


Feature Story
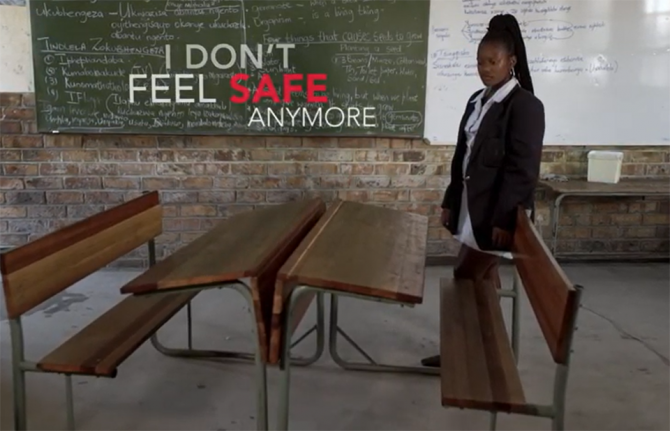
Gender-based violence and COVID-19—“When we are silent, we allow these crimes to multiply”
19 May 2020
19 May 2020 19 May 2020UN Women estimates that globally in the past 12 months 243 million women and girls aged 15–49 years were subjected to sexual and/or physical violence perpetrated by an intimate partner. As a result of the lockdowns imposed to stop the spread of COVID-19, emerging data show that such violence has intensified. In France, for example, reports of domestic violence have increased by 30% since the lockdown started on 17 March, and in Argentina emergency calls about domestic violence have increased by 25% since its lockdown started on 20 March. Many other countries have reported such increases.
Recently, the Odnoklassniki social network, known as OK, hosted a broadcast for experts and others to discuss how to survive lockdown and avoid family conflict and gender-based violence. The broadcast was seen by 1.7 million OK network users across eastern Europe and central Asia.
“I live in Kyrgyzstan,” Ulzisuren Jamstran, a representative of UN Women in Kyrgyzstan, said. “Here, according to the government, the level of domestic violence increased by 65%. We see an increase in aggression against women and children in Kyrgyzstan, we see an increase in suicides among children, even young children.”
Lyudmila Petranovskaya, a Russian psychologist, explained how isolation made good relationships become better and problematic relationships become more problematic. She emphasized that people need to be aware of the options if they are locked down with an abuser. “People have to look for contacts, a hotline, call friends, try to find another place to survive isolation. Staying with the abuser is dangerous. This threat is more serious than coronavirus,” she said.
Julia Godunova, Deputy Head of the Board of the Eurasian Women’s Network on AIDS, spoke about studies in eastern Europe and central Asia that show that more than 70% of women who survived violence do not seek help because of the perceived shame.
Dina Smailova, the founder of the #DontBeSilentKZ nongovernmental organization, addressed female survivors of violence. “When we are silent, we allow these crimes to multiply. I urge women not to be silent. Our movement is expanding, we are active not only in Kazakhstan, but also in other countries of central Asia and beyond.”
The broadcast highlighted successful experiences around the world in responding to gender-based violence. The example in Spain, where women in danger can visit pharmacies and use a code word to alert staff that they need help, was praised. The role of the private sector was also shown to be important—since many shelters are not open at present, hotels are stepping in and providing shelter, either for free or at a minimal cost.
The broadcast was part of a joint initiative of the UNAIDS regional office for eastern Europe and central Asia, the UNESCO Institute for Information Technologies in Education and OK, in partnership with the regional office of UN Women for eastern Europe and central Asia.
When will men stop thinking that women’s bodies are their property?
