Feature Story
New framework to eliminate transmission of HIV from mothers to their babies
28 March 2011
28 March 2011 28 March 2011
(from left) Helen Jackson, UNAIDS, Senior HIV Prevention Adviser, ESA; Elhadj As Sy, UNICEF Regional Director for Eastern and Southern Africa (ESA); Tigest Ketsela, Director, Family and Reproductive Health, World Health Organization (WHO), Africa Region; Michael Klaus, Regional Chief of Communication, UNICEF ESARO.
The elimination of mother-to-child transmission of HIV in Eastern and Southern Africa has come a step closer with the endorsement of a new regional framework following a three-day consultation in Nairobi, Kenya earlier this month.
The consultation brought together government representatives from 15 high-burden countries[i], civil society organizations and donors. They were joined by the UN Children’s Fund (UNICEF), the Joint United Nations Programme on HIV/AIDS (UNAIDS), the World Health Organization (WHO) and the UN Population Fund (UNFPA).
In 2009 some 370,000 young children were newly infected with HIV. It was noted that although the scale of the problem of mother-to-child transmission of HIV cannot be underestimated, there is much that can be done. According to Elhadj As Sy, UNICEF Regional Director for Eastern and Southern Africa, “We now have the leadership at all levels to bring this number down. We know what works. Now is the time to act and make a difference. An AIDS-free generation by 2015 is possible.”
Championing both new and existing interventions
Partners endorsed the UNAIDS call for the virtual elimination of mother-to-child transmission of HIV by 2015 and adherence to the new WHO guidelines that recommend giving pregnant women and new mothers a combination of three antiretroviral drugs. They also pledged to vigorously pursue all four components of the internationally agreed UN strategy to dramatically reduce mother-to-child transmission.
There was an acknowledgement that a different approach is needed if the elimination target is to be achieved. A series of priority actions—which include enhanced support for existing programmes and strategies to implement new ones—were defined:
- Improving coverage access and use of services
- Strengthening the quality of existing interventions
- Integrating efforts to prevent mother-to-child transmission into routine antenatal and reproductive health services
- Making paediatric HIV care a routine part of child health services
- Promoting health systems development
- Improving measurement of programme performance and impact assessment
- Engaging communities more fully
The partners also agreed to work on ensuring that all pregnant women and their partners are counselled and tested during their first antenatal care visit.
Room for optimism
If countries continue rapid scale up of quality, comprehensive PMTCT service access, the goal of elimination of HIV transmission from mother to infants by 2015 can be achieved
Helen Jackson, Senior HIV Prevention Advisor for UNAIDS in Eastern and Southern Africa
Although many pregnant women are still falling through the treatment coverage net, in recent years scaled up prevention of vertical transmission efforts have been effective. According to UNAIDS 2010 estimates, in southern Africa in 2009 an estimated 130,000 infants were newly infected, more than 30% fewer than in 2004. In Botswana, Namibia, South Africa and Swaziland treatment coverage has reached more than 80%[ii]. Given these figures, and the possibility that they can be achieved across the region, participants in the consultation expressed optimism.
“If countries continue rapid scale up of quality, comprehensive PMTCT service access, the goal of elimination of HIV transmission from mother to infants by 2015 can be achieved,” said Helen Jackson, Senior HIV Prevention Advisor for UNAIDS in Eastern and Southern Africa. “We have joined forces to make sure this happens.”
[i] South Africa, Mozambique, Uganda, United Republic of Tanzania, Kenya, Zambia, Malawi, Zimbabwe, Ethiopia, Angola, Burundi, Lesotho, Botswana, Rwanda, Swaziland and Namibia.
[ii] Ibid
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025
 Impact of US funding cuts on HIV programmes in Uganda
Impact of US funding cuts on HIV programmes in Uganda

