

Press Statement
UNODC, WHO, UNAIDS and OHCHR joint statement on COVID-19 in prisons and other closed settings*
13 May 2020 13 May 2020Signed by Ghada Fathi Waly, Executive Director, UNODC; Tedros Adhanom Ghebreyesus, Director-General, WHO; Winnie Byanyima, Executive Director, UNAIDS; Michelle Bachelet, United Nations High Commissioner for Human Rights. — * We thank UNDP for their contributions to this statement.
We, the leaders of global health, human rights and development institutions, come together to urgently draw the attention of political leaders to the heightened vulnerability of prisoners and other people deprived of liberty to the COVID-19 pandemic, and urge them to take all appropriate public health measures in respect of this vulnerable population that is part of our communities.
Acknowledging that the risk of introducing COVID-19 into prisons or other places of detention varies from country to country, we emphasize the need to minimize the occurrence of the disease in these settings and to guarantee that adequate preventive measures are in place to ensure a gender-responsive approach and preventing large outbreaks of COVID-19. We equally emphasize the need to establish an up-to-date coordination system that brings together health and justice sectors, keeps prison staff well-informed and guarantees that all human rights in these settings are respected.
Reduce overcrowding
In the light of overcrowding in many places of detention, which undermines hygiene, health, safety and human dignity, a health response to COVID-19 in closed settings alone is insufficient. Overcrowding constitutes an insurmountable obstacle for preventing, preparing for or responding to COVID-19.
We urge political leaders to consider limiting the deprivation of liberty, including pretrial detention, to a measure of last resort, particularly in the case of overcrowding, and to enhance efforts to resort to non-custodial measures. These efforts should encompass release mechanisms for people at particular risk of COVID-19, such as older people and people with pre-existing health conditions, as well as other people who could be released without compromising public safety, such as those sentenced for minor, non-violent offences, with specific consideration given to women and children.
A swift and firm response aimed at ensuring healthy and safe custody, and reducing overcrowding, is essential to mitigate the risk of COVID-19 entering and spreading in prisons and other places of deprivation of liberty. Increasing cleanliness and hygiene in places of deprivation of liberty is paramount in order to prevent the entry of, or to limit the spread of, the virus.
Compulsory detention and rehabilitation centres, where people suspected of using drugs or engaging in sex work are detained, without due process, in the name of treatment or rehabilitation should be closed. There is no evidence that such centres are effective in the treatment of drug dependence or rehabilitation of people and the detention of people in such facilities raises human rights issues and threatens the health of detainees, increasing the risks of COVID-19 outbreaks.
Ensuring health, safety and human dignity
All states are required to ensure not only the security, but also the health, safety and human dignity, of people deprived of their liberty and of people working in places of detention at all times. This obligation applies irrespective of any state of emergency.
Decent living and working conditions as well as access to necessary health services free of charge form intrinsic elements of this obligation. There must be no discrimination on the basis of the legal or any other status of people deprived of their liberty. Health care in prisons, including preventive, supportive and curative care, should be of the highest quality possible, at least equivalent to that provided in the community. Priority responses to COVID-19 currently implemented in the community, such as hand hygiene and physical distancing, are often severely restricted or not possible in closed settings.
Ensuring access to continued health services
Prison populations have an overrepresentation of people with substance use disorders, HIV, tuberculosis (TB) and hepatitis B and C compared to the general population. The rate of infection of diseases in such a confined population is also higher than among the general population. Beyond the normal infectivity of the COVID-19 pandemic, people with substance use disorders, HIV, hepatitis and TB may be at increased risk of complications from COVID-19.
To ensure that the benefits of treatments started before or during imprisonment are not lost, provisions must be made, in close collaboration with public health authorities, to allow people to continue their treatments without interruption at all stages of detention and upon release. Countries should embrace a health systems approach, where prisons are not separated from the continuity-of-care pathway but integrated with community health services.
Enhancing prevention and control measures in closed settings as well as increasing access to quality health services, including uninterrupted access to the prevention and treatment of HIV, TB, hepatitis and opioid dependence, are therefore required. Authorities must ensure uninterrupted access and flow of quality health commodities to prisons and other places of detention. Staff, health-care professionals and service providers working in closed settings should be recognized as a crucial workforce for responding to the COVID-19 pandemic and receive appropriate personal protective equipment and support as necessary.
Respect human rights
In their responses to COVID-19 in closed settings, states must respect the human rights of people deprived of their liberty. Restrictions that may be imposed must be necessary, evidence-informed, proportionate (i.e. the least restrictive option) and non-arbitrary. The disruptive impact of such measures should be actively mitigated, such as through enhanced access to telephones or digital communications if visits are limited. Certain fundamental rights of people deprived of their liberty and corresponding safeguards, including the right to legal representation, as well as the access of external inspection bodies to places of deprivation of liberty, must continue to be fully respected.
Adhere to United Nations rules and guidance
We urge political leaders to ensure that COVID-19 preparedness and responses in closed settings are identified and implemented in line with fundamental human rights, are guided by World Health Organization (WHO) guidance and recommendations and never amount to torture and other cruel, inhuman or degrading treatment or punishment. In prisons, any intervention should comply with the United Nations Standard Minimum Rules for the Treatment of Prisoners (the Nelson Mandela Rules).