Related

Feature Story
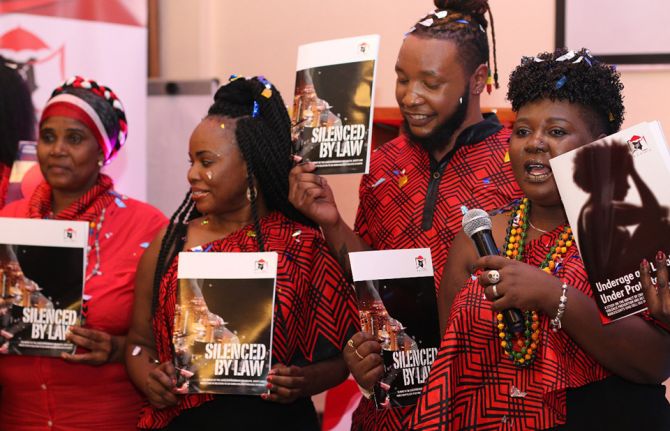
Kenyan sex workers abandoned and vulnerable during COVID-19
20 May 2020
20 May 2020 20 May 2020During the more than a decade that Carolyne Njoroge worked as a sex worker, she never saw such violence against her peers. Now working full time for the Kenya Sex Workers Alliance (KESWA), she said that the COVID-19 lockdown threw everyone into disarray.
“At the outbreak, no one was prepared for the coronavirus,” she said. “It’s not like the rains that we know and can prepare for.”
The government’s lockdown measures to limit the spread of the virus—a dusk-to-dawn curfew and shutting of bars and nightclubs—have left sex workers in Kenya to either work during the day and be very visible or to break the curfew at night.
So far, KESWA has reported that more than 50 sex workers have been forcefully quarantined during the early days of the pandemic, and women have been arrested for not adhering to the social distancing rules and obligatory mask-wearing.
“How do you expect women to adhere to these measures when they cannot feed themselves and their families and many of them don’t even have homes?” Ms Njoroge asked.
Kenya does not criminalize sex work. However, the law forbids “living on the earnings of sex work” and “soliciting or importuning for immoral purposes,” which Ms Njoroge said means that the women work in a grey area. “It’s a very hostile work environment and sex workers are the first to be violated because they say our work is not work,” she said.
Phelister Abdalla, a sex worker living with HIV and KESWA’s National Coordinator, said, “Sex workers need to be protected, but if we are told to stay at home we need to be given food.”
The government has not released funds or directed aid to sex workers, so KESWA started a fundraiser to dispatch hygiene packs, which include hand sanitizer, masks and menstrual pads, as well as food baskets.
Ms Njoroje said that 100 sex workers from the informal settlements had benefitted. “Our challenge is keeping up with demand, so we are reaching out to others for help,” she said.
Ms Abdalla said that fighting the pandemic together is key. “If we want to end COVID-19, we should not be judged by the type of job we do,” she said. “We are first and foremost Kenyans, so treat all of us equally.”
Fifty-seven Kenyan civil society and nongovernmental organizations, including KESWA, drafted an advisory note to the Kenyan Government to urge it to put in place safety nets to cushion the communities and people who cannot afford to not work. They also urged them to stop security forces from enforcing measures around social distancing and curfews. The note adds, “We cannot use a “one size fits all” approach for COVID-19” and calls upon the United Nations leadership to help safeguard the progress.
The Kenyan Government, through the National AIDS and STI Control Programme (NASCOP), in partnership with county governments, implementing partners and donors continues to work to ensure the continuity of KP service delivery during the confinement measures. NASCOP issued technical guidance to all services including information, education and communication materials e.g. posters, setting up virtual coordination platforms, capacity building of service providers on HIV in the context of COVID-19 and they have instituted advocacy efforts to raise resources to ensure that service providers, including outreach teams, and Key Population led groups have personal protective equipment (PPE) and sanitizers. Mobile dispensing services for people who use drugs and tailored outreaches have been established to enhance service delivery along with the formation of virtual psychosocial support groups distribution of food baskets to the very vulnerable and help/hotlines for violence response have been sustained.
UNAIDS collaborates with governments to ensure that international human rights law are respected, protected and fulfilled, without discrimination, in line with state obligations, including in times of emergency.
