Feature Story
UNICEF Executive Director launches innovative approach to prevent mother-to-child HIV transmission in Kenya
29 October 2010
29 October 2010 29 October 2010A version of this story has been published at unicef.org

Credit: UNICEF/NYHQ2010-1057/Susan Markisz
UNICEF Executive Director Anthony Lake joined the Government of Kenya and other partners on 29 October to role out an innovative approach to prevent the transmission of HIV from mothers to their babies (PMTCT). The initiative includes a combination of activities and supplies including a “Mother-Baby-Pack” of antiretroviral drugs and antibiotics, which women can easily administer at home.
The “Mother-Baby-Pack” is part of the government’s Maisha mother-to-child transmission free Zone Initiative. This pioneering programme is designed to help virtually eliminate mother-to-child-transmission of HIV and paediatric AIDS by 2013 in Nyanza and Rift Valley provinces, where about half of all Kenyan children with HIV live, and by 2015 in the entire country. Without treatment, around half of all babies born with HIV will die before their second birthday
Mr Lake commended the Kenyan government for its commitment to take ground-breaking steps to expand and strengthen the quality of PMTCT services. “Maisha means ‘Life’ in Kiswahili, and I can think of no better way to describe a programme with the potential to save so many lives,” he said. “The Maisha Initiative is a significant step forward towards our common goal of virtually eliminating mother to child transmission in Kenya.”
Maisha means ‘Life’ in Kiswahili, and I can think of no better way to describe a programme with the potential to save so many lives
Anthony Lake, UNICEF Executive Director
The roll-out in Kenya of the “Mother-Baby-Pack” marks the beginning of a phased implementation in four countries, including Cameroon, Lesotho and Zambia. It is scheduled to run until mid-2011. During this initial phase, UNICEF and its partners will closely monitor the acceptance of the pack by women, as well as the quality of supply and distribution.
The packs were developed by UNICEF in collaboration with the World Health Organization (WHO), UNITAID, and other partners. Health workers in antenatal clinics will distribute them to pregnant women living with HIV, but who do not yet need antiretroviral treatment for their own health. The initiative is designed to reach pregnant women who have tested positive for HIV, but who might not otherwise return to a clinic following their diagnosis.

Mother-Baby Packs arrive in Nairobi. They are then loaded onto a UNICEF truck for distribution to other parts of Kenya. Credit: UNICEF Kenya/2010/Joseph Munga
The initiative is supported financially by a number of partners including the US Government, UNICEF National Committees, the Clinton Health Access Initiative (CHAI) and the Mothers-to-Mothers (M2M) programme.
While adult HIV prevalence in Kenya has declined steadily, there are still some 22,000 new infections annually among infants through mother-to-child transmission. Overall, an estimated 1.4 million people are living with HIV in the country, including around 81,000 pregnant women.
Related
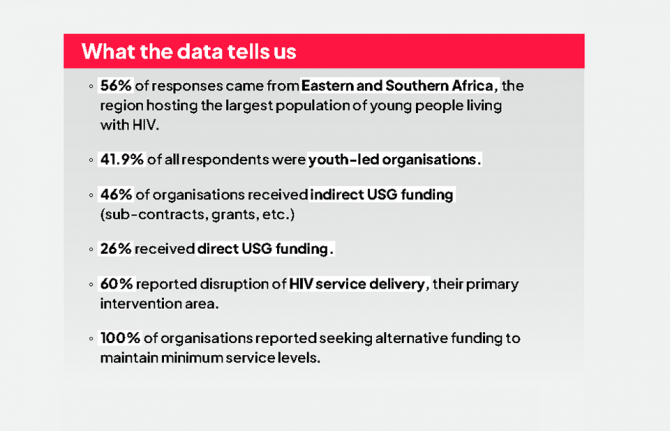
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025
 Impact of US funding cuts on HIV programmes in Kenya
Impact of US funding cuts on HIV programmes in Kenya