People deprived of their liberty exhibiting symptoms of COVID-19 or who have tested positive should be monitored and treated in line with the most recent WHO guidelines and recommendations. Prisons and other places of detention must be part of national COVID-19 plans with dedicated participation of affected populations. All cases of COVID-19 in closed settings should be notified to responsible public health authorities, who will then report to national and international authorities.
In line with our mandates, we remain available to provide support in the rapid deployment of the recommendations outlined above.
This document is available in Arabic, Chinese, French, Portuguese, Russian and Spanish.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Press centre
Download the printable version (PDF)


Press Release
The cost of inaction: COVID-19-related service disruptions could cause hundreds of thousands of extra deaths from HIV
11 May 2020 11 May 2020Gains made in preventing mother-to-child transmission of HIV could be reversed, with new HIV infections among children up by as much as 162%
GENEVA, 11 May 2020—A modelling group convened by the World Health Organization and UNAIDS has estimated that if efforts are not made to mitigate and overcome interruptions in health services and supplies during the COVID-19 pandemic, a six-month disruption of antiretroviral therapy could lead to more than 500 000 extra deaths from AIDS-related illnesses, including from tuberculosis, in sub-Saharan Africa in 2020–2021. In 2018, an estimated 470 000 people died of AIDS-related deaths in the region.
There are many different reasons that could cause services to be interrupted—this modelling exercise makes it clear that communities and partners need to take action now as the impact of a six-month disruption of antiretroviral therapy could effectively set the clock on AIDS-related deaths back to 2008, when more than 950 000 AIDS-related deaths were observed in the region. And people would continue to die from the disruption in large numbers for at least another five years, with an annual average excess in deaths of 40% over the next half a decade. In addition, HIV service disruptions could also have some impact on HIV incidence in the next year.
“The terrible prospect of half a million more people in Africa dying of AIDS-related illnesses is like stepping back into history,” said Dr Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization.
“We must read this as a wake-up call to countries to identify ways to sustain all vital health services. For HIV, some countries are already taking important steps, for example ensuring that people can collect bulk packs of treatment, and other essential commodities, including self-testing kits, from drop-off points, which relieves pressure on health services and the health workforce. We must also ensure that global supplies of tests and treatments continue to flow to the countries that need them,” added Dr Tedros.
In sub-Saharan Africa, an estimated 25.7 million people were living with HIV and 16.4 million (64%) were taking antiretroviral therapy in 2018. Those people now risk having their treatment interrupted because HIV services are closed or are unable to supply antiretroviral therapy because of disruptions to the supply chain or because services simply become overwhelmed due to competing needs to support the COVID-19 response.
“The COVID-19 pandemic must not be an excuse to divert investment from HIV,” said Winnie Byanyima, Executive Director of UNAIDS. “There is a risk that the hard-earned gains of the AIDS response will be sacrificed to the fight against COVID-19, but the right to health means that no one disease should be fought at the expense of the other.”
When treatment is adhered to, a person’s HIV viral load drops to an undetectable level, keeping that person healthy and preventing onward transmission of the virus. When a person is unable to take antiretroviral therapy regularly, the viral load increases, impacting the person’s health, which can ultimately lead to death. Even relatively short-term interruptions to treatment can have a significant negative impact on a person’s health and potential to transmit HIV.
This research brought together five teams of modellers using different mathematical models to analyse the effects of various possible disruptions to HIV testing, prevention and treatment services caused by COVID-19.
Each model looked at the potential impact of treatment disruptions of three months or six months on AIDS mortality and HIV incidence in sub-Saharan Africa. In the six-month disruption scenario, estimates of excess AIDS-related deaths in one year ranged from 471 000 to 673 000, making it inevitable that the world will miss the global 2020 target of fewer than 500 000 AIDS-related deaths worldwide.
Shorter disruptions of three months would see a reduced but still significant impact on HIV deaths. More sporadic interruptions of antiretroviral therapy supply would lead to sporadic adherence to treatment, leading to the spread of HIV drug resistance, with long-term consequences for future treatment success in the region.
Disrupted services could also reverse gains made in preventing mother-to-child transmission of HIV. Since 2010, new HIV infections among children in sub-Saharan Africa have declined by 43%, from 250 000 in 2010 to 140 000 in 2018, owing to the high coverage of HIV services for mothers and their children in the region. Curtailment of these services by COVID-19 for six months could see new child HIV infections rise drastically, by as much as 83% in Mozambique, 106% in Zimbabwe, 139% in Uganda and 162% in Malawi.
Other significant effects of the COVID-19 pandemic on the AIDS response in sub-Saharan Africa that could lead to additional mortality include reduced quality clinical care owing to health facilities becoming overstretched and a suspension of viral load testing, reduced adherence counselling and drug regimen switches. Each model also considered the extent to which a disruption to prevention services, including suspension of voluntary medical male circumcision, interruption of condom availability and suspension of HIV testing, would impact HIV incidence in the region.
The research highlights the need for urgent efforts to ensure the continuity of HIV prevention and treatment services in order to avert excess HIV-related deaths and to prevent increases in HIV incidence during the COVID-19 pandemic. It will be important for countries to prioritize shoring up supply chains and ensuring that people already on treatment are able to stay on treatment, including by adopting or reinforcing policies such as multimonth dispensing of antiretroviral therapy in order to reduce requirements to access health-care facilities for routine maintenance, reducing the burden on overwhelmed health-care systems.