Our work
Region/country
Related


Press Statement
UNAIDS urges governments to ensure that HIV service providers from community-led organizations are recognized as essential service providers in the context of COVID-19
18 May 2020 18 May 2020GENEVA, 18 May 2020—A cornerstone of the response to HIV, community-led health service delivery has become even more critical in the context of COVID-19, as the needs of marginalized community members and the burden on the health sector are increasing, making it vital that continued provision of HIV, tuberculosis and other health services is secured. Community-led organizations are providing a lifeline to underserved, marginalized and hard-to-reach populations around the world.
Physical distancing restrictions have created significant challenges for those needing to access essential services, creating an increased burden on community organizations, which are at the centre of service delivery.
UNAIDS recognizes that community organizations have an unparalleled depth of experience in creating and delivering responses to health and human rights crises within their communities. The many community-led networks and groups that emerged to respond to HIV possess immense practical experience, organizational strength and unparalleled community access for facilitating the delivery of life-saving support, and for influencing people’s real-life practices to better protect their health.
Community-led networks and organizations have also developed important working relationships and roles within health and community systems, including in coordination and task-shifting functions. As evidenced in many countries, these capacities can, with proper support, be deployed to facilitate the provision of COVID-19 information, prevention, testing and linkages to care. Yet without formal recognition of the essential nature of their work, they face significant barriers to continuing to provide services. It is the view of UNAIDS that it is critical to the COVID-19 response and to mitigating broader health impacts of the pandemic that community-led organizations be supported to continue to provide essential services and have the protective equipment and safe policy environment necessary to do so.
The role of community-led organizations must be appropriately recognized and supported in the context of COVID-19. They must be factored into all aspects of planning, design and implementation of interventions to combat both COVID-19 and the efforts required to mitigate the impact of COVID-19 on other health areas, including HIV and tuberculosis. In particular, and as first steps in this effort, UNAIDS urges COVID-19 crisis committees at the national and district levels to:
- Include the workforce of community-led health care services into the lists of essential service providers and treat them as equivalent to health-care providers.
- Design physical distancing restrictions and policies in ways that allow community-led services to continue operating safely. Essential services include, but are not limited to, the physical provision of HIV, tuberculosis and COVID-19 and other health services that include prevention commodities, including condoms, lubricants, clean needles and opioid substitution therapy, contraceptives, hygiene kits, test kits, medication, triage and linkage to care, adherence support, packages of food and other essentials, the provision of legal services and protection for survivors of gender-based violence and other forms of violence and discrimination. Particular attention needs to be paid to people with physical disabilities.
- Provide special authorization to relevant community-led service providers to move freely, with appropriate personal protective equipment, to deliver the services when and where needed.
- Ensure that community-led organizations, networks and groups be provided with personal protective equipment and training in order to protect themselves and their clients in the course of service delivery.
- Take urgent measures to ensure the security, and expansion, of existing funding for community-led organizations, so that those organizations can continue to provide services.
- Ensure inclusive and transparent governance of COVID-19 responses, with decision-making bodies that include representatives of community-led organizations, including those focused on gender, equity and human rights, to ensure that COVID-19 policies are designed to support the range of service providers and activities necessary for an effective and equitable response.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Press centre
Download the printable version (PDF)




Feature Story
COVID-19 community support for Trinidadians on the margins
18 May 2020
18 May 2020 18 May 2020Delores Robinson’s days are usually busy. She heads GROOTS Trinidad and Tobago, a civil society organization that provides psychosocial care for people living with HIV. It also manages a transition house that provides shelter and services for displaced members of key populations.
But since the first COVID-19 case in the country was confirmed, on 12 March, Ms Robinson’s workdays have become a whirlwind. The government’s containment measures—a stay-at-home order and a shutdown of all non-essential business—have thrust the most vulnerable people further into the margins.
GROOTS Trinidad and Tobago is an example of how civil society organizations can move quickly to identify and respond to the needs of the voiceless. Ms Robinson, a Jamaican, has lived in Trinidad and Tobago for the past 34 years. During conversation she alternates between wide, open smiles and a furrowed brow. These days there’s lots to worry about.