19 March 2025

Feature Story
Treatment 2.0: Translating concept into practice to overcome the HIV epidemic
24 March 2011
24 March 2011 24 March 2011
How to translate the concept of Treatment 2.0 into practice was the topic of discussion at a seminar organized by UNAIDS and WHO on 18 March at the UNAIDS Headquarters in Geneva.
How to translate the concept of Treatment 2.0 into practice was the topic of discussion at a seminar co-organized by UNAIDS and the World Health Organization (WHO) on 18 March at UNAIDS Headquarters in Geneva. Staff members from both organizations participated in the event together with colleagues from the Global Fund, the International AIDS Society and UNITAID.
“We need to find innovative solutions to overcome the HIV epidemic,” said Dr Bernhard Schwartländer, UNAIDS Director of Evidence, Strategy and Results Department and the seminar’s organizer. “Innovation to improve treatment regimens but also innovation in the way we approach the AIDS response.”
Treatment 2.0 is a concept launched in November 2010 by UNAIDS and WHO that calls for a radically simplified treatment platform. Its viability and implementation at country level will determine the level of success in the response to HIV in the coming years.
Craig McClure, Senior Adviser on Treatment 2.0 at WHO and Mariangela Simao, UNAIDS Chief, Prevention, Vulnerability and Rights, jointly presented on “Catalyzing the Next Phase of Treatment”. They outlined the five pillars on which the Treatment 2.0 initiative is based: optimizing drug regimens, simplifying laboratory platforms for diagnosis and monitoring; reducing costs; adapting delivery systems and mobilizing communities.
We need to find innovative solutions to overcome the HIV epidemic. Innovation to improve treatment regimes but also innovation in the way we approach the AIDS response
Bernhard Schwartländer, UNAIDS Director of Evidence, Strategy and Results Department
Mr McClure recognized that, while some of the innovations in drugs and diagnostics are years away, there are many actions that countries can take now to simplify treatment and make it more efficient,. For example, choosing to purchase one-pill-per-day fixed dose drug combinations, legal reform to use TRIPS flexibilities to reduce costs, integrating HIV treatment with prevention services and other areas of health care where appropriate and involving communities more intensively in designing and delivering HIV services.
On this topic, David Barr from the International Treatment Preparedness Coalition gave specific examples that show how involving communities in managing treatment programmes can improve treatment access and adherence. Community approaches shall also reduce the burden faced by health systems in trying to absorb the number of people newly put on treatment.
Another advantage of scaling up community-based service delivery is that communities can better reach and engage key affected populations. “Community-based approaches have demonstrated to improve the ability of populations at higher risk of HIV to access HIV services and to benefit from antiretroviral therapy and prevent new infections,” said Mr Barr.
Providing a perspective from Latin America, Dr Massimo Ghidinelli, Regional HIV Adviser at the Pan American Health Organization (PAHO) discussed some of the critical issues faced in that region. The need to optimize drug regimens, diagnosis and monitoring tools as well as lowering costs and improving treatment delivery systems were identified as major challenges.
According to UNAIDS, the new treatment approach could also reduce new HIV infections by up to one million annually if countries provide antiretroviral therapy to all people in need. “We cannot treat ourselves out of this epidemic,” said Dr Schwartländer. “But reaching all eligible with effective therapies will not only safe millions of lives, but significantly reduce the number of new infections through lowering the viral load in people living with HIV.”
External links
External links
Publications
Publications
Related

Feature Story
Call for increased commitment to meet the goal of diagnosing and treating one million people with multidrug-resistant tuberculosis between 2011 and 2015
23 March 2011
23 March 2011 23 March 2011A version of this story also appears at www.who.int.