“Every death is a tragedy,” added Ms Byanyima. “We cannot sit by and allow hundreds of thousands of people, many of them young, to die needless deaths. I urge governments to ensure that every man, women and child living with HIV gets regular supplies of antiretroviral therapy—something that’s literally a life-saver.”
Sources:
Jewell B, Mudimu E, Stover J, et al for the HIV Modelling consortium, Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple models. Pre-print, https://doi.org/10.6084/m9.figshare.12279914.v1, https://doi.org/10.6084/m9.figshare.12279932.v1.
Hogan B, Jewell B, Sherrard-Smith E, et al. The potential impact of the COVID-19 epidemic on HIV, TB and malaria in low- and middle-income countries. Imperial College London (01-05-2020). doi: https://doi.org/10.25561/78670.
Stover J, Chagoma N, Taramusi I, et al. Estimation of the Potential Impact of COVID-19 Responses on the HIV Epidemic: Analysis using the Goals Model. Pre-print. medRxiv 2020.05.04.20090399; doi: https://doi.org/10.1101/2020.05.04.20090399
WHO
The World Health Organization provides global leadership in public health within the United Nations system. Founded in 1948, WHO works with 194 Member States, across six regions and from more than 150 offices, to promote health, keep the world safe and serve the vulnerable. Our goal for 2019-2023 is to ensure that a billion more people have universal health coverage, to protect a billion more people from health emergencies, and provide a further billion people with better health and wellbeing.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS Mediatel. tel. +41 22 791 4237
communications@unaids.org
WHO Media
Tarik Jašarević
tel. tel. +41 79 367 6214
jasarevict@who.int
WHO Media
Sarah Russell
tel. tel. +41 79 598 6823
russellsa@who.int
Press centre
Download the printable version (PDF)


Feature Story
Sex workers in Bangladesh: building resilience during the COVID-19 pandemic
13 May 2020
13 May 2020 13 May 2020Shahnaz Khatun (not her real name), a former sex worker now running a small clothing business in Dhaka, Bangladesh, found herself in difficulties when the country went into lockdown. Before the COVID-19 outbreak, the areas where she used to work were crowded, but now they are quiet. Ms Khatun is self-isolating in response to the government’s call, but she is unable to provide for herself and her family. “My business is now out of action due to the restrictions on movement. I have some underlying health conditions and I spent all my money on buying medicines,” she said.
As a result of the COVID-19 pandemic, sex workers in Bangladesh, like other informal sector workers, are experiencing hardship and a loss of income. With the limited support that some of them get, they can barely feed themselves and their children. Only a few of them have savings to fall back on and little access to services that could bring some relief. Conditions are more vulnerable for street-based sex workers, as most of them are homeless.
However, sex workers in Bangladesh are organizing themselves, establishing support networks to help their peers. The Bangladesh Sex Workers Network, a nongovernment organization working for the rights of sex workers, mobilized financial aid for more than 2100 sex workers across the country that was distributed through the active engagement of 26 community-based organizations. “Many sex workers have chosen this profession for the sake of their families or children, to provide them with food and a livelihood. Today, sex workers’ families are passing their days helplessly with no money in their pocket,” explains Ms Kajol, President of the Sex Workers Network of Bangladesh.
Ms Khatun received 10 000 Bangladeshi taka, equivalent to US$ 120, through the Bangladesh Sex Workers Network. “With this, I also bought food for another 30 sex workers. I am also arranging for delivery of masks, soap and food to other sex workers in my area and am teaching them about hand washing techniques, maintaining personal hygiene and social distance maintenance,” she said.
Ankhi Akhter (not her real name), who works in a brothel in Tangail, gives support for mental health issues to her peers and encourages regular communication among sex workers in order to cope with stress and to exchange thoughts. “The local governmental authority and a number of nongovernmental organizations, as well as private entities, have already helped us with food and a limited amount of money,” she said. “However, these will not be sufficient if the situation continues.”
As a result of Ms Akhter’s efforts, the Dhaka District Council Office and the Member of Parliament representing the district donated food to the brothel and distributed it among a network of 500 sex workers. The Society for Social Service, a local nongovernmental organization, offered cash payments to more than 400 sex workers and landlords postponed utility bills, such as rent, electricity and water. Most of the sex workers in the brothel received masks, soap and hand sanitizer from the brothel and volunteer organizations.
Sweety Begum (not her real name) is the leader of a community-based organization that supports street-based sex workers in Rajshahi. She relies on her husband's limited income for their living expenses and is helping other sex workers with the small amount of financial help she receives. “Street-based sex workers outside Dhaka are getting less help than those in Dhaka and they are scared to collect aid because of stigma and discrimination,” she said.
“Eleven brothels in Bangladesh have received food and some financial support from government organizations: however, this is not enough. In some areas, relief has been provided only to those who have a national identity card and, unfortunately, not all sex workers have this,” says Saima Khan, UNAIDS Country Manager for Bangladesh.
UNAIDS and the United Nations Children’s Fund have been supporting the network of sex workers to develop income-generating schemes so they can compensate for the loss of income caused by COVID-19. Also, through the network of sex workers and in collaboration with the Bangladesh Country Coordinating Mechanism, UNAIDS has supported 23 community-based organizations of sex workers to procure protective commodities such as soap and masks during the initial stages of the response to COVID-19. Advocacy with organizations to make access to aid easier for sex workers is also ongoing.
