Feature Story
How UNAIDS helped in the response to COVID-19 in the Islamic Republic of Iran
08 June 2022
08 June 2022 08 June 2022From the beginning of the COVID-19 pandemic, it was clear that life would be even more difficult for people living with HIV.
“When experts identified how COVID-19 affected people, it was clear that people with compromised immune systems needed to get a heightened level of care and attention,” said Fardad Doroudi, the UNAIDS Country Director for the Islamic Republic of Iran. “We needed to be quick and agile to mobilize our resources and expertise to make sure that no person living with HIV was left behind.”
Throughout the multiple waves of COVID-19 in the country, UNAIDS has provided critical support to people living with and affected by HIV, providing personal protective equipment and medicines, supporting nongovernmental organizations with small grants to help communities, developing information, education and communication materials and developing a community-based monitoring and evaluation framework.
Personal protective equipment, such as masks, shields, gloves and sanitizer, is a key tool in preventing the spread of viruses such as the virus that causes COVID-19. UNAIDS provided 95 tonnes of personal protective equipment to the Ministry of Health and Medical Education and the State Welfare Organization to be distributed through HIV-related nongovernmental organizations. Items provided included 1.8 million face masks, 60 000 bottles of hand sanitizer and 40 000 boxes of latex gloves, among other equipment.
Multimonth dispensing, ensuring that people living with HIV who are on HIV treatment receive enough treatment to last several months in order to avoid frequent visits to health centres, is a key pillar of an HIV response in humanitarian crises and was at the centre of UNAIDS’ efforts during the pandemic in the Islamic Republic of Iran.
To ensure that people on HIV treatment received their life-saving medicines, UNAIDS procured and delivered more than 650 000 doses of Vonavir, which covered the needs of more than 7000 people living with HIV for nearly three months, and more than 520 000 doses of Truvada, which covered the needs of nearly 3000 people living with HIV for six months. The more than 10 000 people helped with treatment received their medicines through treatment centres across the country.
Ten nongovernmental organizations working on HIV were awarded 26 small grants to increase community engagement and help people living with HIV adapt to life during the COVID-19 pandemic, and reached more than 14 000 people. Some of the activities funded by the grants include income generation schemes, home-care services, online sales and commerce, mental health support, the development of e-learning platforms, the distribution of hygiene kits, food and medicines and holding virtual events and forums for awareness-raising and stress reduction.
UNAIDS also helped in creating impactful information, education and communication material to enhance knowledge and build awareness of the COVID-19 pandemic. In collaboration with the national AIDS programme, UNAIDS supported the production and dissemination of a series of animations by a local nongovernmental organization. The 16-minute animation series, split into three episodes, covers topics such as the basics of HIV in relation to COVID-19, prevention of the virus in the context of HIV, the importance of continuing HIV treatment and addressing stigma and discrimination. The videos were featured across a number of online channels and platforms, receiving more than 15 000 views to date.
UNAIDS also developed and piloted a community-based monitoring and evaluation framework. This was born out of field monitoring activities carried out together with government partners and civil society organizations.
Online training sessions were organized for more than 200 people living with HIV and service providers. The sessions covered the basics of monitoring and evaluation of HIV-related COVID-19 programmes for nongovernmental organizations. The goal was to improve the effectiveness of monitoring and evaluation practices for HIV within the framework of the national strategic plan in order to improve the quality of HIV programmes in the country.
“Relying on strong collaborations and partnerships was key for our fast response during a rapidly changing time,” said Mr Doroudi. “With the support of donors, a strong liaison with national counterparts and effective collaboration with other United Nations agencies, we managed to be a part of the overall support to people living with HIV, who had to deal with the health, social and economic challenges associated with the COVID-19 pandemic.”
UNAIDS’ response to COVID-19 in the Islamic Republic of Iran was funded by the European Union’s humanitarian aid budget and was facilitated in partnership with the United Nations Children’s Fund. The Islamic Republic of Iran’s Ministry of Health and Medical Education and the State Welfare Organization were the key governmental partners for the wide range of activities undertaken as part of the project.
Region/country





Feature Story
Social enterprises and financial saving supporting Madagascan sex workers through COVID-19
15 March 2022
15 March 2022 15 March 2022A pioneer of the HIV response in Madagascar, Réseau Association des Femmes Samaritaines (Réseau AFSA, the Association of Samaritan Women), an association of sex workers, was created following the discovery of the first case of HIV among sex workers, in 1987. For the past three decades, it has been focusing on the empowerment and social integration of sex workers, with the objective of preventing the transmission of HIV and other sexually transmitted infections.