Credit: WHO
To mark World TB Day, the World Health Organization (WHO), the Global Fund to Fight AIDS, Tuberculosis and Malaria and the Stop TB Partnership are calling on world leaders to step up their commitment and contributions to meet the goal of diagnosing and treating one million people with multidrug-resistant tuberculosis (MDR-TB) between 2011 and 2015.
WHO has released a report, Towards universal access to diagnosis and treatment of MDR-TB and XDR-TB by 2015, which presents progress in the MDR-TB response in the countries with the highest burden of drug-resistant TB. "Many countries have made progress, but despite the recent scale-up in efforts, the world needs to do much more to get care to all MDR-TB patients who need it," says Dr Margaret Chan, WHO Director-General. "We cannot allow MDR-TB to spread unchecked."
The risk of leaving multidrug-resistant tuberculosis untreated
Leaving MDR-TB untreated increases the risk of spread of drug resistant strains of TB. WHO estimates there will be more than 2 million new cases of MDR-TB between 2011 and 2015.
Treatment programmes
Programmes financed by the Global Fund and that follow WHO treatment standards are expected to diagnose and treat about 200 000 people for MDR-TB by 2015, a fourfold increase from those 50 000 patients who are currently undergoing treatment.
Many countries have made progress, but despite the recent scale-up in efforts, the world needs to do much more to get care to all MDR-TB patients who need it
Dr Margaret Chan, WHO Director-General
It is anticipated that the Global Fund will provide 84% of all international investments in TB in 2011. However, both domestic and international resources need to be scaled up to cope with MDR-TB if progress in the response to TB is to be maintained.
“MDR-TB is a threat to all countries as it is difficult and expensive to treat. Unless we make an extraordinary effort to tackle this problem our ability to finance and secure continued progress against TB in general will be threatened” says Professor Michel Kazatchkine, Executive Director of the Global Fund.
Time to step up commitments
According to Dr Jorge Sampaio, the UN Secretary-General's Special Envoy to Stop TB, "It is time for countries with rapidly growing economies and a heavy burden of MDR-TB to step up their commitment and financing for their own MDR-TB programmes. Several have the capacity to show new leadership on south-south cooperation and aid to neighbouring countries that are also affected."
Since 2009, the 23 countries most heavily affected by TB drug resistance have nearly doubled their budgets for MDR-TB. According to the Global Fund, from 2002 to 2010, they have financed TB programmes around the world that have provided treatment to 7.7 million people and saved the lives of 4.1 million.
"The Global Fund's success can be measured in the number of lives that have been saved through care provided by the TB programmes it finances," says Dr Lucica Ditiu, Executive Secretary of the Stop TB Partnership. "Every TB patient should have access to proper care...To reach a million people with effective care for MDR-TB over the next five years, we will need to work closely with all partners, especially with affected communities."
MDR-TB is a form of TB that fails to respond to standard first-line drugs. In 2009, WHO reported that 9.4 million people became ill with TB and 1.7 million died, including 380 000 people with HIV-associated TB. There were some 440 000 cases of MDR-TB and 150 000 deaths in 2008, the latest year for which estimates are available.
External links
Related

Feature Story
Health 8 group meet to discuss maximizing health outcomes with available resources and getting “more health for the money”
23 February 2011
23 February 2011 23 February 2011
Ms Helen Evans Interim Chief Executive Officer, Global Alliance for Vaccines and Immunisation (GAVI); Dr Michel Kazatchkine Executive Director, Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM); Ms Tamar Manuelyan Atinc Vice President, Human Development Network, World Bank; Dr Tachi Yamada President, Global Health Program, Bill & Melinda Gates Foundation; Dr Margaret Chan Director-General, World Health Organization (WHO); UNAIDS Executive Director Michel Sidibé; Mr Anthony Lake Executive Director, United Nations Children’s Fund (UNICEF); Mr Babatunde Osotimehin Executive Director, United Nations Population Fund (UNFPA).
The Health 8 group gathered at the UNAIDS Headquarters in Geneva on Wednesday 23 February to reflect and strategize on one of most pressing issues affecting the health of the world’s population—maximizing health outcomes with available resources.
The Geneva meeting, convened in this occasion by UNAIDS Executive Director Michel Sidibé, focused on how to get “more health for the money.” Participants held discussions under three main topics: the UN Secretary-General’s Global Strategy for women’s and children’s health, the role of multilateralism in the new economic order, and the provision of technical support for capacity building.
The Health 8 (H8) is an informal group of eight health-related organizations comprising WHO, UNICEF, UNFPA, UNAIDS, GFATM, GAVI, Bill & Melinda Gates Foundation, and the World Bank. It was created in mid-2007 to stimulate a global sense of urgency for reaching the health-related Millennium Development Goals and has focused on better ways to speed up efforts to bring lifesaving-health improvements to people worldwide.
Related