“The Sex Workers Network of Bangladesh, through collective efforts, will continue to work hand in hand, so that sex workers can fight back against any difficult situation they face together, leaving no one behind,” said Ms Kajol.
Our work
Region/country






Feature Story
HIV testing and support for homeless people in Belarus
11 May 2020
11 May 2020 11 May 2020Homeless people have difficulty accessing health-care services at the best of times, but the COVID-19 pandemic has curtailed access even more. Stigma and discrimination and the conditions they live in make homeless people particularly vulnerable not only to COVID-19 but also tuberculosis, HIV, hepatitis and other diseases.
“Before the COVID-19 pandemic there were about 11 shelters in Minsk where people could get clean clothes, wash themselves, have food and stay for a night. Now only three of them remain open,” said Karina Radchenko, a volunteer from Street Medicine, the country's first volunteer network to treat the homeless. “We know that some of them are living with HIV, but because they don’t have proper identification and residence registration they can’t get free treatment. This is why we need to keep providing support to the homeless, especially now.”
Launched by Street Medicine, UNAIDS, the Positive Movement—a Minsk-based nongovernmental organization that provides HIV services—and the Ministry of Health of Belarus, a new initiative is providing HIV testing and support to the homeless during the COVID-19 pandemic.
Working on the streets, the volunteers distribute condoms, hygiene packs and over-the-counter medicines and provide HIV testing and counselling together with first aid, such as wound treatment and bandage application. The first phase of the initiative will see at least 200 homeless people in Minsk and beyond being tested for HIV and will collect information on their HIV prevention needs and the barriers they face in accessing HIV treatment and other health services.
“Homeless people very often don’t have identification, and this complicates a formal recognition of their HIV status and their access to HIV treatment,” said Vera Ilyenkova, the UNAIDS Country Manager for Belarus. “One of the goals of this initiative is to help people who test positive for HIV to get connected to health facilities so they can get treatment and proper documents from the authorities.”
Our work
Region/country
Related


Feature Story
Dealing with COVID-19 in Cameroon
11 May 2020
11 May 2020 11 May 2020Q&A with UNAIDS Country Director Savina Ammassari
Savina Ammassari has been the UNAIDS Country Director for Cameroon since 2018. Before that, she worked for UNAIDS in India, Myanmar and Cambodia as a Strategic Information Adviser. She has supported initiatives promoting sustainable development, equity and human rights in more than 20 countries.
Because she has lived and worked in so many countries and speaks many languages, she considers herself quick to adapt, but COVID-19 has definitely tested her.
Savina, did you feel like COVID-19 was a tsunami coming your way?
Yes, indeed, I saw the tsunami coming. I’d followed the COVID-19 outbreak in China, the rapidly unfolding epidemic in Italy, my home country, which already has claimed more than 24 000 lives. I was acutely aware that many countries in sub-Saharan Africa, including Cameroon, would be ill-prepared to address the devastating health and economic impacts of COVID-19, where fragile health systems and chronic poverty represent significant challenges for government, community and United Nations system responses to the pandemic.
The realities of the crisis enveloping the world were starkly brought home to me when my brother-in-law, working as a surgeon in Brescia, the epicentre of the Italian epidemic, developed severe COVID-19 symptoms, leading to bilateral pneumonia. Fortunately, he was ventilated and received experimental treatments. His life has been saved. But I know this will not be the case for everyone, especially in countries with weaker health-care systems.
Cameroon is now the COVID-19 epicentre in western and central Africa. The first cases were detected at the airport of the capital, Yaoundé. Additional cases were soon recorded in Douala, the largest city of the country. Despite early measures taken by the Government to isolate initial cases, testing and contact tracing, community transmission has taken hold. Limited access to testing services makes it difficult to know the extent of transmission.
The Cameroon response has faced significant constraints, not least the capacity to scale up testing and expand contact tracing and the provision of intensive care unit/ventilation support for the seriously ill, as well as adequate personal protective equipment for medical staff. The rapid implementation of community education programmes, emphasizing hand hygiene and social distancing, is an ongoing challenge, especially in poor, often overcrowded, urban areas.
How did Cameroon prepare? In Cameroon, there initially was a sense of optimism that, somehow, Africa, unlike other regions, would manage to avoid the catastrophic consequences of the pandemic. There was little awareness that Cameroon was most likely just a matter of a few weeks behind.
Today, Cameroon is the most affected country in the region and second in sub-Saharan Africa, with a quickly rising rate of infections. The scarcity of test kits obviously hides the real number of infections. Counting individual infections, recoveries and fatalities does not provide the real picture. UNAIDS advocated for a modelling of the epidemic in order to enable quantification of health-care needs and procurement.
As the first COVID-19 cases were detected in Yaoundé, a small number of health-sector officials gathered with the Minister of Health to discuss and plan epidemic containment and impact mitigation measures. I was one of the United Nations officials requested to be part of the group, given UNAIDS’ experience in epidemic management. I underscored the need to build on existing systems and make use of the community-driven efforts of the national AIDS response. I advocated for frontloading investments in communication and community mobilization to prevent COVID-19 infections, using a multisectoral approach.