But the COVID-19 pandemic brought with it a new tide of socioeconomic hardships that saw sex workers suffer the world over. Income losses and lockdown restrictions, along with ingrained societal and systemic stigma and discrimination, have posed unique challenges for sex workers to protect their health and safety. In line with these complex global challenges, marginalized communities from Madagascar, one of the world’s poorest countries, have been adversely affected during these uncertain times.
Through the UNAIDS Solidarity Fund, which was created to economically empower key populations through social entrepreneurship, Réseau AFSA developed small business activities in the Antananarivo region. Réseau AFSA is supporting 10 sex workers with businesses in the production of food and the sale of fruit, vegetables and clothing, who are also being taught simplified financial management skills to empower their individual businesses.
UNAIDS spoke to Rarivoharilala Esther, Technical Coordinator at Réseau AFSA, about how the Solidarity Fund project is building community resilience and the financial capacity of the community members.
What is the purpose of your social enterprise project?
Our main purpose is to enable sex workers to effectively manage and lead their own businesses, thereby earning a sustainable income.
The added value of the social entrepreneurship project is that each beneficiary is encouraged to save part of their revenue into a savings account to ensure the continuation of their enterprises. This was made possible through a collaboration with the Madagascan Ministry of Post and Telecommunications, which created the savings accounts.
What problem do you want to solve through your social enterprise?
Through the social entrepreneurship activities, we are supporting sex workers, including those who have children to take care of.
The income earned through the social enterprises helps them to support the care of their children. In addition, having savings can ensure the continuity of their enterprises and, potentially, sustained care for their children.
What is your biggest concern about the project and how will you overcome it?
Our main concern now is to encourage the habit of continuous saving to ensure the sustainability of community-led enterprises. But with the response and improving management strategies we have seen from the community, I am confident that they are keen to continue these enterprises. Réseau AFSA is also committed to monitoring their enterprises and supporting them in the coming year. We are focused on mapping funders and partners to ensure the continuity of this project.
What do you want to achieve for the community in the future?
We hope that the benefits of this project extend to more community members. We also hope that the project reaches other regions or provinces of Madagascar.
As part of addressing hardships as a result of the COVID-19 pandemic, the Plateforme Océan Indien (Indian Ocean Platform) entrusted Réseau AFSA with the management and distribution of food, masks, soap and gels for more than one hundred sex workers as well as other key populations at higher risk of HIV and COVID-19, including lesbian, gay, bisexual, transgender and intersex people, people living with HIV and people who inject drugs. The network also improved access to health-care services and vaccines during the pandemic.
The next step in this inspiring journey remains to ensure the sustainability of the social enterprises and to look for partners who can enhance them. Instilling the habit of saving to foster the growth of their social enterprises and strengthen community members’ ability to care for their children is a first step in this direction.
Our work
Region/country




Feature Story
Networks led by young people in Asia and the Pacific find ways to adapt to COVID-19 and deal with uncertain futures
09 February 2022
09 February 2022 09 February 2022Health systems and communities have been pushed to the breaking point by the COVID-19 pandemic, a pandemic that the world was woefully unprepared for. Two years on, networks of key populations and people living with HIV are still at the forefront of the COVID-19 response, working to ensure that communities have access to timely and undisrupted HIV services. Among them is Youth LEAD, the network of young key populations in Asia and the Pacific, which in 2020 established the YKP COVID-19 Emergency Relief Fund to support initiatives led by young people in Asia and the Pacific.
One of the beneficiaries is Ya_All, an organization for young lesbian, gay, bisexual, transgender and intersex (LGBTI) people based in Manipur, India. “The second COVID-19 wave hit north-east India really hard, as it did across the country. We saw health-care systems collapse in front of our eyes. This greatly affected our work as we saw more and more young key populations experience delays in accessing HIV prevention services and saw an increase in mental health issues,” said Sadam Hanjabam, the founder and Chief Functionary of Ya_All. Thanks to the YKP COVID-19 Emergency Relief Fund, Ya_All supported 300 young LGBTI people and members of other key populations to access telecounselling services in five districts to help them with depression and other mental health issues.