04 April 2025
 Impact of US funding cuts on HIV programmes in Kenya
Impact of US funding cuts on HIV programmes in Kenya

01 April 2025

Feature Story
Maternal deaths worldwide drop by a third
15 September 2010
15 September 2010 15 September 2010
The number of women dying due to complications during pregnancy and childbirth has decreased by 34% from an estimated 546 000 in 1990 to 358 000 in 2008, according to a new report, Trends in maternal mortality, released by the World Health Organization (WHO), the United Nations Children's Fund (UNICEF), the United Nations Population Fund (UNFPA) and the World Bank.
Despite this notable progress, the annual rate of decline is less than half of what is needed to achieve the Millennium Development Goal (MDG) target of reducing the maternal mortality ratio (the number of deaths per 100,000 live births) by 75% between 1990 and 2015. This will require an annual decline of 5.5%: the current average annual decline of just 2.3%.
"The global reduction in maternal death rates is encouraging news," says Dr Margaret Chan, the Director-General of WHO.”No woman should die due to inadequate access to family planning and to pregnancy and delivery care."
For nations with high HIV prevalence, AIDS has become a leading cause of death during pregnancy and after the birth. There is also some evidence that women living with HIV are at greater risk of maternal death. Overall, it was estimated that there were 42 000 deaths due to AIDS among pregnant women globally in 2008. About half of those are estimated to be maternal. The contribution of HIV was highest in sub-Saharan Africa where 9% of all maternal deaths were AIDS-related.
“Integrating HIV services with maternal and sexual and reproductive health services is imperative to stop mothers from dying and babies from being born with HIV,” said Mr Michel Sidibé, UNAIDS Executive Director. “The AIDS movement must be leveraged to achieve reductions in maternal and child mortality.
According to the report pregnant women die from four major causes: severe bleeding after childbirth, infections, hypertensive disorders, and unsafe abortion. Every day, about 1000 women died due to these complications in 2008, more than half in sub-Saharan Africa. The risk of a woman in a low-income country dying from a pregnancy- related cause during her lifetime is about 35 times greater than a woman living in a high-income country.
"To achieve our global goal of improving maternal health and to save women's lives we need to do more to reach those who are most at risk," says Anthony Lake, Executive Director of UNICEF. "That means reaching women in rural areas and poorer households, women from ethnic minorities and indigenous groups, and women living with HIV and in conflict zones."
The new estimates show that it is possible to prevent many more women dying. Countries need to invest in their health systems and in the quality of care.
"Every birth should be safe and every pregnancy wanted,” says Thoraya Ahmed Obaid, the Executive Director of UNFPA.The lack of maternal health care violates women's rights to life, health, equality, and non-discrimination.
UN agencies, donors and other partners have increasingly coordinated their assistance to countries, focusing on those with the greatest burden.
According to Tamar Manuelyan Atinc, Vice President for Human Development at the World Bank, “Given the weak state of health systems in many countries, we must work closely with governments, aid donors and agencies, and other partners to strengthen these systems.

Feature Story
WHO online consultation on global health sector strategy for HIV
06 August 2010
06 August 2010 06 August 2010
The World Health Organization (WHO) has launched a web-based consultation to seek input on the development of the WHO Global Health Sector Strategy for HIV/AIDS, 2011-2015.
The Sixty-third Session of the World Health Assembly adopted a resolution requesting that the World Health Organization (WHO) Director-General develop a WHO HIV/AIDS Strategy for 2011-2015, through a broad consultative process.
You are invited to provide your feedback on the consultation materials found on the WHO web site. These materials will be available in Arabic, Chinese, English, French, Russian and Spanish.
Comments should be submitted by 31 August using this online form. Where possible, please submit your comments in English to facilitate the synthesis of all inputs.
The 2011-2015 strategy will:
- Build on the achievements and experiences of the "3 by 5" initiative and the five strategic directions of the WHO HIV/AIDS Universal Access Plan 2006-2010;
- Take into consideration the broad global HIV, health and development architecture, including the UNAIDS Strategy (under development) and UNAIDS Outcome Framework, and existing commitments to achieving Universal Access and the Millennium Development Goals;
- Identify existing and agreed global targets to motivate countries to plan for bold HIV responses through to 2015;
- Provide guidance to countries on how to prioritize their HIV and broader health investments;
- Provide a framework for concerted WHO action at the global, regional and country levels and across all relevant WHO departments.
WHO works in partnership with a broad range of constituencies, including Member States, civil society, donor and development agencies, non-governmental organizations, multilateral agencies (including the UN family), scientific and technical institutions and networks, and the private sector. WHO is committed to a consultation process that involves all key stakeholders and constituencies in the development of the Global Health Sector Strategy for HIV/AIDS, 2011-2015.
Related

