Feature Story
Protecting drug users from becoming infected with HIV in Lithuania
19 February 2010
19 February 2010 19 February 2010
A WHO study, published in 2008, shows that opioid substitution therapy in low- and middle- income countries (as elsewhere) significantly reduces risky behaviour, improves the health of patients and helps them to re-integrate into society. Credit: WHO/Piotr Malecki
The pioneering Vilnius Centre for Addictive Disorders in Lithuania is the focus of the second Dispatch from the Field, a web series designed to highlight the World Health Organization’s work at country level.
The centre is considered a model of best practice in treating drug dependence. Heroin users are offered daily methadone and have access to a mobile needle-syringe exchange service called the ‘Blue bus.' Five days a week, social workers who run the bus go to places frequented by drug users and dispense both sterile equipment and advice about health and social services. Drug users are often marginalized and do not tend to seek health care.
Cooperating closely with the World Health Organization, the centre uses WHO guidelines and advocacy to strengthen its work.
Harm reduction interventions in Lithuania started early in the course of the HIV epidemic and are credited with helping to keep the country’s HIV prevalence relatively low. In 2008, Lithuania’s prevalence was less than one tenth that of some neighbouring countries, and the proportion of new cases of HIV caused by injecting drug use has been steadily decreasing.
Working with injecting drug users in Eastern Europe and central Asia is of paramount importance. Injecting drug use is the main mode of HIV transmission in the region, accounting for some 75-80 percent of all cases. A 2008 WHO study shows that opioid substitution therapy in low- and middle-income countries significantly reduces high risk behaviour, improves health and helps drug users re-integrate into society.
Three regional WHO-supported Harm Reduction Knowledge Hubs have been established, in which the Vilnius centre plays a pivotal role. The Hubs bring together the collective knowledge of regional and international experts and provide technical assistance, training and a forum for the exchange of ideas to widen and deepen the AIDS response.
This latest Dispatch from the Field features a photo essay on the Vilnius Centre for Addictive Disorders, an interview with its Director, Dr Emilis Subata and an article on the WHO Knowledge Hubs.
Protecting drug users from becoming infected with
Cosponsors:
World Health Organization
World Health Organization - HIV
Multimedia:
Photo essay on the Vilnius Centre for Addictive Disorders
Interview with Dr Emilis Subata, Director of the Vilnius Centre for Addictive Disorders
Article on the WHO Knowledge Hubs
Feature stories:
Advocating for HIV and Hepatitis C co-infection services for injecting drug users in India (15 September 2009)
Injecting drug users take central role in anti-stigma film (10 August 2009)
International Harm Reduction conference opens in Bangkok (20 April 2009)
OPINION: HIV and drugs: two epidemics - one combined strategy (20 April 2009)
UNODC and Iran sign agreements to reduce vulnerability of women and Afghan refugees to drugs and HIV (24 March 2009)
Injecting drug use and HIV: Interview with UNAIDS Team Leader, Prevention, Care and Support team (11 march 2009)
OPINION: Silence on harm reduction not an option (11 March 2009)
Related

Feature Story
WHO tool to integrate gender into AIDS programmes
15 January 2010
15 January 2010 15 January 2010
Half of all people living with HIV globally are now women and this figure rises to over 60 per cent in sub-Saharan Africa, where young women aged 15-24 can be several times more likely to be HIV-positive than their male counterparts. In order to offer women greater protection against the virus, the World Health Organization (WHO) has designed a hands-on tool to integrate gender into AIDS programmes in the health sector.
The impact of the epidemic on women is exacerbated by a number of factors women can face, including economic dependence on men which may limit their ability to refuse sex or negotiate condom use; their relatively low status, their vulnerability to violence, and lack of access to information and education about HIV. Such inequalities affect women’s experience of HIV, limiting their ability to cope once infected. In 2001 and 2006, the UN General Assembly Declarations of Commitment on AIDS spelled out the need for member states to address gender inequality as a major driver of the epidemic.
Field-tested in five countries (Belize, Honduras, Nicaragua, Sudan and Tanzania), the new tool helps those planning and implementing AIDS programmes in the health sector to better understand the links between gender inequalities and the virus. It raises awareness of how these inequalities influence women’s access to, uptake of, and experience with such programmes and services in the health sector.
I am a role model in the society and my male fellows will be astonished if I bring gender issues as a man. But because I am a role model, I will do it.
AIDS service provider in Lindi, Tanzania
The manual also gives practical suggestions to managers and health care providers, both public and private, on how to integrate gender into HIV programmes, rendering them more responsive to women’s needs. Informing national AIDS strategies, frameworks, guidelines and operational plans the tool can also be used by practitioners in their day to day work.
One AIDS service provider in Lindi, Tanzania believes that use of the tool in training him has been highly beneficial. “I am a role model in the society and my male fellows will be astonished if I bring gender issues as a man. But because I am a role model, I will do it.”
In addition to describing basic steps in gender-responsive programming, the manual suggests concrete actions to address key gender issues in four service delivery areas; HIV testing and counselling; prevention of mother-to-child transmission; treatment and care and, finally, home- based care and support for people living with HIV.
It also offers examples of gender-responsive interventions from the field, and resources such as counselling role plays for risk-reduction and HIV treatment adherence, and protocols for addressing the risk of violence against women as a result of HIV status disclosure. While citing specific examples, WHO suggests that the tool should be adapted to suit the specifics of each national and local environment.
The manual is seen as a work in progress which will be updated and revised as necessary for use by those who, according to WHO, are committed to gender equality and the health and well-being of all.
WHO tool to integrate gender into AIDS programmes
Cosponsors:
WHO
WHO: Gender, Women and Health
UNFPA
Partners:
The Global Coalition on Women and AIDS (GCWA)
Feature stories:
WHO report on the health of women: AIDS leading cause of death globally in women of reproductive age (09 November 2009)
Empowering women to protect themselves: Promoting the female condom in Zimbabwe (29 October 2009)
UNAIDS partners in new Clinton Global Initiative to address sexual violence against girls (25 September 2009)
Greater action needed to protect women’s inheritance and property rights in the face of HIV (13 March 2009)
New report shows Asian migrant women in the Arab states have heightened vulnerability to HIV (10 March 2009)
Commission on the Status of Women opens with call for action to achieve universal access and gender equality (02 March 2009)
Challenging violence against women a key task for newly launched Caribbean Coalition on Women, Girls and AIDS (06 March 2009)
Highlighting sexual violence on International Women’s Day (05 March 2009)
Publications:
Women and Health: Today’s Evidence, Tomorrow’s Agenda (pdf, 3.21 Mb.)