Feature Story
‘A better future’: New evidence shows triple antiretroviral drugs during pregnancy and breastfeeding can significantly reduce mother-to-child transmission of HIV
14 January 2011
14 January 2011 14 January 2011
Credit: UNAIDS/P. Virot
The Lancet Infectious Diseases today published evidence from a World Health Organization-led study. The study showed that giving pregnant women living with HIV a combination of three antiretroviral (ARV) drugs from the last trimester, through delivery and six months of breastfeeding can reduce the risk of their babies being infected with HIV by more than 40%.
The study, named Kesho Bora which means ‘a better future’ in Swahili, was conducted between June 2005 and August 2008 in five sites in Burkina Faso, Kenya and South Africa. The randomized controlled trial aimed to assess the efficacy and safety of triple antiretroviral treatment to reduce mother-to-child transmission of HIV. This was compared to the use of single-dose nevirapine and zidovudine stopped after delivery, as had been recommended by the World Health Organization (WHO) since 2004.
Triple antiretroviral treatment given to pregnant women with a CD4 immune cell count of 200-500 cells/mm3 starting in their last trimester reduced mother-to-child transmission by 43% and reduced the risk of infection during breast-feeding by more than half. It was also shown to be safe for both mother and baby.
The WHO’s Department of Reproductive Health and Research worked in partnership on the study with the French National Agency for Research on AIDS and Viral Hepatitis (ANRS), the US Centers for Disease Control and Prevention (CDC) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health.
Related

Feature Story
Affordable TB prevention a must for people living with HIV
01 December 2010
01 December 2010 01 December 2010
Tuberculosis (TB) is a leading cause of death among people with HIV and, in order to mitigate this threat, low-cost preventive therapy is essential. In new guidelines released today, the World Health Organization (WHO) sets out how such therapy can be accessed safely and effectively.
According to WHO, the anti-TB drug isoniazid has a dramatic positive impact and the guidelines, aimed at resource-constrained settings, promote the use of Isoniazid Preventive Therapy (IPT) as a simple and cost-effective method that stops TB bacteria becoming active. A quarter of the nearly two million AIDS-related deaths each year is associated with TB and in some communities up to 80% of people who test positive for tuberculosis are also living with HIV.
WHO is committed to increasing the use of IPT. Coverage is currently extremely low with only 0.2% of all people with HIV having had access to this therapy last year. Additionally, around the globe just one in 20 HIV-positive people has ever been screened for TB.
World AIDS Day reminds us that business as usual is unacceptable and HIV programmes need to significantly expand their efforts to address TB
Dr Gottfried Hirnschall, Director of WHO’s HIV Department
“World AIDS Day reminds us that business as usual is unacceptable and HIV programmes need to significantly expand their efforts to address TB,” said Dr Gottfried Hirnschall, Director of WHO’s HIV Department. “We need to fully implement the WHO Three I’s for HIV/TB strategy in collaboration with all partners”.
The Three I’s are: Isoniazid Preventive Therapy, Intensified TB screening and Infection control for TB. According to WHO, these measures should be delivered as part of comprehensive HIV services.
“In many countries HIV is a major driver of the TB epidemic. TB is preventable and curable and the new guidelines show how to break the chain that links TB and HIV leading to death,” said Dr Mario Raviglione, Director of WHO’s Stop TB Department. “All countries and communities need to implement the new guidelines and WHO can provide the necessary support to ensure that this can happen.”
To encourage access to IPT for the millions in need, the WHO guidelines, which are based on recent scientific evidence used to update 1998 policy, address some of the misconceptions seen to be partly responsible for the IPT’s low coverage. There is no scientific evidence, for example, to support concerns that the treatment causes drug resistance to isoniazid. Also, IPT can be started following simple clinical screening without the need for costly mandatory tests as had been feared.
There are several key recommendations in the new WHO guidelines:
-
All children and adults living with HIV, including those on antiretroviral treatment and pregnant women, should receive IPT.
-
IPT should be provided for 6 to 36 months, or as a life-long treatment in settings with high HIV and TB prevalence.
-
People living with HIV who may have TB symptoms should befurther screened for active TB or other conditions to enable them to access appropriate treatment.
Preventing people living with HIV from dying of tuberculosis is one of UNAIDS’ priority areas.