Every day she prepares meals for 30 families. She then personally delivers them. There is no structured funding for this effort—just money and other contributions from HIV response stakeholders.
There’s a unique story at each drop-off point. Today she manoeuvres through the narrow roads of Sea Lots, a low-income community in the shadow of the capital city, Port of Spain. The men on the block recognize her car. One offers to deliver her parcel. She laughs. Ms Robinson has come to visit the seven children of a single mother living with HIV who is currently hospitalized.
The Government of Trinidad and Tobago has provided a range of COVID-19 relief options. These include salary relief, rental assistance grants and nutrition support. Sometimes, Ms Robinson’s role is to help clients navigate government systems. For example, one illiterate mother living with HIV lost her food card and needs help getting it replaced.
“The forms are complicated for many people, plus they don’t have an Internet service,” Ms Robinson explained. “Now that we are all being encouraged to conduct business online, many have no access.”
Since the stay-at-home orders went into effect, she’s been asked by the police to accommodate women and children at the transitional home. The combination of income loss and constant contact has exacerbated abusive situations, leading to a spike in reports of domestic violence.
Ms Robinson reports that her clients living with HIV have so far had no problem accessing their treatment. Before COVID-19, it was standard practice for Trinidad and Tobago clinics to dispense two- to three-month supplies of HIV medicines at a time. HIV treatment facilities and sexually transmitted infection clinics remain open, although they have altered hours.
“They have their meds,” she said. “What they need most now is nutritional support to be able to stay healthy and take their treatment.” And they need masks.
UNAIDS Caribbean is advocating for governments in the region to ensure that community organizations like GROOTS are included in decision-making and planning around meeting the needs of vulnerable populations during the COVID-19 crisis. They are an essential service, ensuring that people’s most basic needs are met. These organizations should be included in contingency plans for connecting people living with HIV to services. And they should be resourced.
“We think we’re all in this together, but there are many people who don’t have the things we take for granted—a safe home, healthy food and the ability to speak out. It’s tiring work but it’s needed now more than ever,” Ms Robinson said.
Our work
Region/country


Feature Story
New videos highlight LGBTI issues in Brazil
16 May 2020
16 May 2020 16 May 2020Two new videos released ahead of the International Day against Homophobia, Transphobia and Biphobia, celebrated on 17 May, highlight different aspects of what it means to be part of the lesbian, gay, bisexual, transgender and intersex (LGBTI) community in Brazil.
‘What is the impact of diversity at the workplace? created by the Free & Equal Campaign, in partnership with the UNAIDS, seeks to inspire people by sharing examples of companies committed to tackling discrimination against transgender people in the workplace, in the formal labour market and in the community.
The second video features Brazilian LGBTI people and members of the electronic music scene raising awareness on COVID-19 and its impact on the LGBTI community. In just four days, the video reached more than 100 000 people with a message on the importance of staying at home.



Feature Story
Let transgender people be in the picture
14 May 2020
14 May 2020 14 May 2020Relief work is not the Humsafar Trust’s specialty, but COVID-19 has changed that.
A few days after the lockdown measures in India went into effect, the Humsafar Trust’s teams received desperate calls from people with no place to live and no income, explained Vivek Anand, Chief Executive Officer of the Humsafar Trust, a lesbian, gay, bisexual, transgender and intersex (LGBTI) people community-based nongovernmental organization based in Mumbai, India. An urgent team meeting was called to determine what to do. “After much back and forth evaluating needs, we agreed, “Let’s start with giving people food support,”” he said.
They pooled money together among themselves and bought food and other essentials.
They then reached out to their communities, telling them that the Humsafar Trust had started an emergency COVID-19 fund. In three days, more than 700 people had asked for support. “With donations from communities, allies, businesses and some donor agencies, we have helped more than 2000 individuals with food, access to medical care, like HIV medicine, financial aid and applying for government support,” Mr Anand said, beaming as his air conditioner sent waves of cold air blowing through his small home office.