Feature Story
“Right for you!” Satellite puts young people centre stage at Vienna
22 July 2010
22 July 2010 22 July 2010 Right for you! satellite. Credit: UNAIDS/Anna Rauchenberger
Right for you! satellite. Credit: UNAIDS/Anna RauchenbergerThe thoughts and voices of young people took centre stage at the Vienna AIDS Conference yesterday as an innovative satellite session explored how they can best protect themselves from HIV. The session was organized by UNAIDS, UNESCO, UNFPA, UNICEF and WHO. It provided an interactive platform for youth from around the world to discuss sexual and reproductive health services and provision of comprehensive information including sexuality education, condom use and HIV counselling and testing.
Called ‘Right for You! Creating Game Changing Strategies for HIV and Young People’, the event was structured around the outcome of an online survey, promoted across varied social media platforms, such as Facebook, Twitter, AIDSspace and Conversations for a better world, to find out what young people really think about how to mount a meaningful and effective personal challenge to HIV. It was moderated by Ms Purnima Mane, United Nations Population Fund (UNFPA) Deputy Executive Director (Programme).
The session explored how to achieve three bold goals for young people:
- Ensure at least 80% of young people in and out school have comprehensive knowledge of HIV.
- Double young people’s use of condoms during their last sexual intercourse.
- Double young people’s use of HIV testing and counselling services.
‘Empowering Young People to Protect Themselves against HIV’, is one of the priority areas of the UNAIDS Outcome Framework 2009-2011. The aim is to reduce new HIV infections among young people by 30% by 2015.
The three goals discussed in yesterday’s satellite are far-reaching and ambitious in scope. They were highlighted in the UNAIDS business case on empowering young people. The business case is an advocacy tool which outlines why UNAIDS has prioritized young people and it recommends that the three results should be achieved in at least 9 of the 17 countries that have largest number of young people living with HIV by 2011, as well as in countries experiencing low and concentrated epidemics.
Those gathered at the event discussed how such results can be achieved and how the necessary good quality programmes can be scaled up at country level. An expert panel that included a youth facilitator, Ishita Chaudhry from India, Dr Doug Kirby, co-author of International Technical Guidance on Sexuality Education: An evidence informed approach for schools, teachers and health educators, Darlington Muyambwa, Programme Manager, SAYWHAT Programme, Zimbabwe , and Shaffiq Essajee, WHO, responded to feedback from participants who expressed their views or asked questions via the web forums.
Exploring ways of empowering young people to protect themselves against HIV is vitally important given latest estimates showing that 15-24 year olds account for some 40% of all adult HIV infections globally. In 2007, far fewer than half of young people around the world had accurate knowledge about HIV.
Additionally, in many parts of the world young people have inadequate access to sexual and reproductive health services and commodities like condoms. Socio-cultural norms can act as barriers to these essential services and commodities which discourage young people from learning about and discussing sex and sexuality and accessing the services. The session explored ways to address these challenges and empower young people to make informed decisions about this key aspect of their lives.
Right Hand Content