The multisectoral response fell into place through the direct involvement of the United Nations Resident Coordinator (UNRC) with my support. I facilitated the UNRC’s efforts to connect the Minister of Health with development partners in weekly teleconference calls. Partners were ready to assist but lacked information on the most immediate needs.
UNAIDS has supported the Ministry of Health to model the COVID-19 epidemic to better understand and quantify needs. This has been done through teleconferencing, with the participation of various technical and financial partners. It has helped with the prioritization of needs and the quantification and costing of urgently required supplies and equipment. Partners were ready to support this effort, but required not only a modelled, costed national COVID-19 response plan but also a well-articulated procurement schedule based on the plan. UNAIDS has also successfully advocated for the establishment of a strategic information working group to analyse more in-depth data from surveillance, model the epidemic, and monitor and evaluate the COVID-19 response.
Communicating is indeed key. But how do you deal with things as basic as the lack of running water in many sub-Saharan African countries, making handwashing difficult. How are people coping with this and other measures, such as physical distancing?
This is indeed a major challenge in Cameroon as there is a lack of consistent water supply in many urban and rural communities. The use of hand sanitizers is not an affordable option for most people and locally produced product is not necessarily quality assured and safe for use.
Similarly, physical distancing and self-isolation are remote, often unrealistic options for communities where large numbers of people, as a rule, share common spaces in their home and community environments. The government has put in place a series of strict measures to contain the spread of COVID-19 (closing schools and educational or training institutions, banning gatherings of all kinds, imposing the use of face masks on public transport), although a comprehensive lockdown has not been promulgated to date. There are legitimate concerns on how a full lockdown could affect the majority of people, as more than 80% of the population work in the informal sector and live hand-to-mouth. Yet, from a public health perspective, lockdowns are a must. Balancing concerns is a major challenge.
Savina, you have never shied away from challenges. Would you say this is the biggest challenge you have faced, and why?
Yes, this crisis is unprecedented, unpredictable. I’m concerned at how the COVID-19 pandemic will affect not only our staff and their dependents but also people living with HIV, who need to continue accessing antiretroviral therapy and services, and people who are already stigmatized, vulnerable and socially and economically marginalized.
We have already witnessed a worrisome rise in stigma and discrimination against members of key populations in Cameroon and are making sure that the UNCT and partners keep human rights issues high on the agenda.
Our work is already challenging in normal times as Cameroon is facing enormous development and humanitarian hurdles. Already, Cameroon’s humanitarian crises on three fronts are not getting enough international attention. It’s the least funded humanitarian crisis worldwide. The COVID-19 epidemic multiplies these challenges several times over.
UNAIDS is mobilizing communities and networks in COVID-19 prevention work and making sure that civil society is adequately consulted and involved in the national response to the new virus.
How do you unwind in the evening? How do you recharge your batteries?
I’m afraid I don’t give enough time to relaxing, as I work around the clock, which isn’t good. Perhaps one of the challenges of COVID-19 is to take up new interests outside of work, that can be sustained and enjoyable well into the future.
What are the lessons learned? Will you do things differently from now on?
I’ve learned once again that unity makes force. In unpreceded emergencies like the current one, where no one has the answer or a magic bullet, everyone’s competence and experience is needed. Connecting people, bringing in resources, getting a transparent exchange—all this is paying off. It requires strong leadership and a cohesive team effort.
Our work
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025



Feature Story
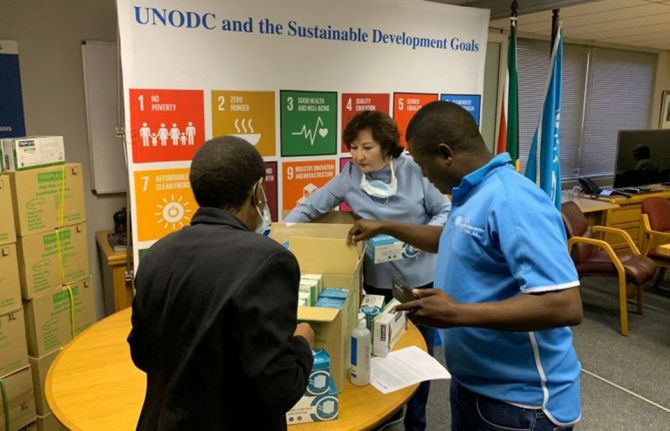
United Nations agencies coordinate their COVID-19 response in South Africa
12 May 2020
12 May 2020 12 May 2020United Nations entities in South Africa, including UNAIDS, are working closely together to support government and community responses to the COVID-19 pandemic. The United Nations in South Africa has jointly engaged with civil society, the private sector and key affected communities, including people living with HIV and tuberculosis, to rapidly respond to the impact of a national lockdown that commenced on 26 March.
Using the World Health Organization eight-pillar approach, the United Nations in South Africa has developed a multisectoral plan centred on the immediate health and other needs of people, including access to medicines, HIV prevention and testing services, food security, education, social protection and community resilience.
On 30 April, the United Nations in South Africa launched an emergency flash appeal for US$ 136 million to support close to 10 million people in need. The appeal will help fund the civil society response and ensure that the needs of key populations and vulnerable communities are met in the response to COVID-19, including continued health support to people living with HIV, migrants and refugees, women and children affected by violence and communities facing shortages of food and other essentials.