UNAIDS Outcome framework 2009-11 (pdf, 3.96 Mb.)
2008 Delegates Guide to Women and AIDS: All Women, All Rights (pdf, 506 Kb.)
An Analysis of the Gender Policies of the Three Major AIDS Financing Institutions: The Global Fund to Fight AIDS, Tuberculosis and Malaria, the World Bank and the President’s Emergency Plan for AIDS Relief (July 2008) (pdf, 166 Kb.)

Feature Story
Sexuality education an imperative for children and young people in a world affected by AIDS
10 December 2009
10 December 2009 10 December 2009
(From L to R) Mark Richmond, UNESCO’s Global Coordinator on HIV and AIDS, Dr Mariangela Batista Galvao Simao, Director, Brazil National STD/AIDS Programme, Michel Sidibé, UNAIDS Executive Director, Elizabeth Mataka, member of the Global Advisory Group on Sexuality Education and the UN Secretary-General’s Special Envoy for AIDS in Africa and Marijke Wijnroks, the AIDS ambassador for the Netherlands
Credit: UNAIDS/D.Bregnard
In many parts of the world, a combination of social taboos, unavailability of sound information, lack of resources and infrastructure make it difficult for children and young people to access sexuality education aimed at improving knowledge and reducing risk. This leaves many young people vulnerable to coercion, abuse, exploitation, unintended pregnancy and sexually transmitted infections, including HIV.
According to the UNAIDS 2008 Global Report on the AIDS Epidemic, only 40% of young people aged 15-24 had accurate knowledge about HIV and transmission. It should come as no surprise that, against this background of insufficient levels of basic knowledge, young people aged 15-24 account for 40% of all new HIV infections (UNAIDS 2009 AIDS Epidemic Update).
In response to this challenge, the voluntary and non-mandatory International Technical Guidance on Sexuality Education developed by UNESCO in partnership with UNAIDS, UNFPA, UNICEF and WHO seeks to assist education, health and other relevant authorities to develop and implement school-based sexuality education materials and programmes. The International Technical Guidance on Sexuality Education is based on a rigorous review of evidence on sexuality education programmes and is aimed at education and health sector decision-makers and professionals.
If we are to make an impact on children and young people before they become sexually active, comprehensive sexuality education must become part of the formal school curriculum, delivered by well trained and supported teachers.
Michel Sidibé, UNIADS Executive Director
Sexuality education can play a key role in improving knowledge and reducing sexual risk behaviours among young people. Equipped with better knowledge, information and skills, young people can be empowered to make informed decisions about sexual choices.
“If we are to make an impact on children and young people before they become sexually active, comprehensive sexuality education must become part of the formal school curriculum, delivered by well trained and supported teachers,” says Michel Sidibé, UNAIDS Executive Director. “Teachers remain trusted sources of knowledge and skills in all education systems and they are a highly valued resource in the education sector response to AIDS.”
The International Technical Guidance on Sexuality Education was co-authored by leading experts in the field of sexuality education and subjected to extensive review and comment by a global panel of experts and practitioners from civil society organizations, ministries of education and international agencies. Volume I of the International Technical Guidance on Sexuality Education focuses on the rationale for sexuality education and provides sound technical advice on characteristics of effective programmes. It is the outcome of a rigorous review of the literature on the impact of sexuality education and sexual behaviour, drawing upon 87 studies from around the world.
Numerous studies show that with the right information and skills, young people can change their behaviour to reduce the risk of acquiring HIV infection or passing it on to others.
Mark Richmond, UNESCO’s Global Coordinator on HIV and AIDS
A companion document (Volume II) focuses on the topics and learning objectives to be covered in a ‘basic minimum package’ on sexuality education for children and young people from 5 to 18+ years of age and includes a bibliography of useful resources. It was informed by a review of curricula from 12 countries, as well as other international models.
“Numerous studies show that with the right information and skills, young people can change their behaviour to reduce the risk of acquiring HIV infection or passing it on to others,” says Mark Richmond, UNESCO’s Global Coordinator on HIV and AIDS and the Director for the Division for the Coordination of UN Priorities in Education. “At a minimum, HIV and AIDS education needs to include information on the HIV virus and its modes of transmission. At some point, HIV and AIDS education must introduce sex and relationships education - simply because over 75% of all HIV infections occur through sexual transmission.”
The UN organizations called on policy-makers to listen to young people, families, teachers and other practitioners, and use the International Technical Guidance to make sexuality education an integral part of the national response to the HIV pandemic.
UNESCO and its partners including UNAIDS, UNFPA, UNICEF and WHO, as well as a wide range of other partners, will support governments in operationalising the International Technical Guidance on Sexuality Education at regional and country level. The two volumes of the International Technical Guidance will be published in all the six UN languages (Arabic, Chinese, English, French, Russian and Spanish) as well as Portuguese.
Sexuality education an imperative for children an
Key populations:
Cosponsors:
Feature stories:
Michel Sidibé calls for prevention revolution in opening address at UNAIDS’ governing body meeting (08 December 2009)
Preventing HIV through education in Latin America and Caribbean (31 July 2009)
New publication champions a strategic approach to HIV and education (15 June 2009)
Publications:
International Technical Guidance on Sexuality Education (Volume-I) (pdf, 2.84 Mb.)
International Technical Guidance on Sexuality Education (Volume-II) (pdf, 1.94 Mb.)

Feature Story
New HIV recommendations to improve health, reduce infections and save lives
30 November 2009
30 November 2009 30 November 2009
Credit: UNAIDS
On the eve of World AIDS Day, the World Health Organization (WHO) is releasing new recommendations on treatment, prevention and infant feeding in the context of HIV, based on the latest scientific evidence.
WHO now recommends earlier initiation of antiretroviral therapy (ART) for adults and adolescents, the delivery of more patient-friendly antiretroviral drugs (ARVs), and prolonged use of ARVs to reduce the risk of mother-to-child transmission of HIV. For the first time, WHO recommends that HIV-positive mothers or their infants take ARVs while breastfeeding to prevent HIV transmission.