Since the outset of the COVID-19 pandemic, the YKP COVID-19 Emergency Relief Fund has helped organizations led by and serving young people implement programmes that ensured young key populations and people living with HIV were not left behind in the HIV and COVID-19 responses. This included providing essential food and supplies of personal protective equipment, information on HIV and COVID-19 prevention and continued access to HIV prevention and treatment services, including mental health services. It also included establishing harm reduction programmes, distributing seed funding for businesses led by transgender people, providing housing and supporting digital and peer-led initiatives.
Funded through the Robert Carr Fund, the AIDS Health Care Foundation and the UNAIDS Regional Support Team for Asia and the Pacific, the YKP COVID-19 Emergency Relief Fund has supported more than 20 projects from 15 organizations led by young people across the region, and has made a considerable difference to the lives of young key populations.
The Viet Nam Young Key Populations Network is one of the beneficiaries of the fund in Viet Nam. Even though the country was in complete lockdown for a substantial period, with a seed grant the network managed to produce HIV and sexual and reproductive health and rights digital educational content for young people at risk of HIV, distributing harm reduction materials to 15 provinces across the country.
Similarly, YPEER Pilipinas, another beneficiary of the fund, trained 1000 young people on HIV combination prevention strategies and screened more than 900 young people for HIV. With a small grant, they were able to scale up the #GetCondomPH Programme, which resulted in successfully distributing more than 11 000 condoms across the Philippines.
In Cambodia, KHANA has given mental health support training to more than 70 LGBTI leaders. The training accelerated ongoing mental health peer support to key affected populations who were experiencing mental health issues. “Online counselling sessions on how to cope with mental health issues were incredibly helpful. The YKP COVID-19 Emergency Relief Fund was an effective mechanism that allowed us to provide timely support to young people in need of HIV prevention and other health services,” said Phorng Chanthorn, Senior Coordinator at KHANA.
These few examples out of the many show that young people, communities and civil society play a crucial role in pandemic responses, helping HIV programmes rebound and adapt to COVID-19 rapidly. Still, these efforts have not been easy. “Youth networks are trying to find ways to recover, adapt and effectively lead in this new funding landscape that has resulted in greater competition for donor funding. Many programmes, including this one, showcase the impact and necessity of supporting youth-led HIV programmes and initiatives. However, it’s not enough,” said Vanessa Monley, Programme Officer at Youth LEAD.
In 2020, young people accounted for 26% of new HIV infections in Asia and the Pacific. In some countries, close to half of new HIV infections were among young people, and one in three members of young key populations do not know their HIV status.
“It is critical to find innovative ways to continue to scale up access to HIV services for young key populations in the context of COVID-19, ensuring that we do not give up achieved gains, and to respond to the additional issues that have come with the pandemic, such as mental health and social support issues. UNAIDS is fully committed to supporting responses led by young people and ensuring their sustainability as we work collectively to end AIDS by 2030,” said Taoufik Bakkali, Director, a.i., of the UNAIDS Regional Support Team for Asia and the Pacific.
Our work
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa


Feature Story
New report highlights vital role of community-led organizations in pandemic response and preparedness
28 January 2022
28 January 2022 28 January 2022In a new UNAIDS report, Holding the line: communities as first responders to COVID-19 and emerging health threats, organizations led by and for people living with HIV and key populations detail their efforts to respond to the colliding pandemics of COVID-19 and HIV. Drawing on qualitative survey data spanning 225 community-led organizations across 72 countries, the report provides a snapshot of the organizations’ work during early 2020 to sustain the HIV response while supporting their communities through the COVID-19 pandemic. The report also illuminates the high-priority actions that are still urgently needed to ensure the continuity of HIV-related services, as well as the sustainability of the community-led organizations providing them.
In community members’ own words, the report tells a story of the phenomenal resourcefulness of community-led organizations to mobilize when and where governments could not. Their stories show that organizations led by and for people living with HIV and key populations, including women and young people, have leveraged in-depth HIV knowledge into broader pandemic expertise. In the face of service interruptions, health commodity shortages, curfews and severe funding gaps, the organizations adapted rapidly to continue providing HIV-related services.
Community-led organizations reported becoming more involved in distributing antiretroviral medicines and self-testing kits, negotiating with government officials to ensure that medicines would be accessible and personally delivering them to beneficiaries. Many organizations also reported shifting their services online, as well as relying on telephone and email contact for personal counselling and monitoring of health status, with some even making home visits in urgent circumstances. Material support, including food packages and income supplements, was mobilized and distributed to those in greatest need.