He feels that during the pandemic response the LGBTI community is being overlooked. “Seventy per cent of our community comes from lower socioeconomic backgrounds with no savings,” he said.
The bulk of the Humsafar Trust’s aid is focused on transgender people, who, he said, have been the hardest hit. “Not only do they usually survive on a meagre income, a lot of them have no legal papers, making them invisible to government aid,” Mr Anand said.
The lockdown has translated into financial distress and has also resulted in mental stress. Mr Anand recounted that one member of his transgender team at the Humsafar Trust cannot introduce herself during their online outreach sessions because she is living with her parents, who consider her a boy. Others are being pressured to marry, while many have been mistreated and beaten.
Standing outdoors by a vegetable vendor to maximize cellphone connectivity, Shreya Reddy said she always wanted to be a woman. Despite being born a boy and constant ridicule and shaming, she never gave up. At the age of 13 years, she ran away and joined a hijra community, comprised mostly of transgender people. Four years later, she started transitioning gender with money she made as a sex worker. After a while, Ms Reddy said, she realized that to succeed, she needed to study. Her social work degree and background led her to the Humsafar Trust, for which she has become a peer educator and outreach worker. COVID-19 has set her back a bit for a number of reasons.
“It has been terrible, because I cannot get my hormones and I have lost weight and was bleeding,” she said. She added that because of the lockdown, no one can get regular check-ups with gynecologists. “And my community cannot understand all the rules and the science language. Basically, a lot of people like me are struggling a lot, from not being able to pay rent to buying bare necessities,” Ms Reddy said.
Speaking more and more quickly, she added, “People are not that educated, they are scared and there are lots of mistruths.”
Ms Reddy has since become better and said that she is dedicated to her outreach work. One of her transgender peers told her, “Better that I die,” once the woman’s income had melted away. "I empower myself by talking to people,” she said. “We are all so vulnerable and as a small-income population we need support.”
OutRight Action International's recent report, Vulnerability amplified: the impact of the COVID-19 pandemic on LGBTIQ people, said that the challenges faced by LGBTI people across the world as a result of the virus and containment measures were amplified compared to the broader population. Jessica Stern, Executive Director of OutRight, said, “For us the situation is dire. I fear how many LGBTI people will lose their lives because of the amplified vulnerability we face.”
Pointing to market vendors behind her, Ms Reddy said, “I have helped them too figuring out the masks and sanitizers. I help everyone, but I am scared about the future.”
Mr Anand echoed her sentiment. He has had to extend the emergency fund until August.
“Every day, there is a new challenge,” he sighed. His teams, usually out and about, can’t all work online. In addition, he mentioned that more and more people are going underground, making outreach difficult.
Recalling his youth, he explained that he was a late bloomer. “I didn’t know anyone who was gay,” he said. When his secret relationship of nine years ended, he had no one to talk to. He felt lonely and abandoned. “From then on, the Humsafar Trust became my home and my family.” He added that he would not judge anyone in these tense times, reiterating that his first duty was to help others.
What he really wants is that the transgender community be part of the narrative. “Give them a voice, let them be seen and include them in the picture,” he said.
Our work
Region/country




Feature Story
“We are human, so of course it was scary”
13 May 2020
13 May 2020 13 May 2020She is sitting opposite, dressed in a lab coat, and you know that with her you are in safe hands. Her kind eyes convey empathy. Malikakhon Kurbanova, known to all who know her as Malika, has been a nurse at the Kyzyl-Kiya family medical centre in Kyrgyzstan for almost 20 years.
Part of one of 10 pilot multidisciplinary teams specializing in infectious diseases in the country, she has been working with people living with HIV for many years. The multidisciplinary teams were formed by UNAIDS in 2013 and include a specialist in infectious diseases or a family doctor, a nurse and a peer consultant. The teams aim to improve the quality of medical and social services for people living with HIV and their families. During the COVID-19 outbreak they are receiving extra financial help from a Russian technical assistance programme.
