Feature Story
UNAIDS and Akbaraly Foundation unite to transform the HIV response in the Indian Ocean region
06 June 2025
06 June 2025 06 June 2025UNAIDS and the Akbaraly Foundation have signed a landmark partnership agreement to reshape how HIV and women’s health are addressed across Madagascar and the Indian Ocean region.
Over the past 15 years, new HIV infections in Madagascar have surged by 151%, and AIDS-related deaths have risen by 279%. Of the estimated 70 000 people living with HIV in the country, only 20% are receiving treatment. These statistics reflect lives and families in jeopardy and communities in need.
This new alliance brings together two organizations with shared goals and complementary strengths. UNAIDS brings decades of global leadership in the HIV response., while the Akbaraly Foundation offers deep community trust and a proven ability to deliver results.
“This agreement goes well beyond organizational cooperation,” said UNAIDS Country Director, Jude Padayachy, “it represents a collective commitment to innovation, equity and results that matter.”
Since its founding in 2008, the Akbaraly Foundation, which also operates in India, Italy and Rwanda, has become a pillar of healthcare delivery in Madagascar, especially in underserved regions. Its mobile unit, LUISA, has travelled more than 25 000 kilometres to provide medical services in remote villages. Over 340 000 women have been screened for cancer and 480 000 people have received life-changing education on cancer prevention.
The partnership will focus on incorporating HIV services into the fixed and mobile Akbaraly medical infrastructure to extend their reach as well as training programmes for health professionals in Comoros to strengthen the region’s response capabilities.
In addition, UNAIDS and the Akbaraly Foundation will coordinate advocacy efforts during global campaigns such as World AIDS Day and World Cancer Day to strengthen public awareness and reduce stigma. This strategic alliance is a promise to deliver health with dignity, from city centres to the most isolated islands.
Region/country



Feature Story
UNAIDS supports countries to adopt differentiated service delivery approaches to HIV care
05 June 2025
05 June 2025 05 June 2025UNAIDS has supported eight countries including Mali, Angola, Madagascar, South Sudan, Indonesia, Pakistan, Philippines and Thailand to assess the strengths and weaknesses of their HIV care service delivery systems.
If countries are to succeed in reaching the 95-95-95 HIV targets, their health systems must adopt rights-based, gender-sensitive, and people-centered models to reach the underserved populations and improve service quality.
One such model is the differentiated service delivery (DSD) approach, which is designed to provide HIV services that are adapted to reflect the preferences and needs of people living with and vulnerable to HIV, while reducing unnecessary burdens on the health system.
UNAIDS mobilized Technical Assistance Demand Generation (TADG) funding support from USAID, to bring together national program stakeholders and community groups for a data-driven consensus building process. In each country, participants used a structured health system assessment and strengthening tool, developed by the HIV Coverage, Quality, and Impact Network (CQUIN), of the Columbia University, to make informed decisions on enhancing quality HIV testing, treatment, and care services.
According to participating country teams, the exercise facilitated a breakdown of national program landscapes into clear, actionable focus areas, and improved their understanding of differentiated delivery of HIV care services. Program teams were able to prioritize areas for focus and to streamline decision-making, which will ultimately lead to practical and sustainable enhancement of HIV service provision.
“Considering South Sudan is lagging behind in treatment coverage, this was a very timely technical support exercise, that will strengthen the HIV care response to achieve 95-95-95 targets through collective action, advocacy and investment” said Dr Agai Akec, Director, HIV Programme, Ministry of Health, South Sudan.
The participating countries recognised the value of adopting differentiated service delivery approach to HIV testing, HIV treatment and the management of advanced HIV disease; establishing linkages with related services such as maternal and child health, Tuberculosis and non-communicable disease care, and promoting collaboration between health facilities and the community.
UNAIDS role has been instrumental in using US catalytic resources to mobilize partners including WHO, The Global Fund, and technical support agencies to support national government and community groups to promote a critical area of work for HIV testing and treatment.
"The TADG catalytic funding helped the country beneficiaries to demystify Differentiated Service Delivery and to identify concrete areas for improvement within national programs. I would encourage countries to undertake more of these exercises to make services available and accessible by all, particularly those who have been left behind." said Fodé SIMAGA, UNAIDS Director, Science Systems and Service for All.
For further details and guidance on using the tool, visit:




Feature Story
“Who will protect our young people?”
02 June 2025
02 June 2025 02 June 2025Noncedo Khumalo grew up in a country with one of the highest HIV prevalence rates in the world, Eswatini—a country landlocked between South Africa and Mozambique. The 24-year-old has overcome her fair share of difficult times to make ends meet. The recent US funding cuts have now put her future in question.
“Young girls go for older men because when you finish high school and you want to pursue university, it becomes so hard for us, (economically) so many take a short cut,” she said.
This was how many of her friends acquired HIV. They had little awareness of HIV or how to protect themselves, she explained. She said that condom use was low and there were many myths about HIV including that it is a curse, only affecting some families.
Gender-based violence and sexual assault increase the risk of HIV infection. “In some cases, the abuser is a family member who is a bread winner, so women don’t report it,” said Ms Khumalo.
Dr Nondumiso Ncube, Executive Director of Eswatini’s National Emergency Response Council on HIV/AIDS, says that while the country has managed to consistently reduce new HIV infections, new HIV infections remain stubbornly high amongst the younger population, particularly adolescent girls and young women who are three to five times more likely to be infected than their male counterparts. As a result, Dr Ncube says young women and girls are at the centre of the country’s new HIV strategy.
Ms Khumalo was determined not to be one of these statistics. Every day she walked almost six kilometres to attend school. She got a diploma in social work and became involved with Young Heroes, a local community organization, supported by the United States President’s Emergency Plan for AIDS Relief (PEPFAR) three years ago.
Through this initiative, Ms Khumalo provided peer counselling to adolescents and young women about how to prevent HIV and about broader sexual and reproductive health. She visited schools and communities, offering information and support to help young people protect themselves against HIV.
Around 60% of Eswatini’s HIV response was funded by PEPFAR, however, in January the US cut all funding for HIV and issued a stop-work order for Young Heroes, forcing them to scale back their services. Ms. Khumalo lost her job.
Now unemployed and unable to reach the vulnerable young people she once served, Ms Khumalo fears for the safety of young women and girls in her community, where transactional sex between older men and young women, often motivated by poverty, and sexual and gender-based violence remain widespread. “I’m scared for the future of young people,” she said. “Without these HIV programmes, who will protect them?”