UNAIDS has worked with partners to coordinate the United Nations in South Africa plan, providing support to strategic information, community engagement and communication. Funds already available to the United Nations Joint Team on HIV/AIDS are being reprogrammed to ensure that civil society, people living with HIV, key populations and vulnerable communities continue to be supported in the AIDS response while also addressing new challenges from COVID-19.
United Nations staff, including UNAIDS staff based in provinces with a high HIV burden, are working in the national and provincial COVID-19 command centres and supporting community health workers actively engaged in screening, contact tracing and voluntary testing. South Africa has massively scaled up screening for COVID-19.
Supporting community innovation
The United Nations has actively engaged with civil society organizations through sector networks, some of which have been established to coordinate responses to the pandemic, such as the C19 People’s Coalition and the COVID-19 Front, and long-standing networks, including the South African National AIDS Council (SANAC) Civil Society Forum and the National Economic Development Council Community Constituency. Their plans include a strong emphasis on advocacy, communication and social mobilization around issues such as medical care, shortages of food and fresh water, crowded housing conditions, homelessness and loss of income. The United Nations Country Team is providing technical support to civil society and resource mobilization through its emergency flash appeal.
UNAIDS has also supported organizations representing people living with HIV to survey and document the needs and challenges of people living with HIV in accessing essential health and social services, antiretroviral therapy and safety and hygiene services committed by the government. The survey results will inform a dialogue led by people living with HIV to find joint solutions.
Working with the government and other partners
Under the leadership of the United Nations Resident Coordinator in South Africa, Nardos Bekele-Thomas, the United Nations in South Africa is fully supporting the all-government, all-society COVID-19 response led by the National Command Council, chaired by the President, with a cutting-edge Ministerial Advisory Council that provides the science and evidence for decision-making.
The United Nations has jointly consulted the government, including the Department of Health and the Department of Social Development, to explore response needs, including support to the National Solidary Fund set up by the President for resource mobilization. The United Nations also briefed the diplomatic corps, the business sector, private foundations and philanthropies on how the United Nations is responding to support the government, civil society and communities. Consultations were also held with the World Bank, which is currently developing a post COVID-19 strategy and possible support to the national response.
The UNAIDS Country Director for South Africa, Mbulawa Mugabe, emphasized the importance of using lessons from the AIDS epidemic to put people at the centre of the COVID-19 response and encourage communities to identify issues and develop solutions. “We need to make sure that we act with purpose and speed,” he said. “Communities have mobilized themselves and are determined that people who need services have access to them. We remain concerned that COVID-19 may impact differently on the 5 million people in South Africa who are living with HIV and on treatment and the 2.5 million people who are not currently receiving antiretroviral therapy. It is important to protect the progress in the AIDS response to date and continue achieving the HIV prevention and treatment targets for 2020.”
The Joint Team on HIV/AIDS in South Africa is working with the Department of Health, primary recipients of the Global Fund to Fight AIDS, Tuberculosis and Malaria and the United States President’s Emergency Plan for AIDS Relief in an effort to safeguard access to HIV services and promote multimonth dispensing of antiretroviral therapy.
UNAIDS is working with the United Nations Office on Drugs and Crime, the Department of Social Development, SANAC and other partners to address disruptions for homeless people, including those who use drugs, so they can access essential services, including antiretroviral therapy, replacement needles and syringes and methadone, even after they were relocated to emergency shelters. The Office of the United Nations High Commissioner for Human Right is monitoring the impact of the lockdown regulations and enforcement procedures on marginalized people and key populations and is advocating to end stigma and prevent punitive measures. The social protection cluster in the United Nations team is working with government and civil society to address humanitarian challenges.
The World Health Organization and UNAIDS are working with the Department of Health and SANAC to develop communication materials directed at communities, including podcasts to be made available through WhatsApp and community radio stations.
Our work
Region/country


Feature Story
Combatting COVID-19 discrimination in Jamaica
08 May 2020
08 May 2020 08 May 2020Some Jamaicans have responded to the COVID-19 outbreak in extreme ways. Family members of one of the first confirmed cases received death threats, and nurses have reported being barred from public transport. Some people have given the health authorities wrong addresses to avoid the stigma that a home visit would attract.
UNAIDS Jamaica and civil society organizations serving people living with HIV have joined the national discourse to share a key lesson learned from HIV: that stigma and discrimination are barriers to an effective response.
Two-thirds of Jamaicans would not purchase vegetables from someone they knew to be living with HIV, according to the 2017 Knowledge Attitude and Behaviour Study. The effect of such widespread prejudice is seen in the island’s treatment outcomes. According to government estimates, while an estimated 84% of people living with HIV were aware of their status in 2018, less than half (47%) were on treatment
For Jumoke Patrick, Executive Director of the Jamaica Network of Seropositives, there are clear parallels between people’s reactions to the novel coronavirus and HIV.
“People living with HIV feel they need to stay away from people and from accessing services. They feel they need to reduce and limit their lives because of how people treat them. We have some of the same treatment meted out to people positive with, or suspected of having, coronavirus. When there’s fear we respond in a defensive way,” Mr Patrick explained in a webinar hosted by UNAIDS Jamaica.
Community organizations have reported that some COVID-19 stigma has even been directed to people living with HIV. UNAIDS Jamaica has been working to raise awareness among policymakers and through the news media about the importance of building trust with affected people while combatting stigma and discrimination among the wider population.