Like many health-care workers, Malika has been caught up in the fight against COVID-19. UNAIDS met her recently in her office in the clinic, adjacent to a blossoming apple orchard, and spoke to her about her background and work.
Why did you decide to become a nurse?
When I was a child, I was quite often sick. My mother and I spent a lot of time in hospitals. I always admired the women who wore lab coats and who knew how to inject me painlessly. I knew then that I would become a nurse and help people. When I graduated from school in 1986, I entered the Kyzyl-Kiya medical college and after that, in 1989, I went to work in the health unit in a construction materials plant. That is how my story began. In the beginning of the 2000s the reform of primary health care started and family medical centres were created. I came to work as a nurse and soon joined the infectious diseases unit, where I still work.
You have been working in the COVID-19 response since the very start of the epidemic in the country. Were you frightened?
We do house-to-house visits, helping people with acute respiratory infections. We are human, so of course it was scary—I was afraid about infecting my family.
It is frightening when you are fighting an unknown virus. In the beginning, I did not know what I should tell patients. At the beginning of the pandemic, many people did not believe the truth about COVID-19; some of them accused us of trying to infect them. But over time, people realized that the virus was real, which greatly helped our work.
You work as a nurse in a multidisciplinary team for people living with HIV. How has your work changed since the COVID-19 outbreak started?
To avoid people running out of their medicine and to reduce their possible exposure to people with COVID-19, we are now distributing three-month supplies of antiretroviral therapy, when before we gave out one-month supplies.
We also focus on psychosocial support for people living with HIV. People need mutual support. Our peer consultant calls patients every day and holds online self-help groups via WhatsApp. Thanks to the financial support given to the project, the transport costs of visiting clients and monitoring their adherence to antiretroviral therapy is covered. The most vulnerable people living with HIV have been receiving food packages since April.
What is the hardest part of your work?
We’ve always had difficulties and they are likely to continue, that is the nature of our work! Sometimes I feel like leaving it at behind, but then I realize that this is my life—I am a nurse. It gives me strength when I see that my actions for my patients bring results and people get better.
Our work
Region/country
Related




Feature Story
Russian regional AIDS centres leading the fight against COVID-19
14 May 2020
14 May 2020 14 May 2020The network of the Russian Federation’s more than 100 AIDS prevention and control centres, established in 1989 to respond to HIV, has been mobilized to support the country’s fight against COVID-19.
Each of the centres, which specialize in HIV surveillance, prevention, testing and treatment, has high-technology laboratory equipment, highly qualified health staff, including infectious disease specialists and epidemiologists, and expertise in epidemiological surveillance and contact tracing. Those centres are now using their technology and expertise on HIV testing and diagnosis to scale-up testing for COVID-19.
Public health experts at the AIDS centres are also supporting epidemiological surveillance and contact tracing, using the approaches developed for HIV. Many of their doctors and nurses have been seconded to medical teams dedicated to providing care for people with COVID-19.
“Many AIDS centres across the country have repurposed their laboratories to also diagnose coronavirus, but provision of quality medical care for people living with HIV continues,” said Natalia Ladnaia, Senior Researcher at the Central Research Institute of Epidemiology of Rospotrebnadzor, Russian Federal AIDS Centre.
In order to ensure the continuity of HIV services, many AIDS centres are working closely with community organizations to provide online counselling, deliver antiretroviral therapy to people living with HIV to their homes and address mental health challenges, which have grown since the COVID-19 pandemic began. Community activists from Novosibirsk representing the Ostrov and Humanitarian Project nongovernmental organizations, in collaboration with the regional AIDS centre, are delivering antiretroviral medicines to people living with HIV who are not able to collect their medicine from the AIDS centre.