Nosipho Sacolo, a young woman living near the capital city of Mbabane expressed her fears. “After managing to stay free from HIV for so many years, we no longer have the services to protect us.”
UNAIDS Country Director for Eswatini, Nuha Ceesay says HIV prevention services—many of which are now closed—have been a game changer in Eswatini.
“Eswatini has made huge progress in preventing new HIV infections, with new infections falling by 73% since 2010,” he said.
The country still has some challenges, according to him. More than 1300 young women and adolescent girls are infected every year. And nearly twice the number of women are living with HIV compared to men.
UNAIDS and partners are concerned that the abrupt halt to PEPFAR supported HIV prevention programmes could reverse the gains that have been made.
A local network of non-governmental organizations (NGOs) working to ensure access to primary health care for people in Eswatini—including populations at high risk of HIV infection—CANGO, says the PEPFAR pause could have dire consequences for the country's HIV response, including a rise in new infections among young women and girls. "85 000 people were benefiting from the support, (now) all the people who were working in the sector, who were supporting our people living with HIV, are now sitting at home," said CANGO Executive Director, Thembinkosi Dlamini.
With PEPFAR’s support Eswatini had managed to ensure 93% of people living with HIV were on lifesaving antiretroviral treatment. This is one of Principal Secretary of the Ministry of Health, Khanyakwezwe Mabuza’s main concerns. “Treatment is not something you can skip,” he said. “We have to make sure that people continue to get their life-saving treatment.”
Meanwhile, Ms Khumalo is still hoping that the government and partners will not abandon the peer outreach workshops. Her livelihood and countless others depends on it as do the people they are helping to stay free from HIV.
Watch: Aid cuts hurt HIV response in Eswatini: UNAIDS fears rebound
Region/country

Feature Story
An urgent call to support youth-led organizations
28 May 2025
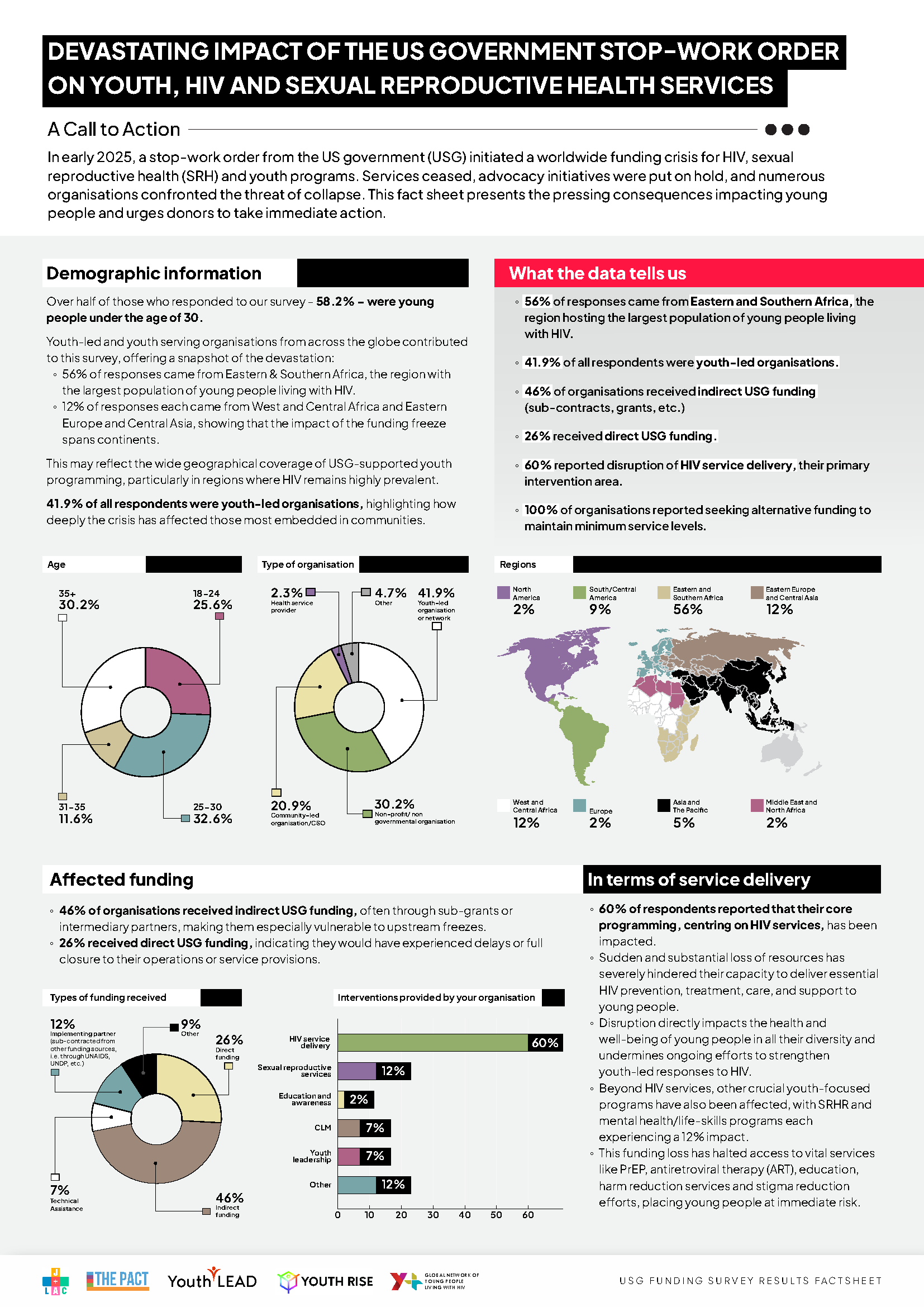
28 May 2025 28 May 2025The sudden stop-work order from the US government in early 2025 triggered a global funding crisis for HIV, sexual reproductive health (SRH), and youth programmes. This abrupt halt has left countless youth-led and youth-serving organizations struggling to survive, with devastating consequences for young people worldwide. The impact is profound, and the need for immediate action is critical.