Feature Story
UNAIDS satellite explores paving the way towards virtual elimination of mother-to-child transmission of HIV
20 July 2010
20 July 2010 20 July 2010
From left: Ambassador Eric Goosby, United States Global AIDS Coordinator; Professor Michel D. Kazatchkine; Executive Director, The Global Fund to Fight AIDS, TB and Malaria; Anthony Lake, Executive Director of UNICEF; Michel Sidibé, Executive Director of UNAIDS; Hiroki Nakatami, Assistant Director General of WHO; at the UNAIDS PMTCT Satellite at the 18th International AIDS Conference in Vienna, Austria on 19 July 2010. Credit: UNAIDS/Heimo Aga
UNAIDS hosted a satellite at AIDS 2010 on preventing mother-to-child transmission of HIV 19 July. It was co-chaired by Antony Lake, Executive Director of UNICEF and Hiroki Nakatani, Assistant Director General of World Health Organization (WHO) and coordinated by Gottfried Hirnschall, Director of the HIV department (WHO). Opening remarks were delivered by Michel Sidibé, Executive Director of UNAIDS and Michel Kazatchkine, Executive Director of the Global Fund to Fight AIDS, TB and Malaria, and Ambassador Eric Goosby, United States Global AIDS Coordinator.
The call to eliminate mother-to-child transmission of HIV was first made by UNAIDS Executive Director Michel Sidibé and he has since been joined by leaders of nations, heads of multilateral, bilateral, regional and national bodies, presidents of foundations, members of civil society, and even captains of football teams in the FIFA 2010 World Cup.

From left: Professor Michel D. Kazatchkine; Executive Director, The Global Fund to Fight AIDS, TB and Malaria; Anthony Lake, Executive Director of UNICEF; Michel Sidibé, Executive Director of UNAIDS; Hiroki Nakatami, Assistant Director General of WHO; at the UNAIDS PMTCT Satellite at the 18th International AIDS Conference in Vienna, Austria on 19 July 2010. Credit: UNAIDS/Heimo Aga
Addressing the satellite, Mr Sidibé noted that many African countries like Botswana, Namibia and Swaziland are already leading the way towards virtual elimination if mother-to-child transmission, and many others are close behind.
This groundswell of support is lending hope to the possibility that transmission of HIV from mothers to children can be virtually eliminated in the highest-burden countries by 2015. At the same time, the WHO has issued new recommendations on the use of antiretroviral drugs for treating pregnant women and preventing HIV infection in infants and HIV and infant feeding. The main purpose of the new recommendations is to improve maternal and child survival by drastically reducing risk to around 5%, including in breastfeeding populations.
WHO, UNICEF, UNFPA and UNAIDS have developed a PMTCT strategic vision through the UNAIDS Outcome Framework for 2009-2011, aiming at defining joint commitment to support scale up of PMTCT of HIV services and integration with maternal, newborn and child and reproductive health services.
A long way to go
Despite this momentum, many nations have a long way to go. The majority of pregnant women in low- and middle-income countries do not know their HIV status. This knowledge has risen from 7% in 2004 to 21% in 2008. Also, the majority of HIV-positive pregnant women who need antiretrovirals (ARVs) for preventing transmission of the virus to their child. Only 45% of women in need of ARVs received it in 2008, although this is up from 10% in 2004.