“Just as with HIV, success in combatting COVID-19 absolutely depends on people’s willingness to get tested and access care. Verbal abuse, violence and intimidation will only chase people away from services,” said Manoela Manova, UNAIDS Country Director for Jamaica.
The Jamaica Ministry of Health has launched an antidiscrimination campaign that includes stories of harassed COVID-19 patients in virtual press conferences.
“None of us are immune to the virus,” Christopher Tufton, the Jamaican Minister of Health, said at a recent press conference. “None of us must claim or think that we will exclusively escape and it is somebody else’s fault. We must treat each other in a way that almost assumes that tomorrow we are going to need the support from those who are so infected and impacted today. We really need to cut the hate and work together as a country and as communities, to overcome.”
Our work
Region/country

Press Release
UNAIDS urges countries to stay focused on HIV prevention during the COVID-19 pandemic
06 May 2020 06 May 2020Overstretched health systems, lockdowns, loss of livelihoods and fewer employment opportunities could increase unprotected sex, sexual violence and exploitation, transactional sex and sex work, leading to an increase in new HIV infections
GENEVA, 6 May 2020—Despite the global progress made in HIV prevention, with new HIV infections falling by 40% since the peak in 1997, hard-won gains are in danger of being reversed by the COVID-19 pandemic sweeping around the world.
In the light of the COVID-19 pandemic, UNAIDS is urging countries to remain steadfast in their HIV prevention efforts and ensure that people can continue to access the services they need to stay HIV-free, discrimination-free and violence-free and to be able to enjoy their sexual and reproductive health and rights.
“COVID-19 is impacting almost every country and community, but the global HIV epidemic hasn’t gone away,” said Winnie Byanyima, UNAIDS Executive Director. “People are still having sex. People are still using drugs. During the COVID-19 pandemic, everyone must be given the tools they need to be safe and to protect themselves from HIV. Human rights are a cornerstone of HIV prevention and must be a cornerstone of the COVID-19 response.”
Three new documents on HIV prevention published by UNAIDS and partners in the Global HIV Prevention Coalition look at how to maintain and prioritize HIV prevention services in the context of COVID-19. They look at the critical measures needed to keep the most vulnerable alive and healthy, including the measures required to prevent and address violence against women and children, to keep the supply of critical commodities available and to sustain the livelihoods of the world’s poorest.
The documents explain that the range of options to prevent HIV—condoms, both male and female, lubricants, sterile needles and syringes and opiate substitution therapy for people who inject drugs, pre-exposure prophylaxis and post-exposure prophylaxis and treatment as prevention—are just as valid now as ever. Innovative ways of getting HIV prevention commodities to the people who need them must be found—dispensing longer-term quantities of prevention supplies, allowing distribution centres to remain open during lockdowns and protecting community distribution points are but a few possibilities.
In addition to hampering HIV prevention and treatment services, UNAIDS is concerned that the COVID-19 epidemic may increase the vulnerability of people to HIV. The widespread loss of livelihoods and fewer employment opportunities could mean that transactional sex, sex work and sexual exploitation will increase, putting people at increased risk of contracting HIV unless they have the means to protect themselves.
As well as HIV prevention commodities, the sustained availability of services and support programmes for the prevention of HIV, prevention of gender-based violence and promotion of sexual and reproductive health and rights as essential services is critical. HIV counselling and testing services, the screening and treatment of sexually transmitted infections, continuity of access to sexual and reproductive health services, peer and other community outreach services, psychosocial support services, drop-in centres for key and vulnerable populations, comprehensive sexuality education and sexual violence protection are all vital to preserving the HIV prevention response. The lockdowns imposed during the COVID-19 response have resulted in alarming increases in reports of domestic and intimate partner violence against women and violence outside the home, necessitating urgent reinforcement of prevention, protection and support services for gender-based and sexual violence.
Since social distancing and lockdowns have all but stopped face-to-face service delivery, UNAIDS is urging the introduction of innovative means through which people can access services. Physical meetings can be made safer by using appointment systems that do not allow too many people in a facility at the same time, while holding meetings and education sessions virtually and the use of telephone hotlines and SMS services all have a role to play to both keep people safe from the new coronavirus and to allow them to continue getting the help they need to stay free from HIV. HIV self-testing is a safer way to carry out HIV testing that reduces contact with other people and reduces the service burden on health facilities.
Community organizations and networks have long been essential for the AIDS response, owing to the central role they play in raising awareness, providing information, dispelling myths and countering misinformation and service delivery for marginalized and vulnerable populations. Now more than ever, community-led actors should be supported to innovate, deliver and be recognized as essential service providers for both the HIV and COVID-19 responses.
Forty years in responding to HIV have provided valuable lessons, notably that the COVID-19 pandemic will not affect everyone equally and that the most marginalized, including key populations, will be the most affected. Across the three new documents, UNAIDS urges countries to take a human rights approach and prioritize the needs of the most marginalized populations during COVID-19, including maintaining critical HIV prevention services.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)


Feature Story
United Nations in South Africa launches US$ 136 million COVID-19 flash appeal
07 May 2020
07 May 2020 07 May 2020The United Nations agencies in South Africa have launched a joint flash appeal to support 9.9 million people to cope with the COVID-19 response.
The United Nations Country Team in South Africa, under the leadership of the Resident Coordinator, was joined for the launch of the appeal on 30 April by government ministers and others.