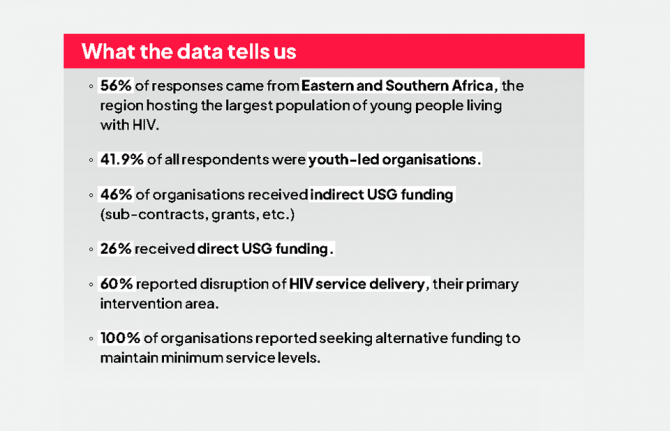
A survey conducted by Y+ Global, Youth LEAD, Youth RISE, The PACT, and J+LAC in March 2025 among organizations delivering HIV and SRH youth programmes reveals the stark reality faced by youth-led and youth-serving organizations. Forty-five youth-led and youth-serving organizations from around the globe completed the survey, with 56% of responses coming from Eastern and Southern Africa, the region hosting the largest population of young people living with HIV. Sixty percent of respondents reported disruptions to their core HIV services, severely hindering their ability to provide essential HIV prevention, treatment, care, and support. These disruptions directly impact the health and well-being of young people in all their diversity and undermine ongoing efforts to strengthen youth-led HIV responses.
Beyond HIV services, other crucial youth-focused programmes have also been affected, with SRH, mental health, and life-skills education programmes each experiencing a 12% decrease. Furthermore, activities like youth-led advocacy and engagement in policy and decision-making discussions have also been impacted, leaving youth voices under represented and unheard in the HIV response as well as other development areas.
The survey also warns about the abrupt policy changes occurring as a consequence, including the integration of HIV-specific clinics into general health systems, and the surge of restrictive laws targeting organizations working on gender, diversity, and sexual and reproductive health and rights, using the term “foreign agent” to criminalize their work. These changes are causing the collapse of service delivery models and increased barriers to youth-led organizations, further reducing accessibility for young people.
“The funding cuts are not just numbers on a spreadsheet; they represent real lives, real services, and real hopes lost. Youth-led organizations are the lifeline for so many young people, especially those most at risk,” shared Maximina Jokonya, Executive Director of Y+ Global. “We need urgent action from donors and governments to recommit and reinvest in youth leadership and safeguard the future of the HIV response,” she added.
Despite these setbacks, youth-led organizations are showing incredible resilience by launching crowdfunding campaigns, seeking alternative national and international partnerships, and continuing peer outreach with limited resources. Still, the long-term sustainability of these efforts is threatened by the funding crisis.
Youth and the next Global AIDS Strategy
Amidst this crisis, UNAIDS convened two global youth consultations in the context of the Global AIDS Strategy 2026 - 2031 development process to gather young people’s views and priorities for the future of the HIV response. More than 120 young people from diverse young key and vulnerable population groups participated in this consultative process. The key messages resulting from these consultations are unequivocal: young people demand involvement in decision-making spaces of the HIV response and in the development of alternative funding strategies, such as the sustainability roadmaps. They also demand a leading role in the implementation and monitoring of these decisions, as well as the positioning of human rights, gender equality, mental health, and innovation at the centre of the HIV response.
Call to action
Youth-led organizations are making an urgent call to all donors, partners, and policymakers to act now to save youth-led responses by reinstituting traditional funding support, increasing domestic and emergency funding solutions to maintain the operational stability of youth-led organizations, and supporting youth leadership in the HIV response.
Survey results
Our work
Related

Feature Story
“We must do everything we can to keep the lights on for the HIV response” says UNAIDS Country Director for Ethiopia Tina Boonto
26 May 2025
26 May 2025 26 May 2025Ethiopia, with a population of 130 million, is Africa’s second most populous country. Despite steady economic growth approaching low-middle income status, the country faces a daunting number of challenges, from economic pressures and development needs to recurring natural disasters such as droughts and floods, as well as conflict and other man-made crises. These factors mean Ethiopia still relies heavily on external aid-particularly for food security and humanitarian assistance.
On top of these existing burdens, HIV remains a significant public health challenge. The country is home to an estimated 610 000 people living with HIV, with over half a million currently on life-saving antiretroviral treatment-most of which is funded by international donors. Recent cuts in US funding have put Ethiopia’s HIV response at risk, threatening to reverse years of progress and placing additional strain on an already fragile health system.
We sat down with Tina Boonto, UNAIDS Country Director for Ethiopia, to discuss the impact of the funding crisis, the government’s response, the resilience of communities, and what needs to happen next to protect Ethiopia’s HIV response.
Q: What is the current situation, and how has the recent US funding crisis impacted the HIV response?
Ethiopia has made significant progress in its HIV response in recent years and is on track to reach the UNAIDS 95-95-95 targets with 90% of people living with HIV in the country being aware of their HIV status; 94% of those diagnosed with HIV receiving antiretroviral (ARV) therapy; and 96% of people on ARV therapy achieving viral suppression. The US Government through PEPFAR and the Global Fund have been the primary funders for the HIV response, supporting treatment for over 530 000 of the estimated 600 000 people living with HIV in the country. However, the sudden cuts had a devastating impact. Critical services have stopped, people have lost their jobs, and many clinics have closed their doors. People living with HIV now face uncertainty about their access to medication, testing, and prevention services.
In Bahir Dar, for example, programmes for key population have stopped, outreach workers have lost their jobs, and peer support groups have been terminated. It’s heartbreaking to see the situation on the ground. Clients arrived at clinics to find them closed, and many were left without guidance or support.
Women are anxious about the availability of medication and prevention tools like condoms. Without these, the risk of HIV transmission increases, and the health of those already living with HIV deteriorates. Some cannot even afford basic necessities like food, let alone treatment.
Q: How are communities responding to the collapse of HIV services?
Despite the collapse, communities are showing incredible resilience and a fighting spirit. Peer educators, youth groups and mothers are stepping in where formal systems are failing. For example, in the Afar region, a case manager working with people living with HIV continued his outreach work despite funding cuts. He was able to get funding from the health bureau and shared “even if the money is not enough, I’m happy to continue to help reach people living with HIV, providing pregnant women information on how to prevent transmission to their babies”.
But while these community-led efforts are inspiring, they cannot replace the need for sustainable funding. Community members often live below adequate income levels, and they need support for basics like transport and food. UNAIDS is encouraging the government to consider a social contract with community organizations-similar to Ethiopia’s successful Health Extension Worker model-so that peer outreach workers can be formally supported and paid for their essential outreach work.