Organizations also undertook COVID-19-related service provision. They began outreach to community members and the broader public to raise awareness about COVID-19 and share information about how people could protect themselves. They detected and responded to rising levels of gender-based violence, providing assistance and support to survivors. They also distributed masks, soap and hand sanitizer, and constructed handwashing facilities. When the cost and availability of masks and soap became an issue, many community-led organizations reported finding innovative ways to produce these items themselves.
However, the majority of these organizations were distressed that their absence—especially from planning and decision-making processes—was resulting in the failure of national COVID-19 responses to address the needs of their communities. They repeatedly expressed deep concern about the economic impact of lockdowns and travel restrictions on their beneficiaries. They also highlighted continuing difficulties in obtaining personal protective equipment and travel approval, public transport or private vehicles for their staff.
Organizations reported shouldering extremely heavy burdens with little external support. Intense funding gaps left staff in these organizations exhausted and working nights and weekends to fundraise, usually unsuccessfully, with some even turning to their own personal salaries and savings to help their communities.
Community-led organizations are at the heart of a people-centered, human rights-based public health response. UNAIDS has repeatedly called for support and funding for community-led infrastructure, emphasizing that communities urgently need the space and the resources to lead.
“Community-led organizations have guided us through two pandemics, first the AIDS pandemic and now COVID-19,” said Winnie Byanyima, Executive Director of UNAIDS. “Their central and critical role in providing services at the heart of communities, reaching the most vulnerable, must be recognized and valued. Collectively, we must do more to support them financially, engage them meaningfully in decision-making processes and ensure they have all the resources they need to continue their work in responding to HIV and COVID-19 and for future pandemics.”
Where public health systems have engaged community-led networks and organizations and empowered those most affected by pandemics, they have been more successful at countering disinformation, ensuring the continuity of health services and protecting the rights and livelihoods of the most vulnerable. This is what it means to put people at the centre of pandemic responses.
In order to ensure the sustainability of a community-led HIV response, the report calls for five measures to be adopted as a matter of urgency:
- Community-led organizations must be fully included and integrated into national pandemic responses, including the continuing COVID-19 responses. This cannot be limited to consultation and should take place at the level of policy development, planning, design and evaluation of interventions.
- Short-term emergency funding must be mobilized and made readily available to community-led organizations.
- A stable, long-term funding base must be established to enable community-led organizations to function effectively.
- The information base on the work of community-led organizations must be expanded and deepened through systematic documentation, identification of good practices and information-sharing.
- Continuity of HIV-related services must be guaranteed, including through expanding funding to community-led organizations and establishing collaborative arrangements between community-led organizations and medical facilities to ensure sustainability of the HIV response through COVID-19 and future pandemics.
Documents
2021 UNAIDS Global AIDS Update — Confronting inequalities — Lessons for pandemic responses from 40 years of AIDS
14 July 2021
UNAIDS report shows that people living with HIV face a double jeopardy, HIV and COVID-19, while key populations and children continue to be left behind in access to HIV services. Read the press release | Data slides | This document is also available in Arabic

Update
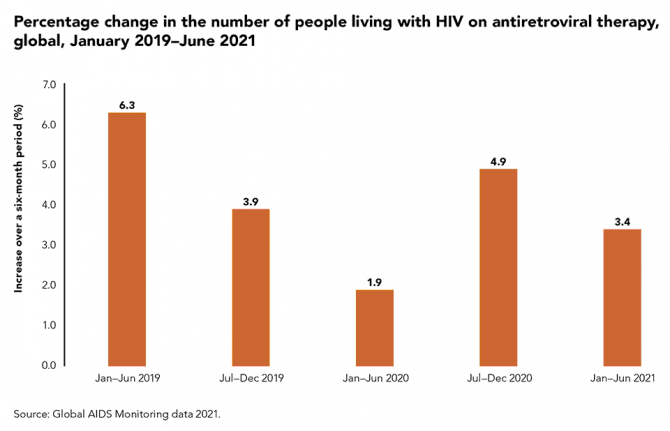
COVID-19 hit treatment take-up, but 28.2 million people living with HIV now on treatment
06 December 2021
06 December 2021 06 December 2021There have been substantial setbacks in the HIV response during the COVID-19 pandemic, particularly when many countries were in their first lockdowns and HIV programmes were scrambling to adapt, but there have also been many inspiring examples of adaptation and resilience.