Feature Story
Next steps with 1% tenofovir microbicide gel
24 November 2010
24 November 2010 24 November 2010After nearly 20 years of research, the results of the CAPRISA 004 trial provided the first evidence that the use of a vaginal microbicide could provide a safe and effective way to prevent HIV infection in women.

Following results from a South African study (CAPRISA 004) showing that a vaginal microbicide gel containing the antiretroviral drug tenofovir was 39% effective in reducing a woman’s risk of becoming infected with HIV during sex, WHO and UNAIDS convened a meeting in August 2010, just a month following the announcement, to review the implications of the CAPRISA 004 results and determine the appropriate next steps.
The meeting participants agreed on the below priority actions for follow-up:
- Additional safety studies;
- Effectiveness trial in South Africa to confirm the CAPRISA 004 BAT 24 dosing regimen;
- Effectiveness and safety trial of simplified dosing and HIV testing schedules;
- Implementation study in South Africa; and,
- Treatment outcome and resistance study.
To find out more, read the executive summary of the meeting report , or download the full report.

Feature Story
WHO World health report: The road to universal coverage
22 November 2010
22 November 2010 22 November 2010
If countries are to guarantee a good quality of life and ensure socio-economic development for people then promoting and protecting health is crucial. Without greater emphasis on health systems financing, however, this goal will remain unattainable for the poor, says the World Health Organization’s (WHO) World Health Report 2010, launched today.
Subtitled Health systems financing: the path to universal coverage, the report provides a detailed analysis of how this can be achieved with the provision of timely access to high-quality, affordable health services.
The concept of universal coverage emerged from a commitment from WHO member states in 2005 to develop their health financing systems. As the report has it, in an era of “globalisation of diseases” and increasing demands for chronic care from, for example people living with HIV on long term antiretroviral treatment, universal coverage will be of paramount importance.
According to the World Health Report, the lack of universal coverage has consequences for the poor. In some countries, for instance, the proportion of births attended by a skilled worker can be as low as 10%. This figure is close to 100% for richer nations.
Attaining universal coverage is considered relatively straightforward in principle but difficult in practice, and among others these two key actions are highlighted in the report.
Raising sufficient resources for health
Firstly, countries must raise sufficient funds. For many lower-income nations this may prove impossible in the short-term and the international community will need to financially support their efforts. Such nations currently spend around $US 32 per capita on health. To provide universal coverage this should be raised to US$ 60 by 2015.
Recipient countries can also increase their own health funding by reprioritising their budgets. Few African countries, for example, spend the 15% of their government budget on health they committed to in the 2001 Abuja Declaration. In fact, 20 countries in the region who signed the commitment actually allocate less now than they did nine years ago; although several, including Tanzania and Liberia, have exceeded this goal.
Another example is Rwanda’s donation of US$ 1 million in this year’s replenishment round of the Global Fund to fight AIDS, Tuberculosis and Malaria and South Africa’s announcement earlier this year of a US$ 1.1 million domestic investment in the country’s AIDS response.
Investing for health must be shared responsibility between development partners and national government
Michel Sidibé, UNAIDS Executive Director.
“Investing for health must be shared responsibility between development partners and national government,” said Mr Michel Sidibé, UNAIDS Executive Director.
Innovative financing may also be explored. Increasing taxes on air tickets, foreign exchange transactions and tobacco could be used to augment health budgets. The report states that, for example, a 50% increase in tobacco excise taxes would generate $US 1.42 billion in additional funds in 22 low income countries for which data are available. In countries such as the Lao People’s Democratic Republic, Madagascar and Viet Nam, the extra revenue would represent a 10% increase or more in total health expenditure, and a more than 25% in crease in the government’s total health budget.
Promoting efficiency and eliminating waste
Finally, the report suggests that inefficiency and waste can be extremely damaging for healthcare systems. It is argued that some 20-40% of resources spent on health are wasted. A 5% saving in health expenditure can be made if unnecessary spending on medicines is reduced, they are more appropriately used and quality control is improved.
Other ways to increase efficiency include; getting the most out of technologies and health services; motivating health workers; reducing medical errors and eliminating corruption.
Related