The reason why we are pushing for outreach workers to be supported is because stigma and discrimination remain significant barriers. Even after 40 years of the HIV epidemic, people living with HIV in Ethiopia still experience stigma, which deters them from seeking care at public facilities. Many fear being discriminated against or not receiving adequate services. This is why the role of community peer outreach is so vital. Without armies of community outreach workers, especially in high-burden areas, it’s impossible to have a successful HIV programme.
Q: What lessons can be drawn from this crisis for the future of HIV response in Ethiopia and beyond?
The crisis has exposed the fragility of systems built around a single funding stream. When the money stopped, so did services, trust, and hope. We must build resilience into the system from the start. Community-led organizations must be recognized as essential, and youth-led innovation must be scaled up. Emergency preparedness and integrated, people-centered solutions are crucial, especially as HIV intersects with conflict, displacement, and gender-based violence. HIV must remain central to humanitarian, development and recovery agendas-not as an afterthought, but as a foundation.
UNAIDS is also supporting by working on producing an investment case to prioritize key components of the HIV programme for government funding. There are ongoing discussions about new partnerships with the private sector and exploring alternative financing mechanisms. There is political will. The Ministry of Health is considering adopting the methodology of the HIV Sustainability Roadmap to develop a broader health sector sustainability strategy. UNAIDS is supporting these efforts by helping to produce a sustainability strategy and mobilizing resources alongside other donors
Q: What steps is the Ethiopian government taking to address the funding crisis?
The government recognizes this as a wake-up call and is actively considering solutions to find resources to cover priority health issues, including HIV, tuberculosis, and malaria. However, the scale of the challenge is enormous-external assistance for Ethiopia’s health, humanitarian and development needs amounts to around US$ 2.7 billion annually. The government is exploring options such as introducing a social tax, where all workers would contribute to health funding, but this is still under parliamentary discussion. While these efforts are encouraging, they are not yet sufficient to fill the gap left by international donors.
Q: How is UNAIDS supporting the government and the HIV response during this crisis?
UNAIDS is playing a critical role. In response to the funding crisis, we conducted immediate impact surveys to understand which programmes have stopped or are ongoing, and what the consequences are on the ground. This information feeds into the national plans and sustainability plan.
We are also producing an investment case to help the government prioritize key components of the HIV programme for domestic funding. Our costing data enables us to propose affordable models, like social contracting with community organizations.
We are reviving HIV prevention efforts, including using AI-powered digital platforms and chatbots to reach young people with real-time information. Ethiopia was also piloting long-acting injectable antiretroviral medicine to prevent HIV or ‘PrEP’ before the funding cuts stopped this progress.
Finally, we are working closely with the Ministry of Health, the Global Fund, and community organizations to mobilize resources and advocate for integrated, sustainable solutions.
Q: What is your message to the international community at this critical juncture?
We need global solidarity now more than ever. We are so close to ending AIDS as a public health threat by 2030. Over half a million people in Ethiopia are on antiretroviral treatment—we cannot let them down. The world has come too far, and too many have sacrificed too much to let progress slip away now. We must do everything possible to keep the lights on for the HIV response, both in Ethiopia and globally.
The resilience of Ethiopian communities is inspiring. People are refusing to give up, finding new ways to support each other and keep the response alive. With renewed commitment from the government, partners, and the international community, we can protect the progress made and continue moving towards ending AIDS as a public health threat.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads the global effort to end AIDS as a public health threat by 2030 as part of the Sustainable Development Goals.
Following the US funding cuts in January, UNAIDS is working closely with governments and partners in affected countries to ensure that all people living with or affected by HIV continue to access life-saving services. For the latest updates, please visit unaids.org
Related resources
Watch: Tina Boonto, Ethiopia Country Director: Communities are going out of their way but they need help
Watch: UNAIDS asking government to increase domestic funding for the HIV response in Ethiopia
Watch: "We cannot let people down," says Tina Boonto, Country Director in Ethiopia
Region/country
Related


Feature Story
Global leaders convene to accelerate access to long-acting HIV prevention technologies amidst funding cuts
23 May 2025
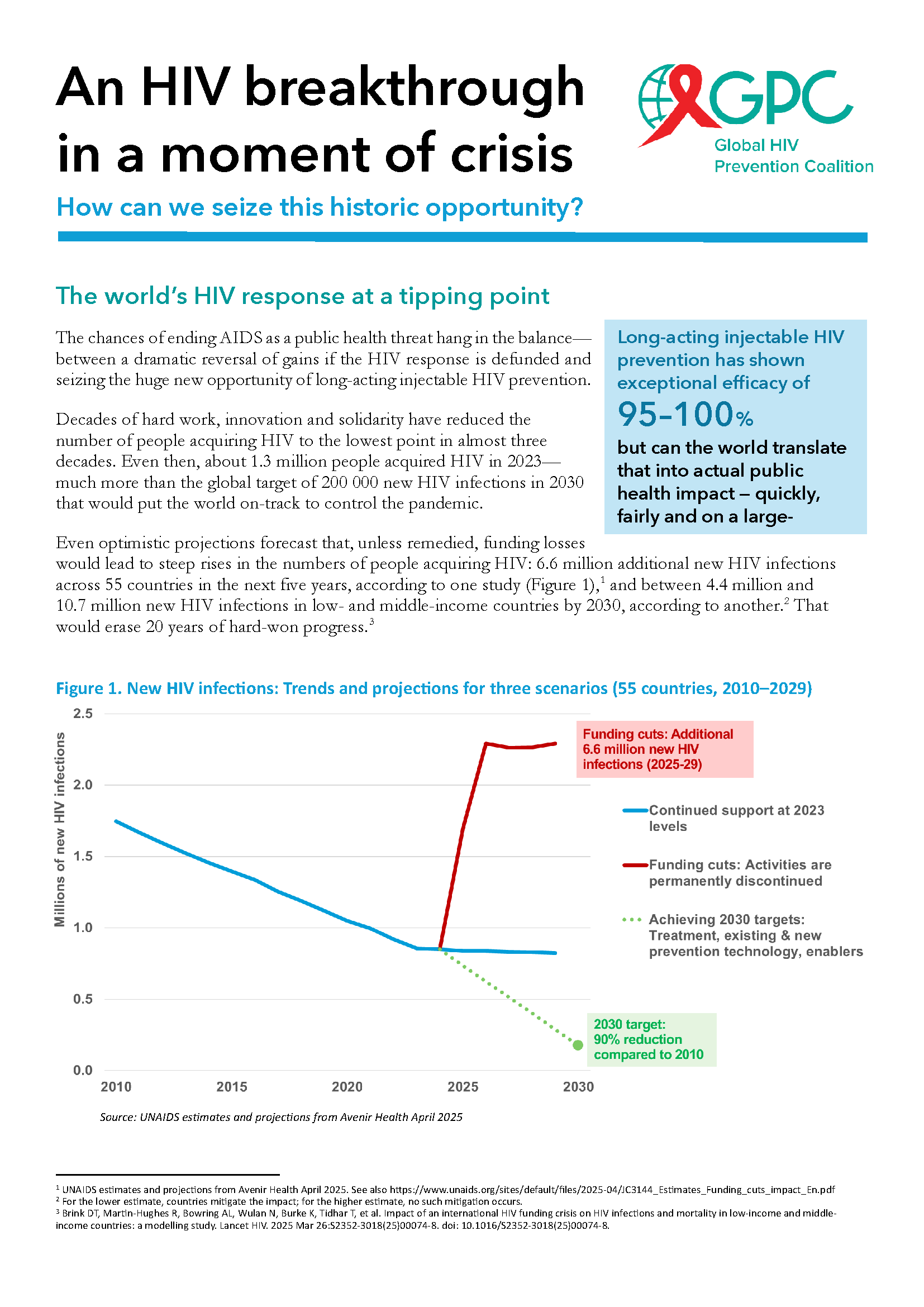
23 May 2025 23 May 2025The global response to HIV has reached a crucial juncture. Groundbreaking scientific advances, including the development of long-acting HIV prevention technologies like lenacapavir and cabotegravir, offer a transformative opportunity to curb the epidemic.