UNAIDS PMTCT Satellite at the 18th International AIDS Conference in Vienna, Austria on 19 July 2010. Credit: UNAIDS/Heimo Aga
The quadrupling of the proportion of women receiving this important service is good news. But children continue to be left behind. Around 32% of infants born to HIV-positive mothers received antiretroviral for PMTCT in 2008, up from 20% in 2007 and 6% in 2004.
Update
Yesterday’s satellite provided an update on global commitments to virtual eliminate mother-to-child transmission of HIV. Participants highlighted key policy and operational considerations in implementing comprehensive PMTCT services integrated with maternal health and family planning services, including the WHO 2009 guidelines on ARV drugs for treating pregnant women and preventing HIV infection in infants which were reviewed by Nathan Shaffer of WHO.
To put theory into perspective country experience was shared by Mpolai Moteetee, the PMTCT focal point in Lesotho's Ministry of Health and Social Welfare Family Health Division who spoke of the experience of rapid scale-up of PMTCT services in Lesotho.
Marie Deschamps of GHESKIO (Groupe Haïtien d’étude du Sarcome de Kaposi et des Infectieuses Opportunistes) presented on the importance of integration of broad range of services of maternal health, family planning, PMTCT, and HIV treatment for maternal and child survival
Lilian Mworeko of ICW (International Community of Women with HIV/AIDS) Uganda shared her personal perspective as an activist and a person living with HIV.
Mother-Baby Pack
UNICEF, in collaboration with WHO and global partners, has developed an innovative simple, user-friendly and affordable packaging mechanism to deliver PMTCT preventive medications, the Mother-Baby Pack (MBP). Chewe Luo, a UNICEF Senior Advisor, presented the Pack which contains medicines for prophylaxis, ARVs and Co-trimoxazole, for the mother and for the infant in line with WHO 2010 PMTCT Guidelines. It also intends to help streamline procurement and supply management of PMTCT medicines.
The Global Fund has also declared preventing mother-to-child transmission (PMTCT) a priority and is currently assessing the possibility of reprogramming existing grants to accelerate scale-up in 20 countries (Angola, Botswana, Burundi, Cameroon, Côte d'Ivoire, the Democratic Republic of Congo, Ethiopia, Ghana, Kenya, Lesotho, Mozambique, Malawi, Namibia, Nigeria, South Africa, Swaziland, Tanzania, Uganda, Zambia and Zimbabwe).
Caroline Ryan of PEPFAR shared how their efforts will contribute towards virtual eiliminaiton. PEPFAR II has aligned its target to the UNGASS targets aiming to provide PMTCT services to 80% of all pregnant women living with HIV and exposed infants in their country programmes. All these commitments fall within the context of integrated programming for improved maternal and child health and survival coordinated with current US Global Health Initiative.
Closing remarks at the session were delivered by Antony Lake and Hiroki Nakatani.
Right Hand Content
Publications:
UNAIDS Outlook Report 2010 (pdf, 6 Mb)
UNAIDS Outcome Framework 2009-2011 (pdf, 388 Kb)

Feature Story
More than five million people receiving HIV treatment
19 July 2010
19 July 2010 19 July 2010World Health Organization advises earlier treatment among people with HIV
19 July 2010, Vienna - An estimated 5.2 million people in low-and middle-income countries were receiving life-saving HIV treatment at the end of 2009, according to the latest update from the World Health Organization (WHO).
WHO estimates that 1.2 million people started treatment in 2009, bringing the total number of people receiving treatment to 5.2 million, compared to 4 million at the end of 2008.
"This is the largest increase in people accessing treatment in a single year. It is an extremely encouraging development," says Dr Hiroki Nakatani, WHO Assistant Director-General for HIV, Tuberculosis, Malaria and Neglected Tropical Diseases.
At the XVIII International AIDS Conference, WHO is calling for earlier treatment for people with HIV. The objective is to begin HIV treatment before they become ill because of weakened immunity.
"Starting treatment earlier gives us an opportunity to enable people living with HIV to stay healthier and live longer,” says Dr Gottfried Hirnschall, WHO Director of HIV/AIDS.
Estimates developed through epidemiological modeling suggest that HIV-related mortality can be reduced by 20% between 2010 and 2015 if these guidelines for early treatment are broadly implemented.
Earlier treatment can prevent opportunistic infections including tuberculosis (TB), the number one killer of people with HIV. Deaths from TB can be reduced by as much as 90%, if people with both HIV and TB start treatment earlier.
The strength of a person's immune system is measured by CD4 cells. A healthy person has a CD4 count of 1000 - 1500 cells/mm3. WHO previously recommended starting HIV treatment when a person's CD4 count drops below 200 cells/mm3 but now advises starting HIV treatment at 350 cells/mm3 or below.
"In addition to saving lives, earlier treatment also has prevention benefits,” Dr Hirnschall says. “Because treatment reduces the level of virus in the body, it means HIV-positive people are less likely to pass the virus on to their partners."
WHO's treatment guidelines expand the number of people recommended for HIV treatment from an estimated 10 million to an estimated 15 million. The cost needed for HIV treatment in 2010 will be about US$ 9 billion, according to the Joint United Nations Programme on HIV/AIDS (UNAIDS).
"The investments we make today can not only save millions of lives but millions of dollars tomorrow,” said Dr Bernhard Schwartlander, Director, Evidence, Strategy and Results, UNAIDS. "People with weaker immune systems who come late for treatment require more complex and costly drugs and services than those who start treatment earlier and are healthier."
Since 2003 - which marked the launch of the historic “3 by 5” initiative to provide access to HIV treatment to 3 million people living in low- and middle-income countries by the end of 2005 - the number of people receiving HIV treatment has increased 12-fold.
At AIDS 2010, WHO is releasing the 2010 guidelines on “Antiretroviral treatment of HIV infection in adults and adolescents – public health approach”, which can be found at www.who.int/hiv.
Right Hand Content
Publications:
Fact sheet: New progress and guidance on HIV treatment
UNAIDS Outlook Report 2010 (pdf, 6 Mb)
UNAIDS Outcome Framework 2009-2011 (pdf, 388 Kb)
Related