"These new recommendations are based on the most up to date, available data," said Dr Hiroki Nakatani, Assistant Director General for HIV/AIDS, TB, Malaria and Neglected Tropical Diseases at the World Health Organization. "Their widespread adoption will enable many more people in high-burden areas to live longer and healthier lives."
An estimated 33.4 million people are living with HIV, and there are some 2.7 million new infections each year. Globally, AIDS is the leading cause of mortality among women of reproductive age.
New treatment recommendations
In 2006, WHO recommended that all patients start ART when their CD4 count (a measure of immune system strength) falls to 200 cells/mm3 or lower, at which point they typically show symptoms of HIV disease. Since then, studies and trials have clearly demonstrated that starting ART earlier reduces rates of death and disease. WHO is now recommending that ART be initiated at a higher CD4 threshold of 350 cells/mm3 for all HIV-positive patients, including pregnant women, regardless of symptoms.
WHO also recommends that countries phase out the use of Stavudine, or d4T, because of its long-term, irreversible side-effects. Stavudine is still widely used in first-line therapy in developing countries due to its low cost and widespread availability. Zidovudine (AZT) or Tenofovir (TDF) are recommended as less toxic and equally effective alternatives.
The 2009 recommendations outline an expanded role for laboratory monitoring to improve the quality of HIV treatment and care. They recommend greater access to CD4 testing and the use of viral load monitoring when necessary. However, access to ART must not be denied if these monitoring tests are not available.
Preventing mother-to-child transmission and improving child survival
In 2006, WHO recommended that ARVs be provided to HIV-positive pregnant women in the third trimester (beginning at 28 weeks) to prevent mother-to-child transmission of HIV. At the time, there was insufficient evidence on the protective effect of ARVs during breastfeeding. Since then, several clinical trials have shown the efficacy of ARVs in preventing transmission to the infant while breastfeeding. The 2009 recommendations promote the use of ARVs earlier in pregnancy, starting at 14 weeks and continuing through the end of the breastfeeding period.
WHO now recommends that breastfeeding continue until the infant is 12 months of age, provided the HIV-positive mother or baby is taking ARVs during that period. This will reduce the risk of HIV transmission and improve the infant's chance of survival.
"In the new recommendations, we are sending a clear message that breastfeeding is a good option for every baby, even those with HIV-positive mothers, when they have access to ARVs," said Daisy Mafubelu, WHO's Assistant Director General for Family and Community Health.
National health authorities are encouraged by WHO to identify the most appropriate infant feeding practice (either breastfeeding with ARVs or the use of infant formula) for their communities. The selected practice should then be promoted as the single standard of care.
Benefits and challenges
An earlier start to antiretroviral treatment boosts the immune system and reduces the risks of HIV-related death and disease. It also lowers the risk of HIV and TB transmission.
The new prevention of mother to child transmission (PMTCT) recommendations have the potential to reduce mother-to-child HIV transmission risk to 5% or lower. Combined with improved infant feeding practices, the recommendations can help to improve child survival.
The main challenge lies in increasing the availability of treatment in resource-limited countries. The expansion of ART and PMTCT services is currently hindered by weak infrastructure, limited human and financial resources, and poor integration of HIV-specific interventions within broader maternal and child health services.
The recommendations, if adopted, will result in a greater number of people needing treatment. The associated costs of earlier treatment may be offset by decreased hospital costs, increased productivity due to fewer sick days, fewer children orphaned by AIDS and a drop in HIV infections.
Another challenge lies in encouraging more people to receive voluntary HIV testing and counselling before they have symptoms. Currently, many HIV-positive people are waiting too long to seek treatment, usually when their CD4 count falls below 200 cells/mm3. However, the benefits of earlier treatment may also encourage more people to undergo HIV testing and counselling and learn their HIV status.
WHO, in collaboration with key partners, will provide technical support to countries to adapt, adopt and implement the revised guidelines. Implemented at a wide scale, WHO's new recommendations will improve the health of people living with HIV, reduce the number of new HIV infections and save lives.
New HIV recommendations to improve health, reduce
Cosponsors:
Publications:
Rapid advice: revised WHO principles and recommendations on infant feeding in the context of HIV(November 2009)
Rapid advice: antiretroviral therapy for HIV infection in adults and adolescents(November 2009)
Rapid advice: use of antiretroviral drugs for treating pregnant women and preventing HIV Infection in infants(November 2009)
Related

Feature Story
Eight-year trend shows new HIV infections down by 17%—most progress seen in sub-Saharan Africa
24 November 2009
24 November 2009 24 November 2009Efforts towards universal access to HIV prevention, treatment, care and support are bringing AIDS out of isolation
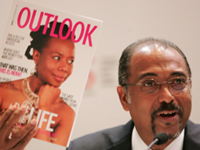
UNAIDS Executive Director Michel Sidibé launches double report in Shanghai, 24 November 2009.
Credit: UNAIDS
Geneva / Shanghai, 24 November 2009 – According to new data in the 2009 AIDS epidemic update, new HIV infections have been reduced by 17% over the past eight years. Since 2001, when the United Nations Declaration of Commitment on HIV/AIDS was signed, the number of new infections in sub-Saharan Africa is approximately 15% lower, which is about 400,000 fewer infections in 2008. In East Asia new HIV infections declined by nearly 25% and in South and South East Asia by 10% in the same time period. In Eastern Europe, after a dramatic increase in new infections among injecting drug users, the epidemic has leveled off considerably. However, in some countries there are signs that new HIV infections are rising again.

Credit: UNAIDS
The report, released today by the Joint United Nations Programme on HIV/AIDS (UNAIDS) and the World Health Organization (WHO), highlights that beyond the peak and natural course of the epidemic—HIV prevention programmes are making a difference.
“The good news is that we have evidence that the declines we are seeing are due, at least in part, to HIV prevention,” said Michel Sidibé, Executive Director of UNAIDS. “However, the findings also show that prevention programming is often off the mark and that if we do a better job of getting resources and programmes to where they will make most impact, quicker progress can be made and more lives saved.”
In this first double issue, the UNAIDS Outlook report further explores how “modes of transmission” studies are changing the approach of HIV prevention efforts. The new magazine-style report looks at new ideas and ways to use the data collected in the companion epidemiological report.