Long-acting injectables, which were hailed by Science magazine as one of the major breakthroughs in science in 2024, have shown exceptional efficacy, with lenacapavir demonstrating nearly 100% protection against HIV infection.
Despite these unprecedented advancements, the HIV response faces a dire threat from severe funding cuts. With more than 1.3 million new HIV infections annually, three times the target for 2025, financial constraints and a lack of sustained political will threaten to undo decades of progress. Global health experts warn that without urgent action to ensure continued investment, the ability to scale these life-saving technologies will be jeopardized, leaving millions at risk.
On the eve of the 78 World Health Assembly, global health leaders, government ministers, pharmaceutical companies, and civil society representatives gathered at UNAIDS headquarters in Geneva for the High-Level Multisectoral Leadership Dialogue on HIV Prevention. This High-Level dialogue, organized by the Global HIV Prevention Coalition and co-hosted by UNAIDS in collaboration with UNFPA, WHO, and UNDP, the Federal Republic of Brazil, and the Kingdom of the Netherlands, focused on accelerating access to long-acting HIV prevention technologies and advancing sustainable prevention systems.
Referring to the current funding crisis, Winnie Byanyima, Executive Director of UNAIDS, warned that “If we continue down this path, we could see an additional 6 million HIV infections and 4 million AIDS-related deaths by 2029. Put simply, we will lose control of the AIDS pandemic. But we have an opportunity today. We have new, long-acting HIV prevention tools that could fundamentally reshape the HIV response, putting us back on the right path.”
Global leaders presented successful national models from Africa, Asia and Latin America, illustrating how innovative prevention strategies are being implemented despite financial challenges. Mariangela Simao, representing Brazil, said “PrEP in Brazil is now a reality. We initially set a target of reaching 50,000 people with PrEP by 2025, but we’ve already surpassed that milestone, with 122,000 people currently using it. Our next goal is to reach 300,000 users by next year. Data shows that HIV incidence is declining in cities with more than 100,000 inhabitants where PrEP coverage is higher.”
Global HIV Prevention Coalition co-chair and CEO of AVAC, Mitchell Warren called for choice in HIV prevention.
“Condoms work well for some people and situations. Oral PrEP is safe and effective for those who can adhere to daily pill taking. The monthly dapivirine vaginal ring is a preferred option for some women, as is voluntary medical male circumcision for many men, while harm reduction is highly effective for people who inject drugs. Now, long-acting injectables offer an additional option for the many people who struggle to protect themselves from HIV and want more convenient and discreet prevention options.”
Key panel discussions focused on the cost of inaction, the significance of equity in access, and the role of long-acting prevention in the future HIV prevention toolkit.
The event underscored the urgent need for a multisectoral approach to overcoming structural barriers to prevention, including regulatory, financial, and societal challenges. The discussions highlighted that global solidarity and sustained political will are essential to closing the prevention gap and achieving the UNAIDS 2030 targets of fewer than 200 000 new HIV infections annually.
Ambassador Paul Bekkers, Permanent Representative of the Netherlands to the UN, closed the dialogue with a powerful call to action: “Not acting now means leaving a larger HIV epidemic to the next generation. Or we can put the world on course to achieve HIV epidemic control and eventually the end of AIDS as a threat to public health. As members of the Global HIV Prevention Coalition, we can achieve this together.”
As part of this pivotal moment, UNAIDS and the Global HIV Prevention Coalition launched a new brochure titled An HIV breakthrough in a moment of crisis: How can we seize this historic opportunity?
Our work
An HIV breakthrough in a moment of crisis; How can we seize this historic opportunity?
Related


Press Release
UNAIDS encouraged by comments from Elon Musk that he will fix the US funding crisis for HIV services
21 May 2025 21 May 2025Mr Musk made the remarks during an interview with Bloomberg’s Mishal Husain at the Qatar Economic Forum on 20 May
GENEVA, 21 May 2025—UNAIDS is deeply encouraged by the statement from Elon Musk that he will fix the current crisis related to a lack of US Government funding for lifesaving HIV services. UNAIDS is tracking daily the impacts of US funding cuts on HIV services for people living with and affected by HIV around the world as the data and stories of impact on UNAIDS website show.
Currently, many HIV prevention programs supported by the US President's Emergency Plan for AIDS Relief (PEPFAR) have been stalled. The Administration issued a limited waiver providing for continuity of some services, including comprehensive HIV testing and treatment, but it is not being fully implemented within countries, and the waiver excludes almost all HIV prevention services except those for pregnant and breastfeeding women.
For detailed, specific examples of the impact of US funding cuts in dozens of countries see here: Impact of US funding cuts on the global HIV response | UNAIDS
UNAIDS estimates indicate that the permanent discontinuation of HIV prevention and treatment programmes currently supported by PEPFAR would, between 2025 and 2029, lead to:
- An additional 6.6 million new HIV Infections.
- Around 2300 additional new HIV infections per day.
- An additional 4.2 million AIDS-related deaths.
- Over 600 additional AIDS-related deaths per day.