The number of people living with HIV receiving antiretroviral therapy increased by just 1.9% between January and June 2020, from 25.5 million people to 26.0 million people. This was followed by an accelerated 4.9% increase from July 2020 to December 2020, reaching 27.3 million people, and then a 3.4% increase during the first six months of 2021. At the end of June 2021, there were 28.2 million people living with HIV on treatment globally.
Our work
Related

Press Statement
UNAIDS welcomes the first WHO COVID-19 Technology Access Pool licensing agreement
24 November 2021 24 November 2021GENEVA, 24 November 2021—UNAIDS welcomes the first licensing agreement under the World Health Organization (WHO) COVID-19 Technology Access Pool (C-TAP) initiative, negotiated between Consejo Superior de Investigaciones Científicas (Spain’s High Council of Scientific Research) and the Medicines Patent Pool.
The C-TAP initiative builds on a successful model to increase access to HIV, tuberculosis and hepatitis C products in low- and middle-income countries and has proved to be effective in overcoming some barriers to access to health technologies for COVID-19. However, the initiative has so far been underutilized, and pharmaceutical companies and other holders of COVID-19 technologies have been reluctant to join C-TAP.
“I welcome this new agreement, but urge other pharmaceutical companies and COVID-19 technology-holders to share their know-how,” said Winnie Byanyima, Executive Director of UNAIDS. “Think of how many lives could be saved if COVID-19 vaccines, medicines and other technologies were available through this mechanism to everyone who needs them.”
The new licensing agreement shows that it is possible to share knowledge, technology and intellectual property rights in the fight against COVID-19.
The sharing of intellectual property rights, data and know-how should be a fundamental component of pandemic preparedness and response. UNAIDS encourages research institutes and holders of life-saving technologies, including vaccine manufacturers, to follow suit and join C-TAP and urges the governments of countries that host pharmaceutical companies to ensure that their technologies are offered to C-TAP as a matter of urgency.
The agreement contains key access provisions, such as the non-exclusive right to develop the licensed patents, know-how and material. There is no geographical limitation, so qualified companies worldwide will be able to develop the licences and commercialize the products derived from them. The terms of the agreement will be publicly available, ensuring transparency. The agreement includes a technology transfer package.
The agreement covers the licensing of a technology to detect antibodies to SARS-CoV-2, the virus that causes COVID-19, from either COVID-19 infection or a vaccine, and will allow the measurement of the effectiveness of vaccination programmes and help in the management of vaccination booster programmes. The tests derived from the technology are simple to use, which will allow their application in resource-limited settings, and companies based in low- and middle-income countries will not have to pay royalties for the technology’s use.
UNAIDS was a supporter of a call for action in May 2020, led by the Government of Costa Rica and WHO, which led to the setting up of C-TAP. UNAIDS is a member of the C-TAP Steering Committee.
UNAIDS thanks the Government of Spain for backing and facilitating the agreement and for its financial support of C-TAP.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Documents
2021 World AIDS Day report — Unequal, unprepared, under threat: why bold action against inequalities is needed to end AIDS, stop COVID-19 and prepare for future pandemics
29 November 2021
This document is also available in Arabic

Press Release
UNAIDS warns of millions of AIDS-related deaths and continued devastation from pandemics if leaders don’t address inequalities
29 November 2021 29 November 2021GENEVA, 29 November 2021—UNAIDS issued a stark warning today that if leaders fail to tackle inequalities the world could face 7.7 million* AIDS-related deaths over the next 10 years. UNAIDS further warns that if the transformative measures needed to end AIDS are not taken, the world will also stay trapped in the COVID-19 crisis and remain dangerously unprepared for the pandemics to come.
“This is an urgent call to action,” said UNAIDS Executive Director Winnie Byanyima. “Progress against the AIDS pandemic, which was already off track, is now under even greater strain as the COVID-19 crisis continues to rage, disrupting HIV prevention and treatment services, schooling, violence-prevention programmes and more. We cannot be forced to choose between ending the AIDS pandemic today and preparing for the pandemics of tomorrow. The only successful approach will achieve both. As of now, we are not on track to achieve either.”
The warning comes in a new report by UNAIDS launched ahead of World AIDS Day (1 December) entitled Unequal, unprepared, under threat: why bold action against inequalities is needed to end AIDS, stop COVID-19 and prepare for future pandemics.