An estimated:
- 33.4 million [31.1 million–35.8 million] people are living with HIV worldwide
- 2.7 million [2.4 million–3.0 million] people were newly infected in 2008
- 2 million [1.7– 2.4 million] people died of AIDS related illness in 2008
Universal access to HIV prevention, treatment, care and support

photo caption. Credit:
Data from the AIDS Epidemic Update also show that at 33.4 million, [31.1 million–35.8 million] there are more people living with HIV than ever before as people are living longer due to the beneficial effects of antiretroviral therapy and population growth. However the number of AIDS-related deaths has declined by over 10% over the past five years as more people gained to access to the life saving treatment. UNAIDS and WHO estimate that since the availability of effective treatment in 1996, some 2.9 million lives have been saved.
"International and national investment in HIV treatment scale-up have yielded concrete and measurable results,” said Dr Margaret Chan, Director General of WHO. “We cannot let this momentum wane. Now is the time to redouble our efforts, and save many more lives."
Antiretroviral therapy has also made a significant impact in preventing new infections in children as more HIV- positive mothers gain access to treatment preventing them from transmitting the virus to their children. Around 200 000 new infections among children have been prevented since 2001.
In Botswana, where treatment coverage is 80%, AIDS-related deaths have fallen by over 50% over the past five years and the number of children newly orphaned is also coming down as parents are living longer.
AIDS out of isolation
One of the significant findings of the report is that the impact of the AIDS response is high where HIV prevention and treatment programmes have been integrated with other health and social welfare services. Early evidence shows that HIV may be a significant factor in maternal mortality. Research models using South African data estimate that about 50,000 maternal deaths were associated with HIV in 2008.
“AIDS isolation must end,” said Mr Sidibé. “Already research models are showing that HIV may have a significant impact on maternal mortality. Half of all maternal deaths in Botswana and South Africa are due to HIV. This tells us that we must work for a unified health approach bringing maternal and child health and HIV programmes as well as tuberculosis programmes together to work to achieve their common goal.”
The AIDS epidemic is evolving and HIV prevention programmes are not rapidly adjusting to the changes
The double report also shows that the face of the epidemic is changing and that prevention efforts are not keeping pace with this shift. For example the epidemic in Eastern Europe and Central Asia once characterized by injecting drug use is now spreading to the sexual partners of people who inject drugs. Similarly in parts of Asia an epidemic once characterized by transmission through sex work and injecting drug use is now increasingly affecting heterosexual couples.
Data show that few HIV prevention programmes exist for people over 25, married couples or people in stable relationships, widowers and divorcees. These are the same groups in which HIV prevalence has been found to be high in many sub-Saharan countries. For example in Swaziland people over the age of 25 accounted for more than two thirds of adult infections yet very few HIV prevention programmes are designed for older people.
Funding for HIV prevention has become the smallest percentage of the HIV budgets of many countries. For example in Swaziland, just 17% of the country’s total budget for AIDS was spent on prevention despite a national HIV prevalence rate of 26%. In Ghana, the prevention budget was cut in 2007 by 43% from 2005 levels.
Building capacity: new social networking site for global AIDS community
Building on the need to maximize results and to better connect the 33.4 million people living with HIV and the millions of people who are part of the AIDS response, UNAIDS has launched AIDSspace.org. This social networking site is open to the community and is free.
AIDSspace.org aims to expand informal and established networks to include more people interested in HIV to maximize resources for a stronger AIDS response. The premise behind AIDSspace is simple: if hundreds of millions of people can connect on some of the most popular social networking sites (e.g. Facebook, LinkedIn, MySpace, Twitter, YouTube) to connect, exchange ideas, post and share HIV-related content, they can do the same for HIV related content—including key policies, case studies, multimedia materials, conference posters, reports and other essential resources. Users can also find and post jobs and reviews on service providers on AIDSspace.org
Press conference launch of two publications, Shanghai, 24 November 2009.
Speakers from left) Ms Annemarie Hou, Director Communicaitons UNAIDS; Mr Michel Sidibé, Executive Director, UNAIDS; Dr Chen Zhu, Chinese Minister of Health; Dr Hiroki Nakatani, Assistant Director General, AIDS, TB, Malaria and Neglected Tropical Diseases, WHO; Ms Zhao Chunki, Social worker.
UNAIDS is an innovative joint venture of the United Nations, bringing together the efforts and resources of the UNAIDS Secretariat and ten UN system organizations in the AIDS response. The Secretariat headquarters is in Geneva, Switzerland—with staff on the ground in more than 80 countries. The Cosponsors include UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, ILO, UNESCO, WHO and the World Bank. Contributing to achieving global commitments to universal access to comprehensive interventions for HIV prevention, treatment, care and support is the number one priority for UNAIDS. Visit the UNAIDS website at www.unaids.org
The World Health Organization (WHO) is the directing and coordinating authority for health within the United Nations system. It is responsible for providing leadership on global health matters, shaping the health research agenda, setting norms and standards, articulating evidence-based policy options, providing technical support to countries and monitoring and assessing health trends. For more information, please visit www.who.int
AIDSspace.org is an online community for connecting people, sharing knowledge, and accessing services for the 33.4 million people living with HIV and the millions who are part of the response. Sign up today at www.aidsspace.org
Eight-year trend shows new HIV infections down by
Cosponsors:
Press centre:
Download printable PDF (pdf)
Multimedia from press conference launches in Shanghai and Geneva (24 November 2009)
Feature stories:
UNAIDS Outlook 2010: Fresh perspective on the AIDS epidemic and response (24 November 2009)
Contact:
Sophie Barton-Knott
Tel: +41 22 791 1697
Email: bartonknotts@unaids.org
Publications:
2009 AIDS Epidemic Update (pdf, 3 mb)
Corrigendum to version downloaded before 25 November 14:00
UNAIDS Outlook 2010 (pdf, 4 mb)
Related

Feature Story
WHO report on the health of women: AIDS leading cause of death globally in women of reproductive age
09 November 2009
09 November 2009 09 November 2009
In a landmark report on the health of women and girls across the globe, the World Health Organization (WHO) states that AIDS-related illness is the leading cause of death and disease among women of reproductive age in low and middle income countries, particularly in Africa. Also, globally, unsafe sex is the single leading risk factor contributing to deaths among women of reproductive age. These findings support the contention in Women and Health: Today’s Evidence, Tomorrow’s Agenda that in a multiplicity of areas female health is neglected and must now be considered an urgent priority
The report maintains that women and girls are especially vulnerable to HIV infection due to a variety of biological and social factors. These include low socio-economic status that can limit choices and lead to high risk behaviours and norms and laws that subjugate women and which discourage them from seeking and obtaining the information they need to keep themselves safe. For example, globally only 38% of young women are able to describe the main ways to avoid infection and they are less likely to know that condoms can protect against HIV than young men. Data from 16 countries in sub-Saharan Africa from 2001-2007 also show that HIV prevalence is generally higher among adolescent girls aged 15-19 than their male counterparts. A significant cause of this is young girls partnering with older men who are more sexually experienced and more likely to be infected.