Estimating the potential impact of HIV response disruptions
We can end the AIDS pandemic, but we cannot do so without continued partnership and leadership by the US on HIV prevention efforts for those most in need. Latest estimates show that 1.3 million people were newly infected with HIV in 2023; many were among the most marginalized and vulnerable groups, including young women and girls. Every week some 4000 young women and girls became infected in 2023.
Some countries relied on PEPFAR for over 95% of their funding for HIV and while UNAIDS has been supporting countries' transition to self-reliant nationally funded responses, this transition must be done methodically to ensure no more lives are lost during this process.
UNAIDS has also been impacted by US funding cuts; given the critical roles UNAIDS is playing to build a sustainable future for the AIDS response, the cuts undermine continued progress to end AIDS and transition to sustainability nationally owned and financed HIV responses.
UNAIDS is encouraged by Mr Musk’s remarks and urges the US to continue their leading role in ending AIDS by restoring HIV prevention and treatment funding to countries most affected by HIV. UNAIDS stands ready to work hand in hand with the US to help support sustainable transitions in the coming months and into the future.
Watch original interview:
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.

Feature Story
‘My greatest fear is that we will return to the dark days of the epidemic’
21 May 2025
21 May 2025 21 May 2025UNAIDS Country Director reports on the impact of funding cuts to the HIV response
The HIV response in Zambia, known as a model of success in sub-Saharan Africa, is now facing major challenges following the abrupt and significant cuts to US funding. It has led to widespread disruption: clinics have closed, prevention services have been scaled back, and thousands have lost access to lifesaving medication. Yet the Zambian government and partners are stepping in to protect the progress made.
In this interview, UNAIDS Country Director for Zambia, Isaac Ahemesah, details the fallout from these funding decisions on health services, vulnerable communities, and the country’s ability to sustain progress against HIV-and outlines what is urgently needed to avert further health crisis.
“In 1997, life expectancy in Zambia was about 46 years due to HIV and AIDS. In 2023, it was nearly 66 years because of the investments made and the strong partnership.”
Q: How have the US funding cuts impacted the HIV response in Zambia?
Zambia has long relied on international aid, including substantial support from PEPFAR. Three years ago, the US government’s commitment stood at approximately US$ 402 million, which was subsequently reduced to US$ 392 million, and most recently to US$ 367 million. Despite these reductions, the contribution remains significant, not only to the HIV response, but to Zambia’s overall health sector. To put it in perspective, of the US$ 600 million in total US support to Zambia for development last year, US$ 367 million, around 60%, was allocated to HIV.
However, the abrupt funding cuts led to the termination of key programmes. More than 11 000 health workers supporting the HIV response, and approximately 23 000 health workers providing services for malaria, tuberculosis, and other health needs, were impacted.
Several essential initiatives were stopped. These include the closure of 32 wellness centres that served over 20 000 key populations, including LGBTQ+ people, sex workers, and people who inject drugs, across seven of Zambia’s ten provinces. These centres offered critical services such as HIV testing, treatment, and support.
All DREAMS programmes, which supported adolescent girls and young women in 22 districts, have also been shut down. This has cut off access to HIV prevention, life skills, and economic empowerment activities for thousands of vulnerable girls.
HIV prevention services have also been disrupted. Sixteen standalone centres providing voluntary medical male circumcision - a proven HIV prevention method - have ceased operations. Nearly half of Zambia’s pre-exposure prophylaxis (PrEP) services, which help prevent HIV infection, were funded by the US and have now been discontinued.
Community-led monitoring programmes, which ensured quality and accountability in HIV care, have also been terminated. Furthermore, the Smart Health electronic medical records system, along with platforms used for forecasting and quantifying medical supplies, is no longer operational, making it increasingly difficult to manage patient care and maintain drug inventories.
Q: What will happen if the DREAMS programme is not reinstated?
Currently, Zambia records approximately 23 000 new HIV infections annually, with about 8700 occurring among young people aged 15 to 24. Notably, 60% of infections in this age group happen among girls.Without support for prevention and treatment interventions, new HIV infections could surge to 180 000 per year by 2030. Among young people, infections could rise to over 60 000 annually by 2030.
Gender-Based Violence (GBV) remains a growing concern in Zambia, and each GBV case carries a heightened risk of HIV transmission. Addressing this requires a coordinated, multi-sectoral approach that extends beyond HIV alone to include family planning and reproductive health services. National partners are working to reinvigorate this multi-sectoral response so that all relevant sectors-education, gender, internal affairs, and others-actively share responsibility for the HIV response.
Given the challenges, there is a pressing need to pursue local initiatives and mobilize alternative funding sources to support adolescent girls and young women, safeguarding their health and rights.
Q: Are there concerns about supplies of HIV medicines?
Yes, there is significant concern. At present, Zambia has sufficient antiretroviral (ARV) medication to last until the end of the year. However, the US has announced an additional US$50 million cut in funding for medicines and health commodities, effective from next year, due to concerns about drug theft. This will make it extremely difficult to ensure an uninterrupted supply of ARVs, particularly for the most vulnerable populations. There have already been reports of people living with HIV receiving reduced quantities of medication - less than the standard three- to six-month supply - due to ongoing uncertainty and challenges in stock management.
Q: What is UNAIDS doing to support Zambia during this crisis?
At the onset of the US funding freeze, UNAIDS immediately partnered with the Ministry of Health to convene national leadership and all key stakeholders. This was critical to coordinate a unified and effective response to the sudden disruption. We quickly led an impact assessment to understand how the freeze was affecting Zambia’s HIV response on the ground. This provided the data needed to guide urgent decisions.
One of our first steps was to work with the government and partners, we helped define a minimum package of essential HIV services that could realistically be maintained with the reduced resources available. We costed this package at about US$ 147 million and presented it to the Cabinet and Presidency for consideration in the national budget.
At the same time, we supported the development of the HIV Sustainability Roadmap, which explores alternative domestic financing options. This includes innovative approaches such as leveraging health insurance schemes and introducing total market strategies-for example, making PrEP and vaginal rings available through pharmacies.
We also worked closely with the Ministry of Health to revise policies to better fit the current context. For example, we supported allowing longer antiretroviral therapy refills—for up to six months–—to reduce the burden on both patients and the health system. We also helped adjust HIV testing protocols to manage limited supplies more effectively and piloted new service delivery models outside traditional health facilities to expand access.