Feature Story
WHO: HIV Programme highlights significant achievements towards universal access
02 June 2010
02 June 2010 02 June 2010
A recent report by the World Health Organization (WHO), HIV/AIDS Programme Highlights 2008-09, outlines major accomplishments of the agency in collaboration with countries and partners in promoting interventions to accelerate the progress towards universal access to HIV prevention, treatment, care and support services.
The report highlights, for example, that there has been a sharp increase in HIV testing in recent years thanks to WHO and UNAIDS’ approach, called the provider initiated testing and counseling (PITC), where healthcare providers specifically recommend an HIV test to patients attending health facilities in certain settings.
WHO now recommends earlier initiation of antiretroviral therapy (ART); delivery of safer, more effective antiretroviral drugs (ARVs); and their prolonged use for the prevention of mother-to-child HIV transmission.
More than half of the 93 reporting countries developing programmes have addressed their human resource shortages in AIDS care through WHO’s strategy of “task shifting”.
Due in part to WHO's efforts, the volume and scope of data to measure progress in scaling-up priority HIV interventions has also improved substantially since 2008. For the first time, WHO, UNICEF and UNAIDS jointly collected data from national programmes worldwide.
Despite funding gaps and implementation challenges, measurable progress was seen in the 2008-2009 biennium. While much work remains, the HIV/AIDS Programme Highlights shows that progress can be achieved, even in the most difficult environments.
WHO: HIV Programme highlights significant achieve
Related