Violence against women
Violence against women is also a major cause of their increased vulnerability to HIV. It can make it difficult or impossible for them to control their sexual lives, abstain from sex or get their partners to use condoms. Violence, or the threat of it, can also result in women avoiding HIV prevention, treatment, care and support services.
We know that there is a strong relationship between violence against women and HIV. We need to help young people develop the skills for mutual consent in sex and marriage and put an end to violence and sexual coercion. This is key to preventing HIV and to achieving gender equality in all aspects of life.
Michel Sidibe, Executive Director of UNAIDS
For UNAIDS, this is a major area of concern and its Outcome Framework 2009-11 has stopping violence against women and girls as one of nine priority areas. According to Michel Sidibe, Executive Director of UNAIDS, “‘We know that there is a strong relationship between violence against women and HIV. We need to help young people develop the skills for mutual consent in sex and marriage and put an end to violence and sexual coercion. This is key to preventing HIV and to achieving gender equality in all aspects of life.”
Gender inequalities
Women and Health has an extremely broad scope and addresses a range of women’s health issues. The factors that come into play to increase women’s vulnerability to AIDS are also shown to profoundly affect women and girls’ general health and well-being. As the report contends, gender inequalities in the allocation of resources such as education, income, health care, nutrition and having a political voice are very much associated with poor health and reduced well-being.
“Despite considerable progress over the past two decades, societies are still failing women at key moments in their lives,” says Dr Margaret Chan, WHO Director-General, in the foreword to Women and Health. “These failures are most acute in poor countries, and among the poorest women in all countries. Not everyone has benefited equally from recent progress and too many girls and women are still unable to reach their full potential because of persistent health, social and gender inequalities and health system inadequacies.”
Key stages relevant for health: early childhood, adolescence, adulthood and older age
The report explores the lives of women and girls through key stages relevant for health: early childhood, adolescence, adulthood and older age, and shows that women face “widespread and persistent inequities” during each of these stages. It not only highlights women’s health needs- and how they are not being currently met in terms of HIV and other areas- but also the valuable contribution that they make to the health sector and society in general.
By using today’s evidence, sharing what is currently known about the health of women from all regions and throughout their lives, the report attempts to set out tomorrow’s agenda, a key element of which is championing reforms to enable women to not only be seen in their sexual and reproductive capacity, but to become active agents in health-care provision, playing a central role in the design, management and delivery of health services.
Women and Health draws attention to four areas where policy action could make a real difference to women’s health: building strong leadership and a coherent institutional response coalescing around a clear agenda; making health systems work for women; leveraging changes in public policy to encourage fundamental social change (through, for instance, targeted action to help girls enrol in school); and finally, building the knowledge base and monitoring progress.
WHO hopes that by reviewing the available data and charting a cogent way forward that the health of women and girls, and society as a whole, can be ameliorated. As the report has it, “Improve women’s health, improve the world.”
WHO report on the health of women: AIDS leading c
Key populations:
Cosponsors:
Partners:
The Global Coalition on Women and AIDS (GCWA)
Press centre:
WHO calls for action beyond the health sector to improve the health of girls and women (09 November 2009)
Feature stories:
Empowering women to protect themselves: Promoting the female condom in Zimbabwe (29 October 2009)
UNAIDS partners in new Clinton Global Initiative to address sexual violence against girls (25 September 2009)
New report shows Asian migrant women in the Arab states have heightened vulnerability to HIV (10 March 2009)
Commission on the Status of Women opens with call for action to achieve universal access and gender equality (02 March 2009)
Challenging violence against women a key task for newly launched Caribbean Coalition on Women, Girls and AIDS (06 March 2009)
Highlighting sexual violence on International Women’s Day (05 March 2009)
Publications:
Women and Health: Today’s Evidence, Tomorrow’s Agenda
UNAIDS Outcome framework 2009-11 (pdf, 396 Kb.)
2008 Delegates Guide to Women and AIDS: All Women, All Rights (pdf, 506 Kb.)
An Analysis of the Gender Policies of the Three Major AIDS Financing Institutions: The Global Fund to Fight AIDS, Tuberculosis and Malaria, the World Bank and the President’s Emergency Plan for AIDS Relief (pdf, 150 Kb.)

Feature Story
Antiretroviral treatment for prevention
06 November 2009
06 November 2009 06 November 2009People living with HIV who are following an effective antiretroviral therapy regimen can achieve undetectable viral loads – the amount of virus in a body fluid such s blood, semen or vaginal secretions – at certain stages of their treatment. Research suggests that when the viral load is undetectable in blood the risk of HIV transmission is significantly reduced. However, antiretroviral therapy for prevention has not proven to completely eliminate the risk of transmitting the virus.
To explore the issue WHO earlier this week convened a meeting to review the scientific data available on the use of ART for prevention and also explored the implications of this approach for individuals and communities as well as take into consideration human rights and ethical and public health implications.
Participating in the meeting, UNAIDS Deputy Executive Director, Dr Paul De Lay, provided closing reflections. Dr De Lay said the meeting had raised the hard fact that many people living with HIV - including many who need treatment today - are unable to access HIV testing and counseling and to initiate timely treatment, as a result of a range of social, cultural and economic barriers.
These are exciting and challenging times. The diverse perspectives heard in this meeting reflect the best of the AIDS response, and continuing this dialogue - this committed questioning and the research agenda coming from this meeting - will undoubtedly lead to more lives saved and fewer new infections.
Dr Paul De Lay, UNAIDS Deputy Executive Director
Dr De Lay congratulated the participants in their effort to identifying scientifically sound and innovative ways to accelerate progress toward universal access to HIV prevention, treatment, care and support, and maximizing the effects of ART both for extending full and productive life for people with HIV, and also for primary prevention.
"These are exciting and challenging times. The diverse perspectives heard in this meeting reflect the best of the AIDS response, and continuing this dialogue - this committed questioning and the research agenda coming from this meeting - will undoubtedly lead to more lives saved and fewer new infections" continued Dr De Lay.