Even some HIV testing services are moving online. Owing to quarantine restrictions, mobile laboratories cannot travel, so the Humanitarian Project organized remote testing for key populations in Siberia. “We are working with representatives of key populations and the regional Ministry of Health,” said Denis Kamaldinov, the head the Humanitarian Project. The initiative is providing online support and counselling for people who are at risk of HIV. Since March 2020, online and telephone-based counselling related to HIV and the health of people who use drugs and other key populations has intensified. “Our counsellors are communicating with clients by phone, social media and instant messaging,” he added. In order to receive an HIV self-test kit, a client only needs to complete an online application on the organization’s website.
The Deputy Prime Minister of the Russian Federation, Tatiana Golikova, has called for nongovernmental organizations working with key populations and people living with HIV to be supported during the COVID-19 pandemic. The regions that have introduced COVID-19 lockdowns have been advised to allow nongovernmental organizations working on social services, including the AIDS response, to continue their work, with their employees having freedom of movement and being supplied with personal protective equipment.
"The unique value of the AIDS centres is demonstrated by their quick and professional response to COVID-19. We are seeing this leadership coming from AIDS centres across the region. With the strategic involvement of AIDS centres and their partners, the COVID-19 response in our region will be more effective and the risk of progress in the AIDS response being rolled back will be mitigated,” said Alexander Goliusov, Director, a.i., of the UNAIDS Regional Support Team for Eastern Europe and Central Asia.
Our work
Region/country
Related


Press Release
World leaders unite in call for a people’s vaccine against COVID-19
19 May 2020 19 May 2020More than 140 world leaders, experts and elders have made an unprecedented call for guarantees that COVID-19 vaccines, diagnostics, tests and treatments will be provided free of charge to everyone, everywhere
GENEVA, 14 MAY 2020—More than 140 world leaders and experts, including the President of South Africa and Chair of the African Union, Cyril Ramaphosa, the Prime Minister of Pakistan, Imran Khan, the President of the Republic of Senegal, Macky Sall and the President of the Republic of Ghana, Nana Addo Dankwa Akufo-Addo have signed an open letter calling on all governments to unite behind a people’s vaccine against COVID-19. The call was made just days before health ministers meet virtually for the World Health Assembly on 18 May.
The letter, which marks the most ambitious position yet set out by world leaders on a COVID-19 vaccine, demands that all vaccines, treatments and tests be patent-free, mass produced, distributed fairly and made available to all people, in all countries, free of charge.
Other signatories include the former President of Liberia, Ellen Johnson Sirleaf, the former Prime Minister of the United Kingdom, Gordon Brown, the former President of Mexico, Ernesto Zedillo, the former United Nations Development Programme Administrator and former Prime Minister of New Zealand, Helen Clark.
They join notable economists, health advocates and others, from the Chair of the Elders and the former President of Ireland, Mary Robinson, Nobel Laureate, Joseph Stiglitz, to Moussa Faki, Chairperson of the African Union Commission, Dr John Nkengasong, Director of African Centres for Disease Control and Prevention, and Dainius Puras, the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health.
“Billions of people today await a vaccine that is our best hope of ending this pandemic,” said Cyril Ramaphosa, President of South Africa. “As the countries of Africa, we are resolute that the COVID-19 vaccine must be patent-free, rapidly made and distributed, and free for all. All the science must be shared between governments. Nobody should be pushed to the back of the vaccine queue because of where they live or what they earn.”
“We must work together to beat this virus. We must pool all the knowledge, experience and resources at our disposal for the good of all humanity,” said Imran Khan, Prime Minister of Pakistan. “No leader can rest easy until every individual in every nation is able to rapidly access a vaccine free of charge.”
The letter, coordinated by UNAIDS and Oxfam, warns that the world cannot afford monopolies and competition to stand in the way of the universal need to save lives.