Feature Story
Report calls for urgent scale-up of MSM strategies to prevent HIV in Asia Pacific
28 May 2010
28 May 2010 28 May 2010
A report on HIV among men who have sex with men and transgender people in the Asia-Pacific region has called for urgent scale-up of strategies to prevent the transmission of HIV, and to ensure greater access to treatment, care and support for those already in need.
Titled “Priority HIV and sexual health interventions in the health sector for men who have sex with men and transgender people in the Asia-Pacific Region”, the report was developed after a meeting held in Hong Kong in February 2009, organized by WHO Regional Office for the Western Pacific, UNDP, UNAIDS and the Department of Health of Hong Kong.
The context of the report is important as it comes at the back of two similar reports—by the Commission on AIDS in Asia and by the Commission on AIDS in the Pacific—recommending that the control of the HIV epidemic in the region would imply focusing on the most-at-risk populations, including men who have sex with men (MSM) and transgender persons (TG).
The HIV epidemic among MSM and TG is escalating globally and in Asia, MSM are disproportionately affected by it, with the odds of MSM having HIV infection being 18.7 times higher than that in the general population, the report states. The Asian Epidemic Model projects that unless effective prevention measures are intensified, by 2020, around 46% of new infections in Asia will be among MSM, up from 13% in 2008.
The report lays great emphasis on repealing laws by parliament or decisions by courts that violate the constitutional rights of MSM. Male-to-male sexual behaviour remains a criminal offence in 18 Asia-Pacific countries, contributing directly to the stigma associated with male-to-male sex and driving MSM underground, making it more difficult for prevention programmes to reach them.
To counter difficulties in motivating health workers and reducing stigma and discrimination, the report recommends sensitizing health workers to work with people living with HIV, including MSM and TG; and recruiting MSM and TG into healthcare positions.
The report recommends for the involvement of MSM in community responses to HIV through self-organization. MSM should be given supportive access to the full range of services in which staff are sensitized to their issues and needs. Peer support and counselling should be actively encouraged, it states.
National health sector strategies and plans should call for the engagement of civil society and MSM and TG community based organisations in strategic planning, programme development, implementation, monitoring and evaluation.
Finally, the report recommends involving WHO, United Nations Development Programme (UNDP), UNAIDS, United Nations Educational, Scientific and Cultural Organization (UNESCO) and the Asia Pacific Coalition on Male Sexual Health (APCOM) in all aspects of planning, implementing, monitoring and evaluating health sector responses to HIV at the global, regional, national and local levels.
Report calls for urgent scale-up of MSM strategie
Key populations:
Cosponsors:
World Health Organization
United Nations Development Programme
Feature stories:
Punitive laws limit access to HIV prevention and care services in Asia Pacific (21 May 2010)
HIV prevention hampered by homophobia
(13 January 2009)
External links:
Department of Health of Hong Kong
Commission on AIDS in the Pacific
Publications:
Priority HIV and sexual health interventions in the health sector for men who have sex with men and transgender people in the
Asia-Pacific Region (pdf, 1.84 Mb.)
Turning the tide: An open strategy for a response to AIDS in the Pacific. Report of the Commission on AIDS in the Pacific (pdf,
1.52 Mb.)
HIV and Men who have Sex with Men in Asia and the Pacific (pdf, 1.11 Mb.)

Feature Story
World Health Assembly to discuss International Health Regulations and MDG
17 May 2010
17 May 2010 17 May 2010
Credit: WHO/Jesse Hoffmann
The 63rd World Health Assembly, the gathering of the decision-making body of World Health Organization (WHO), opened in Geneva today. Health Ministers and officials from across the world will meet until 21 May 2010 to discuss the implementation of the International Health Regulations (IHR).
There are 194 countries across the globe, including all the member states of the World Health Organization (WHO) who are State Parties to the IHR, a binding, international legal instrument. The aim of these global rules is to help the international community prevent and respond to acute public health risks that have the potential to cross borders and threaten people worldwide.
The IHR, for example, require countries to report certain disease outbreaks and public health events to WHO and also to strengthen their existing capacities for public health surveillance and response.
This year’s World Health Assembly will also focus on monitoring the achievements of the health-related Millennium Development Goals. In the year 2000, 189 countries committed their nations to a new global partnership to reduce extreme poverty. They set out a series of targets to be reached by 2015. These have become known as the Millennium Development Goals (MDGs) and include halving extreme poverty, halting the spread of HIV and providing universal primary education.
The World Health Assembly is attended by delegations from all WHO member states yearly to focus on specific health agenda. Last year’s Assembly focused considerable attention on the widespread outbreak of influenza A (H1N1) and the most effective responses to the potential pandemic, including preparedness, access to vaccines and sharing of influenza viruses.
World Health Assembly to discuss International He
Cosponsors:
World Health Organization (WHO)
Feature stories:
UNAIDS calls for a virtual elimination of mother to child transmission of HIV by 2015 (21 May 2009)
Sixty-second World Health Assembly to be dominated by A(H1N1) (18 May 2009)
Publications:
Joint action for results: UNAIDS outcome framework, 2009 – 2011 (pdf, 931 Kb.)