UNAIDS strongly recommend a comprehensive approach to HIV prevention that plans and delivers an evidence informed and human rights based combination of programmes and policies, tailored to meet the needs of those most at risk, and including practical programmes to reduce underlying causes of vulnerability, such as gender inequality and HIV related stigma and discrimination.
Antiretroviral therapy will play several roles in combination prevention strategies, along with other key strategies including, but not limited to, social and behavioral change communication to delay sexual debut, promote mutual fidelity and reduction of the number of sexual partners, promote safer sex including correct and consistent male and female condom use, harm reduction programmes for people who use drugs, prevention of vertical transmission, and other biomedical, behavioural and structural prevention programmes.
The WHO hosted antiretroviral treatment (ART) for Prevention was held in Geneva from the 2 to the 4 of November, 2009.
Antiretroviral treatment for prevention
Cosponsors:
Press centre:
Antiretroviral therapy and sexual transmission of HIV
Publications:
Intensifying HIV Prevention: UNAIDS Policy Position Paper (2005) (pdf, 3.80 Mb.)
Practical Guidelines for Intensifying HIV Prevention (2007) (pdf, 1.67 Mb.)

Feature Story
Governments and civil society expand access to HIV testing and counselling
30 September 2009
30 September 2009 30 September 2009This story has also been published at www.who.int/hiv

Photo credit: WHO
A brightly coloured van known as the ‘Tutu Tester’ has become a familiar sight in Cape Town, South Africa, as part of an accelerating drive to persuade people to know their HIV status. More than 10 000 people have been tested and counselled since May 2008 when the mobile clinic from the Desmond Tutu HIV Foundation took to the road.
It is one of many initiatives in sub-Saharan Africa designed to dispel the stigma and fear long associated with AIDS through imaginative campaigns ranging from sex worker advice at truck stops to peer counselling in mining areas to national testing weeks spearheaded by celebrities. The campaigns are part of wider national and international efforts to expand the number of people receiving testing and counselling—which is often referred to as ‘the gateway to HIV prevention, treatment and care’ because it is a precondition for timely access to all three, including antiretroviral therapy which cuts mortality rates.
Ninety percent of low- and middle-income countries last year reported that they have national HIV testing and counselling polices, up from 70% in 2007, according to the 2009 Towards universal access progress report, published by WHO, UNICEF and UNAIDS. Countries hardest hit by the pandemic—Botswana, Kenya, Lesotho, Malawi, Namibia, Rwanda, South Africa, Swaziland, Tanzania and Uganda—are testing and counselling pregnant mothers as the basis for prevention of mother-to-child transmission (PMTCT) to cut the number of infants born with HIV, and to help HIV-negative pregnant women stay negative.
There is encouraging evidence that more countries are adhering to WHO-UNAIDS guidance on provider-initiated testing and counselling in health facilities. This recommends HIV testing and counselling as part of the standard care to all persons with symptoms or medical conditions that could indicate HIV infection, to infants born to HIV-positive women, and in generalized epidemics to all persons attending health facilities. The guidelines are key to facilitating early diagnosis in countries which are struggling with a dual HIV-TB epidemic.
The number of health centres providing HIV testing and counselling is on the increase. In 15 reporting nations in East, South and South-East Asia, the number of such facilities rose from 13 000 to 15 000 between 2007 and 2008; in reporting Latin American and Caribbean countries it doubled, while sub-Saharan Africa boasted a 50% increase.
Some countries have made more progress than others. Ethiopia increased its number of facilities from 1005 to 1469 and reported that 4.5 million people received testing and counselling in 2008, up from 1.9 million in 2007. At the other end of the scale, less than 10% of health centres in Nigeria and the Democratic Republic of Congo had testing and counselling facilities.
Cameroon adopted provider-initiated testing and counselling in 2007. This was part of the government commitment to increase the number of people on treatment, up from 600 in 2001 to 60 000 in November 2008, according to WHO’s National Programme Officer for HIV/AIDS in Cameroon, Etienne Kembou. Although much remains to be done to train health professionals to implement the government model at local level, Kembou says about 85% of pregnant women at health facilities agree to be tested, as do growing numbers of men. “AIDS is not stigmatised like it was in the 1990s and many people who are HIV-positive are open about it,” Kembou says, adding that the annual national testing week and peer education projects aimed at 15–25 year-olds have helped enormously.
Uganda and Kenya have expanded coverage through home-based testing and counselling, whereby trained counsellors go from door to door. The advantage is that couples can be counselled together in a familiar environment without the stigma of going into a government facility. As a result, there are fewer disclosure problems which may arise with the male or female partner testing separately. It means that undiagnosed children with the virus can access HIV services and that high-risk areas such as the Kibera slum near Nairobi can be targeted.
In nations like Botswana and Swaziland, the government drive to scale up male circumcision for HIV prevention has led to an upsurge in testing and counselling among males, an often underserved group, as a precondition for the surgical intervention. WHO’s country representative in Botswana, Eugene Nyarko, says intensified prevention campaigns targeting youth are bearing fruit. “Across the board there is an increase in testing because young people know they can benefit from interventions if they know their status.”
In South Africa, which has the highest number of people in the world living with HIV, a national population-based survey in 2008 by the Human Sciences Research Council showed that 50% of respondents over 15 years of age said they had received an HIV test, compared to 20% in 2002. Between 2005 and 2008, the percentage of women and men who reported having an HIV test in the past 12 months more than doubled.
Civil society groups in South Africa, like the Treatment Action Campaign, have mounted high profile ‘Get Tested’ campaigns. There are many local initiatives backed by foreign donor funding and the government, and the message is getting through.
Sweetness Mzoli, runs an organisation called Kwakhanya (‘Light’) which helps care for 300 beneficiaries in Khayelitsha, a poor suburb of Cape Town with high HIV prevalence. She tours minibus taxi ranks trying to persuade men to be tested and counselled and notes there is far less resistance than even a year ago. “It’s coming right. There’s a lot of men out there who want to talk about their status and who want to know their status,” she comments.
The ‘Tutu Tester’ is also a regular visitor to Khayelitsha’s taxi ranks, as well as to shopping malls and other crowded areas. The testing and counselling process is efficient, thorough and friendly. Clients can avoid lengthy queues at public health facilities, while knowing they will receive high quality, confidential service.