At the operational level, we partnered with WHO, UNICEF, UNFPA, and others to monitor weekly stock levels of HIV commodities, ensuring timely responses to shortages. We support civil society organizations, especially those representing key populations, in transitioning clients from closed wellness centers to public health facilities, helping maintain continuity of care.
To address broader systemic challenges, UNAIDS contributed to the restructuring plan for the Zambia Medicines and Medical Supplies Agency to improve accountability and strengthen the supply chain.
Our Resource Allocation Forecasting Tool was used to estimate the real cost of sustaining Zambia’s HIV response, which we estimated at around US$ 150 million annually. This tool helps the government and partners plan budgets more effectively.
UNAIDS acts as the central hub for information-sharing and advocacy around the impact of US funding cuts. We regularly present needs assessments to the UN Country Team and support ongoing fundraising discussions to urgently mobilize resources to sustain services.
Finally, we have supported training for health workers to promote respectful, non-discriminatory care for key populations now accessing mainstream health services. This is vital to ensure no one is left behind despite the challenges.
Q: What is the solution to ensure sustainable financing for Zambia’s HIV response, and avoid such a crisis in the future?
The key to sustainable financing lies in increasing domestic funding and reducing reliance on external donors. While the recent US funding cuts were abrupt and challenging, this situation was not entirely unexpected. For years, Zambia and other countries have been encouraged to take greater ownership of their HIV responses. The real surprise was the speed and scale of the funding reductions.
To protect its HIV response, Zambia must now mobilize domestic resources. This includes engaging local philanthropic organizations, expanding the role of national health insurance schemes, and ensuring that HIV services are fully integrated within these systems. Innovative models like risk pooling and market-based access to prevention tools, such as making PrEP and vaginal rings available through pharmacies, will also be key to expanding reach and ensuring continuity.
On the global level, the HIV response must increasingly pivot toward long-acting treatment and prevention options, such as injectable PrEP and antiretroviral treatment. These innovations can help simplify adherence and improve outcomes.
Zambia is also exploring total market approaches, where the private sector helps supply prevention and treatment services. In addition, local production of ARVs could help reduce costs and improve supply chain stability.
Critically, the country has already shown that essential HIV services can be maintained on smaller budgets, provided resources are used efficiently. But for long-term sustainability, the government must take the lead. This means prioritizing HIV in the national budget and exploring innovative domestic revenue sources, such as earmarked taxes on alcohol, tobacco, or health products.
While international partners will remain important, the responsibility for a predictable, sustainable HIV response now rests squarely with Zambia itself—to protect the lives and health of its 1.4 million citizens living with HIV, and to ensure that no one is left behind.
Q: What’s your message to the international community?
Today, I believe the global HIV response stands at a crossroads. The decisions we make now will either help the world achieve Sustainable Development Goal 3.3—the target of ending AIDS as a public health threat by 2030—or risk a devastating reversal.
If we ease up, we could see a return to the 1990s, when new HIV infections spiraled out of control, HIV-related deaths surged, and the global economy suffered greatly.
All we ask for is a final push— a sustained commitment to support countries in fulfilling their promises to end AIDS as a public health threat. I urge the US government and all other donors to reconsider the recent funding cuts. We need to keep our foot firmly on the accelerator until we reach the finish line.
Otherwise, my greatest fear is that we will return to the dark days of the epidemic, with significant increases in new infections and deaths.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads the global effort to end AIDS as a public health threat by 2030 as part of the Sustainable Development Goals.
Following the US funding cuts in January, UNAIDS is working closely with governments and partners in affected countries to ensure that all people living with or affected by HIV continue to access life-saving services. For the latest updates, please visit unaids.org
Related resources
Watch: Integration of HIV services key
Watch: Final push needed
Region/country
Related

Feature Story
‘We Can’t Afford to Go Back’- UNAIDS Country Director on HIV funding cut in Eswatini
14 May 2025
14 May 2025 14 May 2025Eswatini, a country once described as the epicentre of the HIV epidemic with nearly 1 in 3 adults living with HIV in 2015 [adult HIV prevalence in 2015 was 31%]. But Eswatini managed to turn around its HIV epidemic, reducing new HIV infections from a peak of 21 000 per year in 2000 to 4 000 in 2023, a remarkable result, achieved with the support of US funding.
However, the sudden US funding cuts threaten to undo years of progress. We sat down with Nuha Ceesay, UNAIDS Country Director in Eswatini, to discuss the current situation, the impact on HIV services, and the way forward.
Q: How are US funding cuts impacting Eswatini’s HIV response?
Eswatini’s HIV response has been a success story, by transforming a crisis that once saw extremely high HIV prevalence rates, into a model of resilience and opportunity. But the recent US funding cuts, representing about half of the country’s HIV response budget, have left the people living with and affected by HIV in despair, the government was not notified and left unprepared, and the people working to end AIDS are in total shock. There is real concern that new HIV infections and AIDS-related deaths will rise, reversing years of hard-won progress. The cuts threaten not just HIV treatment and prevention, but also the broader health system improvements, data collection, jobs and empowerment of people living with HIV.
Q: What disruptions are being seen on the ground?
The effects are immediate and widespread. HIV testing services, the gateway to treatment, are now limited. With fewer people being tested, many may unknowingly be infected with HIV, missing the chance for early treatment and increasing the risk of further transmission. This could push annual new infections, which are currently around 4 000, even higher, and add pressure to already strained treatment resources. Stockouts of antiretroviral, lab test kits, and condoms are expected within months, and health worker layoffs are affecting service delivery and quality data collection. Primary prevention services, such as medicine to prevent HIV (PrEP), education campaigns, and voluntary medical male circumcision for HIV prevention (which is around 60% effective in preventing HIV) have also been scaled back or suspended.
We are also seeing a stop of the DREAMS programme which is a major setback for adolescent girls and young women, who are disproportionately affected by HIV in Eswatini. DREAMS provided prevention education, skills, and socio-economic support to young women. Its termination leaves them more vulnerable to infection and strips away resources that have been central to empowering this high-risk group. HIV prevalence among young women and girls aged between 15 and 24 years was 70% higher than among young men in Eswatini in 2023.
Read more about the impact on UNAIDS website
Q: How is UNAIDS responding to these challenges?
UNAIDS is working closely with the government and partners to continue the work of developing and implementing the HIV Sustainability Roadmap. This will help Eswatini’s HIV response to gradually shift from being reliant on international aid to increasing its domestic funding which will lead to the government taking full ownership of its HIV response. The first phase of this roadmap has already been launched, focusing on building resilience and long-term solutions.