Feature Story
TB partners meet in Viet Nam
04 May 2010
04 May 2010 04 May 2010 Preventing people living with HIV from dying of tuberculosis is one of the 10 priority areas outlined in the UNAIDS Outcome Framework for the period 2009-2011. Credit: UNAIDS/P.Virot
Preventing people living with HIV from dying of tuberculosis is one of the 10 priority areas outlined in the UNAIDS Outcome Framework for the period 2009-2011. Credit: UNAIDS/P.VirotThe 18th Stop TB Partnership Coordinating Board meeting is being held from 4 – 5 May 2010 in Hanoi, Viet Nam. The meeting will bring together UNAIDS and the Stop TB Partnership to strengthen their joint response to HIV/TB co-infection and to agree on a compact intended to halve TB deaths in people living with HIV by 2015.
‘One in four AIDS deaths is linked to tuberculosis. This compact represents an important milestone in ensuring that no person living with HIV dies of TB, a preventable and curable condition’ noted UNAIDS Deputy Director, Programme Paul De Lay
Every three minutes a person living with HIV dies of tuberculosis. Mortality rates have escalated (to an estimated 500,000 a year) over the past 10 years. The emergence of drug resistant strains of TB is a particularly lethal threat in populations with high rates of HIV infection.
Preventing people living with HIV from dying of tuberculosis is one of the 10 priority areas outlined in the UNAIDS Outcome Framework for the period 2009-2011. UNAIDS hopes to achieve this goal by ensuring an effective integrated delivery of services for HIV and tuberculosis as well as nutritional support in all settings.
Universal access and MDG targets for HIV and TB will be difficult, if not impossible, to achieve without greater attention to marginalized and vulnerable groups, such as prisoners, drug users, women, and migrants, and the strengthening of a human rights approach to ensure equitable access and risk-reduction.
A wide variety of participants are expected to attend the meeting, including Ministers of Health of Viet Nam, South Africa and Myanmar, the Regional Director of the World Health Organization Western Pacific Region as well as high-level representatives from UNAIDS, the Stop TB Partnership and the Global Fund to Fight AIDS, Tuberculosis and Malaria.
Discussions will range from an overview of the TB epidemic in Viet Nam and the Western Pacific Region to a review of progress in the development of new TB drugs, diagnostics and vaccines.
The Board meeting is also meant to be a follow-up from the Beijing Ministerial Meeting held in April 2009 where ministers from countries with high burden of multi-drug-resistant tuberculosis (MDR-TB) and extremely drug-resistant tuberculosis (XDR-TB) met to address the disease’s alarming threat. The 18th Stop TB Partnership Coordinating Board meeting will review the progress made by countries since Beijing and recommend further actions to overcome bottlenecks and accelerate action.
The Stop TB Partnership is a leading public-private global health partnership, established in 2001, with the aim of eliminating tuberculosis as a public health problem and, ultimately, to obtain a world free of TB. It comprises a network of more than 900 international organizations, countries, donors from the public and private sectors, governmental and nongovernmental organizations and individuals.
TB partners meet in Viet Nam
Cosponsors:
Partners:
Global Fund to Fight AIDS, Tuberculosis and Malaria
Feature stories:
Need for scale up in integrated TB and HIV screening to address linked epidemics (24 March 2009)
UNAIDS Executive Director meets with TB Programme Managers, TB civil society (26 March 2009)
External links:
Publications:
Interim Policy on Collaborative TB/HIV Activities (pdf, 285 Mb.)
Joint Action for Results: UNAIDS Outcome Framework (2009–2011) (pdf, 932 Kb.)
Tuberculosis: Guidelines for Workplace Control Activities (pdf, 223 Kb.)