“When you make it quick and efficient, people are willing to undergo testing,” says project coordinator Nienke van Schaik. The mobile clinic now offers a package, including testing for hypertension and diabetes “to make it less scary,” she says. “We literally just pitch up. People see us and run off and fetch their partners and family members. People are willing to test.”
Governments and civil society expand access to HI
Cosponsors:
World Health Organization (WHO)
United Nations Children’s Fund (UNICEF)
Publications:
Towards Universal Access: Scaling Up Priority HIV/AIDS Interventions in the Health Sector (pdf, 3 Mb.)
UNAIDS Outcome Framework 2009-2011 (pdf, 388 Kb.)
Related

Feature Story
More infants protected from HIV as access to antiretroviral drugs to prevent mother-to-child transmission increases
30 September 2009
30 September 2009 30 September 2009This story has also been published at www.who.int/hiv

Credit: WHO/James Oatway 2009
Despair is giving way to cautious optimism even in the most HIV-affected African nations as antiretroviral drugs become more widely available to stop HIV-positive women from infecting their unborn child or infant, thus edging closer to United Nations targets for an HIV-free generation of children.
The prevention of mother-to-child transmission (PMTCT) is one of the most powerful tools in HIV prevention and has huge potential to improve both maternal and child health. Yet despite recent progress much work remains.
In 2008, 45% of pregnant women in low- and middle-income countries received antiretrovirals to prevent HIV transmission to their child, up from 35% in 2007 and 10% in 2004, according to the 2009 Towards universal access progress report, published by WHO, UNICEF and UNAIDS. In Eastern and Southern African nations, which have the highest rates of infection, coverage jumped to 58% in 2008 from 46% in 2007, thanks to increased national commitment and focused international support.
One important reason is that HIV testing and counselling among pregnant women is increasing with the expansion of provider-initiated approaches in health-care settings. In 2008, 21% of pregnant women giving birth in low- and middle-income countries received an HIV test, up from 15% in 2007. In sub-Saharan Africa, the corresponding percentage rose from 17% to 28%, with particularly high rates of increase in countries in Eastern and Southern Africa. This was partly due to an increase in antenatal facilities providing PMTCT services and attracting high first-visit turnouts by pregnant women.
Globally, AIDS is the leading cause of mortality among women of reproductive age. In 2008, an estimated 1.4 million pregnant women living with HIV gave birth, 91% of them in sub-Saharan Africa, according to the report. One third of children living with the virus die before the age of one year and almost half by the second year.
In 2008, 70 low- and middle-income countries had established a national scale-up plan with population-based targets to prevent mother-to-child transmission of HIV, up from 34 countries in 2005. 54 countries had plans to scale up paediatric HIV services in 2008, compared to 19 countries in 2005. An estimated 32% of the infants born to HIV-infected mothers in 2008 were reached with antiretrovirals, more than five times as many as in 2004.
UN recommendations on PMTCT are based on a four-pronged approach: primary prevention of HIV infection among women of childbearing age; preventing unintended pregnancies among women living with HIV; preventing HIV transmission from women living with HIV to their infants, and providing appropriate treatment, care and support to mothers living with HIV and their children and families.
The UN General Assembly has set a target for 80% of pregnant women and their children to have access to essential prevention, treatment and care by 2010 to reduce the proportion of infants with HIV by 50%. This would entail at least 500 000 additional pregnant women accessing PMTCT services in order to meet this target. Given that PMTCT represents the interface between HIV and maternal and child health services, this would have a positive impact on the health of women and children in general. Achieving the target remains a formidable challenge, but more and more countries are making strides in the right direction.
Botswana, long regarded as sub-Saharan Africa’s flagship in prevention, treatment and care, has easily surpassed the target, with an estimated 95% of HIV-positive pregnant women and their newborns receiving testing, counselling and antiretrovirals. PMTCT has long been one of the pillars of national prevention programmes, according to WHO country representative Eugene Nyarko. “Government commitment and responsibility has been key,” he says.
Huge progress has been made in Swaziland, which has the world’s highest HIV prevalence. More than 90% of pregnant women in public health facilities now receive counselling and testing, and most of those testing positive are given antiretrovirals, according to Derek von Wissel, director of Swaziland’s National Emergency Response Committee on HIV/AIDS. “The availability of treatment is a huge positive element. People are not as fearful of testing since they know that HIV is no longer a death sentence and that there are remedies.” Swaziland has cut its mother-to-child HIV transmission rate from a peak of more than 30% to around 20%, and the goal is to reduce it to 5% by 2014, says von Wissel. “In Botswana, the paediatric programme is slowing down because fewer and fewer infants are being infected with HIV. We will hopefully go in that direction as well,’’ he says.
Equally significantly, more countries are following WHO recommendations to use a combination of two or three antiretroviral drugs to prevent vertical transmission from mother to child. In 2007, 49% of women receiving antiretrovirals were given a single-dose regimen of nevirapine. By 2008, this had fallen to about 31%, with more women receiving the more efficacious combination of several antiretrovirals.
A survey of babies tested for HIV during routine immunization in South Africa’s KwaZulu-Natal province showed the six-week vertical HIV transmission rate was 7% in 2008/2009 compared to 20.8% in 2004/2005. The dramatic reduction was largely due to an increase in testing, counselling and treatment and the switch to a combination of more than one antiretroviral drug.
“These data demonstrate that effective antiretroviral interventions can be delivered at scale and transmission rates can be dramatically reduced,” according to the Towards universal access progress report. “From where we were five years ago, there has been a tremendous increase in coverage,” comments Hoosen Coovadia, one of the South Africa’s top professors of paediatrics and PMTCT scientists. But he says capacity constraints at local level remain a challenge, and that health authorities should do more to use PMTCT as a catalyst to widen reproductive health services and involve male partners.
Progress in general in Western and Central Africa was held back by low coverage levels in Nigeria and the Democratic Republic of Congo which bear the heaviest HIV burden in the region. Nigeria alone accounts for 30% of the global gap in the UN’s target of reaching 80% of women by 2010.
In North Africa and the Middle East, less than 1% of pregnant women living with HIV received an antiretroviral regimen to stop HIV transmission to their child. In East, South and South-East Asia the figure was 25%. Coverage in Latin America increased from 47% in 2007 to 54% in 2008, and in the Caribbean from 29% to 52%. In Europe and Central Asia, coverage jumped from 74% in 2007 to 94% in 2008.