“This is an unprecedented crisis and it requires an unprecedented response,” said former President of Liberia, Ellen Johnson Sirleaf. “Learning the lessons from the fight against Ebola, governments must remove all the barriers to the development and rapid roll out of vaccines and treatments. No interest is more important than the universal need to save lives"
The leaders recognize that progress is being made and that many countries and international organizations are cooperating multilaterally on research and development, funding and access, including the welcome US$ 8 billion pledged on 4 May at the European Union’s international pledging marathon.
However, as many countries and companies are proceeding with unprecedented speed to develop an effective vaccine, the leaders are calling for concrete commitments to ensure that it is made affordable and available to all in the quickest possible time. These include:
- A mandatory worldwide pooling of patents and sharing of all COVID-19-related knowledge, data and technologies in order to ensure that any nation can produce or buy affordable doses of vaccines, treatments and tests.
- The rapid establishment of an equitable global manufacturing and distribution plan for all vaccines, treatments and tests that is fully funded by rich nations and which guarantees transparent “at true cost prices” and supplies in accordance with need rather than the ability to pay.
- This would include urgent action to massively increase manufacturing capacity to produce the vaccines in sufficient quantities and train and recruit millions of health workers to distribute them.
- A guarantee that COVID-19 vaccines, treatments and tests are provided free of charge to everyone, everywhere, with priority given to frontline workers, vulnerable people and poor countries with the least capacity to save lives.
“Faced with this crisis, we cannot carry on business as usual. The health of each of us depends on the health of all of us,” said Helen Clark, former Prime Minister of New Zealand. “The COVID-19 vaccine must not belong to anyone and must be free for everyone. Diplomatic platitudes are not enough—we need legal guarantees, and we need them now.”
“Market solutions are not optimal to fight a pandemic,” said Nelson Barbosa, former Finance Minister of Brazil. “A public health care system, including free vaccination and treatment when that becomes available, is essential to deal with the problem, as shown by the Brazilian experience with compulsory licensing of antiretroviral drugs in the case of HIV.”
Uniting behind a people’s vaccine against COVID-19—open letter and full list of signatories
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
Oxfam
Anna Ratcliff
tel. +44 7796 993288
anna.ratcliff@oxfam.org
Oxfam
Annie Theriault
tel. +51 936 307 990
annie.theriault@oxfam.org
The People's Vaccine website
A COVID-19 vaccine for all


Feature Story
COVID-19 in prisons—a ticking time bomb
13 May 2020
13 May 2020 13 May 2020With more than 11 million people in custody worldwide, and 30 million people entering and leaving detention every year, the threat of COVID-19 for people in prisons is very real. In the vast majority of the world’s overcrowded and underfunded prisons and detention centres, physical distancing is simply not an option. In situations where close confinement, shared facilities and spaces and poor hygiene are commonplace, inmates and prison staff are living in constant fear of the ticking COVID-19 time bomb.
“A health response to COVID-19 in prisons is not enough. This unprecedented global emergency demands a response based on human rights,” said Winnie Byanyima, Executive Director of UNAIDS. “Countries must ensure not only the security but also the health, safety and human dignity of people deprived of their liberty at all times, irrespective of any state of emergency.”
UNAIDS, the Office of the United Nations High Commissioner for Human Rights, the World Health Organization and United Nations Office on Drugs and Crime are calling on leaders to make detention a last resort, to close drug rehabilitation detention centres and to decriminalize sex work, same-sex sexual relations and drug use. They are urging countries to release the people who can be released and to consider people at risk of COVID-19, such as older people and people with pre-existing health conditions. Other people, including people sentenced for minor, non-violent offences, pregnant women, women who are breastfeeding and children, should also be considered for release.
As reports of terrified inmates sewing makeshift masks continue to emerge, countries are starting to take action. The Government of Ethiopia, for example, has released more than 30 000 prisoners and has heightened sanitation measures. Indonesia is releasing more than 50 000 people, including 15 000 people incarcerated for drug-related offences. The Islamic Republic of Iran is releasing 40% of its total prison population,100 000 people, while Chile is set to release around 50 000 people.

