Feature Story
400 000 deaths among people living with HIV due to TB in 2009
11 November 2010
11 November 2010 11 November 2010
The latest WHO Global Tuberculosis Control Report 2010, launched today, highlights the need to reinvigorate efforts to prevent deaths from tuberculosis (TB) in people living with HIV. In 2009 there were an estimated 1.1 million cases of TB disease in people living with HIV, resulting in 0.4 million deaths. Yet TB is mostly preventable and curable.
According to the report, access to HIV testing, prevention, treatment and care for TB patients continues to expand. At least 75% of TB patients knew their HIV status in 55 countries, including 11 African countries such as Burkina Faso, Cote d’Ivoire, Mozambique and Zambia.
There are other examples of good practice. Namibia has improved its monitoring and evaluation systems and has reported around 15 000 people living with HIV are on isoniazid preventive therapy (IPR) in 2009. This therapy can prevent and reduce active TB among people living with HIV.
UNAIDS and Cosponsors have set an ambitious target of halving TB deaths in people living with HIV by 2015. This report highlights the need for us to work together on bold actions to achieve this goal
Alasdair Reid, UNAIDS HIV/TB Adviser
"The findings in the Global Tuberculosis Control 2010 publication confirm that when WHO's best practices are put in place, and with the right amount of funding and commitments from governments, we can turn the tide on the TB epidemic," said Dr Mario Raviglione, Director of the WHO Stop TB Department.
However, globally only 26% of TB patients knew their HIV status in 2009. People living with HIV who know their HIV status can benefit from appropriate treatment. In 2009 only about 140,000 HIV-positive TB patients were treated with antiretroviral therapy, this is only about 40% of all people living with HIV co-infected with TB.
“UNAIDS and Cosponsors have set an ambitious target of halving TB deaths in people living with HIV by 2015. This report highlights the need for us to work together on bold actions to achieve this goal,” said Alasdair Reid, UNAIDS HIV/TB Adviser.
Related
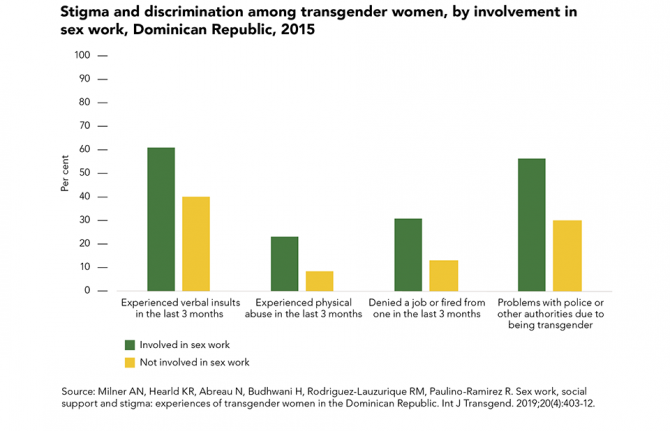
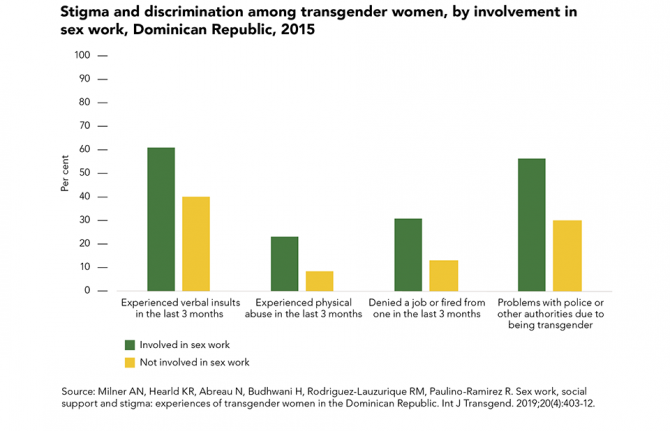 Transgender sex workers face frequent abuse
Transgender sex workers face frequent abuse
29 March 2022
 Many key populations avoid health services
Many key populations avoid health services