UNAIDS has also worked closely with the Ministry of Health and partners to map the impact of the funding cuts, identify service gaps, and strategize on mitigating disruptions. Collaboration with the Ministry of Health, UN partners, and civil society remains central, but the transition to sustainability is a complex and gradual process.
Q: What’s your message to the international community?
The successes that we celebrate in the HIV response are built on mutual accountability and global solidarity. That’s what enabled countries like Eswatini to shift the narrative-from a crisis by leading a response that brought down new HIV infection to 4 000 compared to when new infections were as high as 21 000.
It is therefore devastating to see all the hard-won gains being reversed at this stage. This is the moment we need to come together in solidarity and in partnership to accelerate our collective efforts.
Ending the epidemic is like a marathon. We have run the race many miles, but the end is what matters. If we cannot reach that finish line, it means we have not completed, and we cannot afford that.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads the global effort to end AIDS as a public health threat by 2030 as part of the Sustainable Development Goals.
Following the US stop work order in January, UNAIDS is working closely with governments and partners in affected countries to ensure that all people living with or affected by HIV continue to access life-saving services.
For the latest updates, please visit unaids.org
Related resources
Watch: "Access to prevention services no longer available", Nuha Ceesay, Eswatini UNAIDS Country Director
Watch: UNAIDS actively working on forward planning with governments, says Eswatini country director
Watch: "From crisis to opportunity," says UNAIDS citing Eswatini HIV response
Region/country
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025


Feature Story
Community-led HIV services under threat: global networks and UNAIDS track the impacts of the US funding cuts
13 May 2025
13 May 2025 13 May 2025Community-led organizations are the backbone of the HIV response in many countries, providing access to HIV services for key populations, advocating for human rights and monitoring the HIV response. However, data collected by community-led organizations shows mass shut-downs of life-saving, peer-led services, significant – or total – budget cuts, staff lay-offs and rising levels of stigma, discrimination and mortality rates.
Two new key population-led reports, one by Global Black Gay Men Connect (GBGMC) and another by the International Network of People Who Use Drugs (INPUD), document the consequences of the US President’s Executive Order in January 2025 which froze all US foreign assistance. These reports highlight how services led by and for key populations are facing deep uncertainty about their future due to the funding cuts and loss of staff.
In its Frozen Out report, GBGMC found that 36% of partners supported by the US President’s Emergency Plan for AIDS Relief (PEPFAR) shut down within one week of the Executive Order. Another 19% said they could not operate beyond one month without renewed support. Similarly, INPUD’s report The Human Cost of Policy Shifts describes significant disruptions across harm reduction programmes. Nearly half (45%) of the organizations surveyed reported major budget losses, and one in four lost between 75% and 100% of their harm reduction programming. Critical services including peer-led outreach, HIV and hepatitis C testing, opioid agonist therapy, and overdose prevention have been disrupted.
A cascading crisis
The GBGMC report states that nearly 93% of key population-serving partners in Kenya reported experiencing full or partial service shutdowns. In Nigeria, every PEPFAR implementing partner providing services to key populations was reportedly affected. Across Kenya, Uganda and Nigeria, an estimated 2.2 million people have lost access to key population-focused HIV prevention services.
The report also warns that even short-term interruptions can have life-threatening consequences. Each day, an estimated 200,000 people rely on receiving their HIV treatment through US government-funded sites. Interruptions risk treatment failure, HIV transmission and the emergence of resistance to HIV medicines. Prevention efforts are also at risk, with US government funding supporting nearly 90% of global pre-exposure prophylactic (PrEP) initiatives.
“The PEPFAR funding freeze has led to the closure of numerous organizations and the disruption of essential HIV prevention services, leaving millions at risk. Immediate action is imperative to restore funding and protect key populations from further harm,” says Micheal Ighodaro, Executive Director of GBGMC
Impacts on organizations led by people who use drugs
INPUD’s report, The Human Cost of Policy Shifts, provides a detailed picture of how harm reduction services have been devastated by the US funding cuts. Based on a global rapid assessment of 101 respondents, the report reveals that nearly half lost between 26% and 100% of their harm reduction budgets, and 23% lost more than three-quarters of their funding.
The most disrupted services included peer-led outreach (41%), legal and human rights support (36%), HIV testing (35%), services for women who use drugs (33%), and overdose prevention (25%). The consequences for individuals and communities have been severe. 47% of organizations reported that people are now going without harm reduction supplies such as sterile syringes and naloxone, and 46% said people are relying on underground or informal networks for access. 30% observed increases in overdose deaths. Additionally, 62% of organizations documented rising stigma and discrimination against people who use drugs.
The report also highlights a particularly stark impact on women who use drugs. Of the 54 organizations that previously offered tailored services for women, 68% halted outreach, and over a third had to reduce or close services altogether.
“While increasing overall funding is important, it is equally vital to ensure that organizations led by people who use drugs receive targeted support to run harm reduction services that effectively address their communities’ unique challenges and needs," says Anton Basenko, Executive Director of INPUD
Heightened stigma and structural risks
Even before the funding cuts, key populations faced legal and social barriers
including criminalization, discrimination, and denial of services. According to reports gathered through UNAIDS’ dialogues with global and regional networks, these challenges are now intensifying. Community organizations have documented a rise in harassment, hate speech and healthcare discrimination. In some countries, specialized clinics are being “mainstreamed” into general health systems without adequate training or protections ensuring safe access.
UNAIDS’ response and coordinated action
Since February 2025, UNAIDS has been convening biweekly virtual dialogues with global key population networks, civil society advocates and international partners to share updates, raise concerns, and coordinate efforts to protect HIV services. At the regional level, UNAIDS is also convening with networks and joining forces to document the impact of funding disruptions and shape collective responses. These engagements have informed UNAIDS’ advocacy and programming supporting the launch of tools like the Rapid Action Financing Tool, strengthening country-level tracking through the UNAIDS impact portal (launched in early 2025) and amplifying community voices at global forums such as the UN’s Commission on the Status of Women and the Human Rights Council. Through continued collaboration with country teams, regional networks, and civil society, UNAIDS remains committed to co-creating solutions and prioritizing community-led responses.
A call for urgent action
GBGMC and INPUD urge governments, donors, and development partners to take immediate steps to:
- Restore and increase funding for community-led and key population-focused services and establish dedicated funding streams for key population-led organizations
- Establish pooled emergency funding mechanisms to sustain prevention and harm reduction
- Ensure meaningful community engagement in funding, service design, and legal reform
- Protect peer-led HIV services, which are grounded in principles of dignity, safety, and equitable access