Some countries, including some with the highest rates of HIV, have made remarkable progress against AIDS, illustrating what is feasible. However, new HIV infections are not falling fast enough globally to stop the pandemic, with 1.5 million new HIV infections in 2020 and growing HIV infection rates in some countries. Infections are also following lines of inequality. Six in seven new HIV infections among adolescents in sub-Saharan Africa are occurring among adolescent girls. Gay men and other men who have sex with men, sex workers and people who use drugs face a 25–35 times greater risk of acquiring HIV worldwide.
COVID-19 is undercutting the AIDS response in many places. The pace of HIV testing declined almost uniformly and fewer people living with HIV initiated treatment in 2020 in 40 of 50 countries reporting to UNAIDS. HIV prevention services have been impacted—in 2020, harm reduction services for people who use drugs were disrupted in 65% of 130 countries surveyed.
“It is still possible to end the epidemic by 2030,” affirmed United Nations Secretary-General António Guterres in his World AIDS Day message. “But that will require stepped up action and greater solidarity. To beat AIDS—and build resilience against the pandemics of tomorrow—we need collective action.”
This new report from UNAIDS examines five critical elements of the plan agreed by Member States at the United Nations General Assembly High-Level Meeting on AIDS that must be urgently implemented to halt the AIDS pandemic and which are critical but under-funded and under-prioritized for pandemic prevention, preparedness and response. These include:
- Community-led and community-based infrastructure.
- Equitable access to medicines, vaccines and health technologies.
- Supporting workers on the pandemic front lines.
- Human rights at the centre of pandemic responses.
- People-centred data systems that highlight inequalities.
The call for upscaled investments and shifts in laws and policies to end the inequalities that drive AIDS and other pandemics is backed by leaders in global health and pandemic response from across the world.
“If we do not take the steps needed to tackle the inequalities driving HIV today, not only will we fail to end the AIDS pandemic, we will also leave our world dangerously unprepared for future pandemics,” said Helen Clark, Co-Chair of the Independent Panel for Pandemic Preparedness and Response, in a special foreword to the UNAIDS report. “Pandemics find space to grow in the fractures of divided societies. The amazing scientists, doctors, nurses and communities who work to end pandemics cannot succeed unless world leaders take the steps that will enable them to do so.”
UNAIDS and global health experts emphasize that while business as usual would kill millions and leave the world trapped with colliding pandemics going on for decades, leaders can, by acting boldly and together to tackle the inequalities in which pandemics thrive, end AIDS, overcome the COVID-19 crisis and be protected from the pandemic threats of the future.
“Pathogens ranging from HIV to the virus behind COVID-19 invade the cracks and fissures in our society with startling opportunism,” said Paul Farmer of Partners in Health, a nonprofit that for decades has effectively treated AIDS in settings of material poverty. “That the AIDS pandemic is shaped by deep structural inequalities need not resign us to inaction, however. Our teams, in rural Haiti and across the world, have routinely shown that with comprehensive care delivery, robust forms of accompaniment and social support and a larger dose of social justice, disparities in HIV outcomes can be rapidly narrowed, and health systems swiftly strengthened. We shouldn’t settle for anything less.”
This year marks 40 years since the first cases of AIDS were reported. Since that time, where investments have met ambition, there has been huge progress, particularly in expanding access to treatment. By June 2021, 28.2 million people had access to HIV treatment, up from 7.8 million in 2010, although progress has slowed considerably.
Countries with laws and policies aligned to evidence, strong community engagement and participation and robust and inclusive health systems have had the best outcomes, whereas the regions with the largest resource gaps and countries with punitive laws and that have not taken a rights-based approach to health have fared the worst.
“We know what works from seeing brilliant AIDS responses in some places,” said Ms Byanyima, “but we need to apply that everywhere for everyone. We have an effective strategy that leaders adopted this year, but it needs to be implemented in full. Ending inequalities to end AIDS is a political choice that requires bold policy reforms and requires money. We have reached a fork in the road. The choice for leaders to make is between bold action and half-measures.”
* The estimate of 7.7 million AIDS-related deaths between 2021 and 2030 is what UNAIDS models predict if HIV service coverage is held constant at 2019 levels. If the Global AIDS Strategy 2021–2026: End Inequalities, End AIDS is executed and the 2025 targets are achieved, UNAIDS estimates that at least 4.6 million of those deaths can be averted over the decade.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.