21 February 2022

Feature Story
Bridging the health gap in South Africa
09 November 2010
09 November 2010 09 November 2010A longer version of this article appeared in the November Bulletin of the World Health Organization

Credit: UNAIDS
When she was four years old, Thando* was taken to a public hospital in Johannesburg for HIV treatment. “I first saw her in 1998 with advanced disease and her CD4 count was less than 50,” says Ashraf Coovadia, a paediatrician at the Rahima Moosa Mother and Child Hospital. “In 1999 we managed to get her antiretrovirals (ARVs) through a research project.”
Prior to 2003, ARVs were not available in the public health system in South Africa, the country with the highest number of people with HIV in the world. While private patients could get access to the life-saving drugs and buy their survival, many patients in the public sector did not survive.
It is this stark public–private divide that the South African government hopes its proposed National Health Insurance (NHI) scheme will tackle by providing universal access to health care “based on need rather than ability to pay.”
The starting point for the NHI is to close the increasing gap between the rich and the poor
Dr Aaron Motsoaledi, Minister of Health of South Africa
Thando was lucky to get therapy in time and this “lovely teenager”, raised by her aunt, is the longest attending patient at the hospital’s paediatric clinic. “Prior to the rollout, we had a handful of children accessing ARVs, less than 5%. Now the majority who need it are on ARVs and doing well,” says Prof Coovadia.
Access to treatment for HIV has expanded dramatically in the past decade and, since the 1994 democratic elections, access to health services in general have improved for poorer South Africans. However, some believe that the standard of care in the public sector has been steadily deteriorating.
“South Africa has had difficulty post 1994 in grappling with the HIV epidemic—that was a real curveball,” says Helen Schneider, Chief Researcher at the University of Cape Town’s (UCT) Centre for Infectious Diseases Epidemiology and Research.
South Africa has had difficulty post 1994 in grappling with the HIV epidemic—that was a real curveball
Helen Schneider, Chief Researcher, Centre for Infectious Diseases Epidemiology and Research.
Health Minister Aaron Motsoaledi told the Bulletin: “the starting point for the NHI is to close the increasing gap between the rich and the poor. If I am sick, I get the best care. If people are unemployed, they can forget it.” Dr Motsoaledi describes the existing health-care system as “very expensive, destructive, unaffordable and not sustainable.”
In September 2010, the ruling African National Congress (ANC) released its current proposals for the NHI for wide consultation. According to Zweli Mkhize, chairman of the ANC’s health committee, the scheme, which aims to provide universal coverage for all South Africans, is expected to cost an extra R11 billion on top of the R117 billion in the government’s health budget for 2012. Taxation to pay for this compulsory medical insurance scheme is expected to start in 2012, with a plan to phase it in over 14 years.
A private economic consultancy, Econex, has published an extensive critique of the proposals, teasing out some of the implementation challenges, chief among them the enormous anticipated cost of the system as currently conceptualized.
And cost models produced for the Congress of South African Trade Unions, which strongly supports the introduction of NHI, suggest an additional funding requirement of around R189 billion, before administrative savings.
The NHI would also introduce new dimensions to the South African health financing system, notably the possibility of using public resources through strategic purchasing of services for the population. According to Di McIntyre, a professor from UCT’s Health Economics Unit, this would ensure that “everyone will be able to access health services on the basis of their need for care and not on the basis of their ability to pay.”
*Thando’s name has been changed.