The Emergency Appeal on the Impact of COVID-19 in South Africa calls for US$ 136 million to support government efforts to reach vulnerable and marginalized communities to address the impact of COVID-19. It aims to raise funds for health, including HIV/tuberculosis, food security and nutrition, gender-based violence protection and response, education, water and sanitation, coordination and governance.
The United Nations Resident Coordinator, Nardos Bekele-Thomas, said, “Helping South Africa especially at this time makes development sense and it also makes business sense. We focus on the most vulnerable groups. They have potential to be producers and, with disposable income, they will become consumers, investors and productive assets for the economy,” she said.
The Minister of Health, Zwele Mkhize, welcomed the United Nations plan, which will complement national efforts and focus on the needs of vulnerable communities, including people living with HIV and tuberculosis, migrants and refugees, vulnerable women and children, key populations and millions affected by poverty, unemployment and the impact of national restrictions on trade and movement since 26 March. “We have various issues of inequality, unemployment, poverty and densely populated areas and chronic overcrowding in our metros, which are the most affected by COVID-19. We have already started to see local transmissions in these areas, which has given us cause for concern,” he said.
Mr Mkhize said the appeal would also help to ensure that the AIDS response continues unabated, including scaling up testing and treatment for people living with HIV. “We had already started a programme to achieve our 90–90–90 goals in 14 of the 52 districts and we cannot allow this pandemic to disrupt all these efforts and the successes and achievements we have already scored,” he said. “We appreciate the focus on people living with HIV, given the burden of disease.”
The Minister of Health told the launch that it was important to work with communities, civil society and other stakeholders already in place. The COVID-19 response would strengthen South Africa’s resolve to achieve universal health coverage, he said.
Our work
Region/country




Feature Story
Mitigating the impact of the COVID-19 pandemic among people living with HIV in India
06 May 2020
06 May 2020 06 May 2020For the more than 3000 people, including 330 children and adolescents, living with HIV and on antiretroviral therapy in Goa, India, the COVID-19 outbreak is a time of worry—they are worried about COVID-19 and they are worried about being able to stay on their HIV treatment during the lockdown in India.
In order to respond to one of those worries, the team at the Human Touch Foundation, a community-based organization that provides care and support to children and adolescents living with HIV, has, since the start of the lockdown, organized a force of volunteers to deliver antiretroviral therapy to people’s doorsteps.
Health officials at the HIV clinics provide a list of people who need deliveries of antiretroviral therapy, after making sure that the beneficiaries consent. Alternatively, several beneficiaries connect with the Human Touch Foundation directly for a supply of medicine.
“Most people living with HIV are still hiding their HIV status and do not wish that we come directly to their homes for the delivery. With poor mobile connectivity, in many cases we have no option rather than make more than two trips, instead of asking their location with the villagers,” said Peter Borges, the founder and Chief Executive Officer of the Human Touch Foundation.
Along with antiretroviral therapy, the Human Touch Foundation also provides essential groceries—rice, lentils, grams, oil and milk—for children and adolescents living with HIV and their families. “Many children and adolescents are with anxiety and depression, mostly concerning their survival, due to loss of income of their families and scarcity of essential supplies,” said Mr Borges. Bars of soaps are also provided with the packages, distributed in collaboration with UNAIDS, Reckitt Benckiser, the Just Imagine Trust and the Rotary Club of Panaji Riviera.
The Human Touch Foundation is also offering online psychosocial support to children and adolescents living with HIV. “We have streamlined our communication through telecounselling and support. We have a staff team giving coordinating and rendering support to the field team through assessment of the family,” Mr Borges added.
Similar efforts are being undertaken in Bangalore to support people living with HIV. Champion in Me, a community-based organization that provides care, support and skills to adolescents and young people living with HIV, has built a support system to reach out to communities during the lockdown. A force of young volunteers has partnered with the Karnataka Network of Positive People to distribute medicines to 140 people and food provisions to 1200 people. “I praise the courage of our volunteers and supporters that came out to help people living with HIV, in a time of crisis. This is when our organizations and leaders have to stand tall and join efforts to make sure nobody is left behind,” said Elvis Joseph, the Director of Champion in Me.
At the national level, the National Coalition of People Living with HIV in India (NCPI+) is coordinating efforts with the National AIDS Control Organisation (NACO) and other partners, including UNAIDS, to ensure adherence to treatment and a continuum of care for people living with HIV.
“Since the lockdown started, the National Coalition of People Living with HIV in India established a good communication platform through WhatsApp and emails connecting the National AIDS Control Organisation and networks of people living with HIV to closely monitor challenges, find joint solutions and help coordination,” said Daxa Patel, the President of NCPI+ and the Secretary of the Gujarat State Network of People Living with HIV. As a result, NCPI+ has helped more than 45 000 people living with HIV in India to get home deliveries of antiretroviral therapy.
“HIV-affected communities have played an important role delivering antiretroviral therapy to people who were not able to collect it themselves. The Human Touch Foundation, Champion in Me and the National Coalition of People Living with HIV in India are just some examples of what can be done at the national, state or city level by communities themselves. Many local solutions have been put in place in a joint effort between the government, UNAIDS and community-based organizations to get medicines, food or soap delivered to those in need,” said Bilali Camara, the UNAIDS Country Director in India.
