Even in countries with strong PMTCT programmes, there is no room for complacency. Thailand, for instance, has cut mother-to-child transmission rates to less than 5%, according to Siripon Kanshana, Deputy Permanent Secretary in the Ministry of Public Health. But she says there is a need for further capacity building and more training of medical personnel—nurses in particular—in testing and counselling and in monitoring side effects of antiretrovirals and potential drug resistance. “The Ministry of Health has the commitment. But the government still needs advocacy from UN agencies to help strengthen our health care systems to cope.”
More infants protected from HIV as access to anti
Cosponsors:
World Health Organization (WHO)
United Nations Children’s Fund (UNICEF)
Press centre:
More than four million HIV-positive people now receiving life-saving treatment (30 September 2008) (pdf, 40 kb.)
Feature stories:
Evidence shows new drug combination dramatically reduces mother-to child transmission of HIV during breastfeeding (22 July 2009)
Lesotho: HIV free babies bring hope (16 July 2009)
Early diagnosis and treatment save babies from AIDS-related death (27 May 2009)
Publications:
Towards Universal Access: Scaling Up Priority HIV/AIDS Interventions in the Health Sector (pdf, 3 Mb.)
UNAIDS Outcome Framework 2009-2011 (pdf, 388 Kb.)
Related

Feature Story
More than four million HIV-positive people now receiving life-saving treatment
30 September 2009
30 September 2009 30 September 2009
UNAIDS Executive Director presents the new WHO/UNAIDS/UNICEF report at the UN in Geneva, 30 September 2009. Credit: WHO/Christopher Black
Geneva / Paris -- More than 4 million people in low- and middle-income countries were receiving antiretroviral therapy (ART) at the close of 2008, representing a 36% increase in one year and a ten-fold increase over five years, according to a new report released today by the World Health Organization (WHO), the United Nations Children's Fund (UNICEF) and the Joint United Nations Programme on HIV/AIDS (UNAIDS).
Towards Universal Access: Scaling Up Priority HIV/AIDS Interventions in the Health Sector highlights other gains, including expanded HIV testing and counselling and improved access to services to prevent HIV transmission from mother to child.
"This report shows tremendous progress in the global HIV/AIDS response," said WHO Director-General Margaret Chan. "But we need to do more. At least 5 million people living with HIV still do not have access to life-prolonging treatment and care. Prevention services fail to reach many in need. Governments and international partners must accelerate their efforts to achieve universal access to treatment."
Treatment and Care
Access to antiretroviral therapy continues to expand at a rapid rate. Of the estimated 9.5 million people in need of treatment in 2008 in low- and middle-income countries, 42% had access, up from 33% in 2007. The greatest progress was seen in sub-Saharan Africa, where two-thirds of all HIV infections occur.
Prices of the most commonly used antiretroviral drugs have declined significantly in recent years, contributing to wider availability of treatment. The cost of most first-line regimens decreased by 10-40% between 2006 and 2008. However, second-line regimens continue to be expensive.
Despite recent progress, access to treatment services is falling far short of need and the global economic crisis has raised concerns about their sustainability. Many patients are being diagnosed at a late stage of disease progression resulting in delayed initiation of ART and high rates of mortality in the first year of treatment.
Testing and Counselling
Recent data indicate increasing availability of HIV testing and counselling services. In 66 reporting countries, the number of health facilities providing such services increased by about 35% between 2007 and 2008.
Testing and counselling services are also being used by an increasing number of people. In 39 countries, the total reported number of HIV tests performed more than doubled between 2007 and 2008.
Ninety-three percent of all countries that reported data across all regions provided free HIV testing through public sector health facilities in 2008.
Nevertheless, the majority of those living with HIV remain unaware of their HIV status. Low awareness of personal risk of HIV infection and fear of stigma and discrimination account, in part, for low uptake of testing services.
Women and Children
In 2008, access to HIV services for women and children improved. Approximately 45% of HIV-positive pregnant women received antiretroviral drugs to prevent HIV transmission to their children, up from 35% in 2007. Some 21% of pregnant women in low- and middle-income countries received an HIV test, up from 15% in 2007.
More children are benefiting from paediatric antiretroviral therapy programmes: the number of children under 15 years of age who received ART rose from approximately 198 000 in 2007 to 275 700 in 2008, reaching 38% of those in need.
Globally, AIDS remains the leading cause of mortality among women of reproductive age.
"Although there is increasing emphasis on women and children in the global HIV/AIDS response, the disease continues to have a devastating impact on their health, livelihood and survival," said Ann M. Veneman, UNICEF Executive Director.
Most-At-Risk Populations
In 2008, more data became available on access to HIV services for populations at high risk of HIV infection, including sex workers, men who have sex with men and injecting drug users.
While HIV interventions are expanding in some settings, population groups at high risk of HIV infection continue to face technical, legal and sociocultural barriers in accessing health care services.
"All indications point to the number of people needing treatment rising dramatically over the next few years," said Michel Sidibé, Executive Director of UNAIDS. "Ensuring equitable access will be one of our primary concerns and UNAIDS will continue to act as a voice for the voiceless, ensuring that marginalized groups and people most vulnerable to HIV infection have access to the services that are so vital to their wellbeing and to that of their families and communities."
More than four million HIV-positive people now re
Cosponsors
Press centre:
Download printable version (pdf, 40 Kb.)
Feature stories:
Governments and civil society expand access to HIV testing and counselling (30 September 2009)
More infants protected from HIV as access to antiretroviral drugs to prevent mother-to-child transmission increases (30 September 2009)
Contact:
In Geneva:
WHO
Saira Stewart
T: +41 22 791 2511
M: +41 79 467 2013
E: stewarts@who.int
UNAIDS
Sophie Barton-Knott
T: +41 22 791 1697
M: +41 79 514 6896
E: bartonknotts@unaids.org
In New York:
UNICEF
Kathryn Donovan
T: + 1 212 326 7452
E: kdonovan@unicef.org
In London:
Cathy Bartley
T: +44 20 8694 9138
M: +44 7958 561 671
E: cathy.bartley@bartley-robbs.co.uk
Claire Hoffman
T: +44 208 892 5215
M: +44 7977 440 353
E: claire.hoffman@bartley-robbs.co.uk
In Paris:
Michel Aublanc
T:+33 1 69 286 286
M: +33 6 08 719 795
E: michel.aublanc@orange.fr