the European Journal of Public Health, combines both data on institutional homophobia, such as laws, and social homophobia—relations between people and groups of people. Data for the index were taken from a wide range of sources, including from the United Nations, the International Monetary Fund and the International Lesbian, Gay, Bisexual, Trans and Intersex Association. More than 460 000 people were asked questions on their reactions to homosexuality through regionwide surveys that were also used as sources for the index.
The Homophobic Climate Index gives estimates for 158 countries. Western Europe was found to be the most inclusive region, followed by Latin America. Africa and the Middle East were the regions with the most homophobic countries, with the exceptions of South Africa and Cabo Verde, which were among the top 10 most inclusive low- and middle-income countries. Among low- and middle-income countries, Colombia was the most inclusive, and Sweden was the most inclusive of all countries.
From comparing the results of the index with other data, the researchers found that countries with higher levels of homophobia were the same countries that face higher levels of gender inequality, human rights abuses, low health expenditures and low life satisfaction. Increases in a country’s Homophobic Climate Index were found to be associated with a loss of male life expectancy and a lower economic output.
The index therefore shows the damaging effects that homophobia has on the lives and well-being of everyone in a county, not just gay men and other men who have sex with men. “This index provides communities with sound data that can help them in their advocacy for more inclusive societies,” said Erik Lamontagne, Senior Economist Adviser at UNAIDS.
With knowledge of the harmful effects of homophobia, countries will be in a much better position to respond to it and improve the lives of all.
European Journal of Public Health


Feature Story
UNAIDS a top-nine gender-responsive organization
08 March 2018
08 March 2018 08 March 2018UNAIDS has emerged as a top performer in the first Global Health 50/50 report.
Global Health 50/50, an initiative that monitors the gender-responsiveness of influential global health organizations, reviewed 140 major organizations working in or influencing global health. According to the new report, UNAIDS is among the top nine health organizations in the world.
Published on 8 March, International Women’s Day, the Global Health 50/50 report was inspired by a growing concern that too few global health organizations define, programme, resource or monitor gender in their work on health or in the workplace. The report aims to show both the challenges and the way forward.
The report shows that UNAIDS has not only policies that address gender, but also concrete and time-bound gender parity targets, as set out in its Gender Action Plan. Under the plan, UNAIDS has seen the proportion of female staff rise, so that women account for 54% of UNAIDS staff. And female leaders in the field are increasing, with women accounting for 48% of UNAIDS country directors, up from 27% in 2013.
“The Global Health 50/50 survey has shown that UNAIDS’ commitment to gender equality is strong. I am resolved to building on our results and achieving all the targets of the UNAIDS Gender Action Plan,” said Michel Sidibé, Executive Director of UNAIDS.
In addition to its commitment to gender equality and its workplace gender policy, UNAIDS was marked highly for having a definition of gender in its public statements, strategies or policies and having a programmatic gender strategy that seeks to improve health for everyone.
UNAIDS has long strived for gender equality and women’s empowerment, both within the UNAIDS Secretariat and elsewhere, and has recently started to review its practices and recommitted to ensuring adherence to them.
Guaranteeing the rights and empowerment of women and girls is not only a moral obligation, but a development imperative and a smart investment that safeguards the health of women and girls. Eliminating gender inequalities is one of the 10 Fast-Track commitments that Member States made at the 2016 United Nations General Assembly High-Level Meeting on Ending AIDS.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Global Health 50/50




Feature Story
Communities at the heart of the AIDS response in Zambia
07 March 2018
07 March 2018 07 March 2018Zambia has made good progress in its AIDS response. In 2016, the country had more than 800 000 people on HIV treatment, with 83% of pregnant women living with HIV accessing it. To better understand the progress, and the challenges, Michel Sidibé, UNAIDS Executive Director, visited the Chilenje health facility in Lusaka, Zambia, during a visit to the country from 5 to 7 March.
The Chilenje facility offers HIV treatment, a prevention of mother-to-child transmission of HIV programme and tailored services for adolescents and young people. At the facility’s youth-friendly space, peer educators facilitate service uptake by young people and reach out to schools and other groups within their community with counselling and sensitization.
“We need to build cities of the future where services are not only available to people, but they are also tailored to their needs. This is the rationale behind the Fast-Track cities initiative, of which Lusaka is an excellent example,” said Mr Sidibé during his visit.
The facility offers extended hours in the evening and weekends so that people who are unable to access health services outside of standard operating hours can access HIV treatment and other services.
“Young people often fall through the cracks of the health system for fear of judgement or stigma. Owing to the large number of adolescents and young people in our community, we have set up a youth-friendly space,” said Malinba Chiko, the Superintendent of the Chilenje health facility.
Earlier in the day, Mr Sidibé met with members of civil society, who raised the issue of access to HIV and sexual and reproductive health services for key populations, especially gay men and other men who have sex with men and sex workers. Mr Sidibé reiterated that civil society is at the heart of the AIDS response and, for it to be sustainable, the voice and decision-making of civil society are essential.
Region/country




Feature Story
Leveraging education to improve health and end AIDS
02 February 2018
02 February 2018 02 February 2018During the Global Partnership for Education meeting on 2 February, hosted by Senegal and France, UNAIDS Executive Director Michel Sidibé discussed the importance of education and health. “Integrating education and health is key for our success in controlling the epidemic among young people. Without effective, quality and sustainable health and education systems we are failing young people”, Mr Sidibé said. Credit: UNAIDS/B. Deméocq.
The First Lady of Senegal, Marieme Faye Sall, and the First Lady of France, Brigitte Macron, inaugurate a cardio-paediatric centre that provides surgical treatment for children affected by cardiologic diseases. The centre, funded by the Cuomo Foundation in Monaco, supports women and children in Senegal. Credit: UNAIDS.
Preventing mother-to-child transmission of HIV is crucial, as is community involvement, stressed Mr Sidibé during his meeting with Ms Sall. The western and central Africa region lags behind in access to treatment and prevention, which is why UNAIDS and partners launched a western and central Africa catch-up plan. Credit: UNAIDS/B. Deméocq.
Mr Sidibé also met with the Minister of Health and Social Action of Senegal, Abdoulaye Diouf Sarr, stressing that no matter who you are or where you are from, everyone has the right to health, the right to an education, the right to equal opportunities and the right to thrive. Credit: UNAIDS/B. Deméocq.
The Secretary General of the Organisation Internationale de la Francophonie, Michaëlle Jean, will raise the issue of counterfeit medicines at the upcoming World Health Assembly in May. Credit: UNAIDS/B. Deméocq.
Minister of International Development of Norway, Nikolai Astrup, and Mr Sidibé met on the sidelines of the meeting. Credit: UNAIDS/B. Deméocq.
Mr Sidibé, along with the Ambassador of Luxembourg, Nicole Bintner. Luxembourg has been an active participant and donor in the western and central Africa catch-up plan. Credit: UNAIDS/B. Deméocq.
Good health enables a girl to thrive, to grow, to think, to explore and to contribute to her community. Knowledge of how to stay healthy and access to quality health services enable her to prevent illness, to eat well, to manage her sexual health, to have healthy babies when and if she chooses to and to nurture her own well-being. Education and health are two of the most transformative elements of a girl’s life. Credit: UNAIDS/B. Deméocq.
Region/country
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025