Feature Story
US foreign aid cuts puts the lives of people who use drugs at risk
05 May 2025
05 May 2025 05 May 2025Godfrey Swai is shaken. Since the end of January, the US aid funding cuts have meant that he can only afford for his staff to work a couple of hours twice a week compared to a full five days.
As the Executive Director of an organization called Methadone Family Against Drug Abuse based in Tanzania he has had to scramble. “Despite clinics being partly opened, our outreach in hotspots came to a halt,” he said. “The community is scared.”
In many countries, like Uganda, centres distributing opioid agonist maintenance therapy (OAMT), also known as medically assisted treatment, closed for a month. OAMT is often prescribed as oral medication to alleviate withdrawal symptoms and reduce injecting drug use, which in turn lowers the risk of acquiring HIV. In 2022, the risk of acquiring HIV was 14 times higher for people who inject drugs than for people in the overall adult population.
“We know that disruption to OAMT is a threat to life,” said Catherine Cook, Sustainable Financing Lead at Harm Reduction International (HRI).
Banza Omary Banza, Director of Community Peers for Health and Environment Organization in Tanzania, agrees. “Fearing a stock out of methadone–the OAMT medicine–we have witnessed people returning to heroin use and hitting the black market,” he said.
A setback that has a myriad of repercussions.
According to a recently published survey by International Network of People who Use Drugs (INPUD) there has been large-scale suspension of outreach and harm reduction programmes, including needle and syringe distribution, HIV and hepatitis C testing, overdose prevention and legal support services.
“The hardest hit has really been the peer-led outreach,” said Aditia Taslim, Advocacy lead at INPUD. “Three months later no alternative solutions have been put in place. It’s like we are being erased from the HIV response.”
For harm reduction advocates this crisis isn't just financial, it's profoundly human.
“Peers and peer outreach have been the backbone of the harm reduction response," said Juma Kwame, Director of Tanzania Network of People who Use Drugs (TANPUD). “Without people seeking out their peers you don’t have linkages to treatment to health services or to recovery.”
Team leader at a network of women who use drugs in Dar es Salaam, Grace Mbalawa, said that most people living with HIV who use drugs have little income or a stable home, so the loss of support programmes has upended their lives.
“They no longer have a safe space and many are stretching out their HIV treatment by skipping days in case they can no longer get their medicine,” she said. People living with HIV must take daily treatment to stay healthy and suppress the virus. In addition, when the viral loads of people living with HIV are suppressed, sexual transmission of HIV does not occur.
International donor funding comprised 67% of total harm reduction funding in 2022. Most of the money went towards HIV prevention programmes for people who inject drugs. The US President’s Emergency Plan for AIDS Relief (PEPFAR), a decades-long initiative, supported OAMT to 27 000 people in seven countries (India, Kenya, Kyrgyzstan, South Africa, Tajikistan, Tanzania and Uganda). In many cases these were and are the only services available. They also supported harm reduction programmes in Mozambique, Myanmar and Kazakhstan.
Many fear the loss of funding threatens to undermine human rights and marginalize communities already battling stigma and years of neglect with women bearing a big portion of the impact.
“One in three people who use drugs are women but women only account for one in five people accessing services due to the stigma of being a woman using drugs,” said Ms Cook from HRI. “They risk having to admit drug use and face stigma, arrest, losing custody of their children or even violence from the wider community.” Any services tailored to women like the one Ms Mbalawa works for are key as are all peer-led services.
Ms Cook is concerned that if funding for communities and civil society support dries out, the entire harm reduction response may collapse. INPUD also warns that without immediate and strategic intervention, the world could witness a resurgence of HIV, hepatitis C, and overdose epidemics.
UNAIDS, UNODC and partners have been working with governments to encourage increasing domestic funding and mapping out sustainability plans. Central to these include having organisations led by people from the community participating as well as moving funds away from punitive approaches like criminalising drug use to reduce stigma, and inequalities.
“As countries look at new models for how to integrate specific HIV services tailored to serve the needs of people living with HIV or at risk of HIV, including people who use drugs, into general health services, this must include the integration of harm reduction services ” said Suki Beavers, UNAIDS Director of Equality and Rights for All. “And peer-led outreach is part of that equation.”
Mr Kwame stressed, “We need our voice to be heard so that people who inject drugs are part of the health agenda, and our needs are met.”
Related resources
Related


Feature Story
Impact of the US funding cuts: A snapshot on HIV commodity availability and management risks
01 May 2025
01 May 2025 01 May 2025The sudden pause and suspension of US Government foreign assistance has resulted in a multifactorial increase in the risks, challenges, and uncertainty related to HIV commodity[1] availability and management.
The analysis below presents findings from 56 countries (including 100% of PEPFAR-supported countries) which reported on the status of their HIV commodity stocks and supply chains between February and April 2025.[2]
The nature of PEPFAR support is different in all countries, and inclusion in this fact sheet does not necessarily mean that PEPFAR funded HIV commodities or supply chains specifically in that country, nor that all the issues faced are directly attributable to the US funding cuts.
This fact sheet reflects the situation based on information available as of 28 April 2025. Given the rapidly shifting situation, the information presented could change significantly as the situation evolves.
SUMMARY
- Funding for antiretrovirals often comes from diverse sources and their availability and effective delivery to those who need them depends on well-coordinated stakeholder efforts. Some 14% of countries reported six or less months of stock in at least 1 antiretroviral line.
- The degree of public uncertainty and concern over the continued availability of and access to free antiretroviral treatment has increased significantly. Some 18% of countries flagged public reactions to uncertainty, among others changes in individual behavior related to antiretroviral treatment.
- The most frequent variations in antiretroviral dispensation in countries include reductions in multi-month dispensing periods and in dispensing of emergency supplies, restricted switches to alternative antiretroviral regimens, closures of certain antiretroviral treatment dispensing points, and antiretroviral stock redistribution. Authorities have often sought to preempt or respond to rumors and uncertainty by proactively communicating about antiretroviral availability.
- Global Fund existing (or incoming) antiretroviral stocks are helping some countries ensure HIV commodity availability. National authorities are also securing supplementary domestic budget allocations to ensure HIV commodity availability and management.
- Despite the precarious situation faced by many community-led organizations because of the USG shift, they continue to play a central role in engaging and informing communities, addressing rumors, advocating for mitigation actions, and providing early warning on ARV availability, accessibility and cost.
- Significant disruptions affecting combination prevention commodities have been reported as a result of the USG shift. This is due to the dominant role played by PEPFAR in prevention commodity procurement, distribution or delivery in many countries. Some 23% of countries reported six or less months of condom or PrEP stocks.
- Around 21% of countries reported six or less months of stock in at least 1 HIV testing commodity. Careful monitoring of individualized country situations is necessary to mitigate any possible increase in stockout risks.
- Even when HIV commodities exist in-country, they may not always be reaching health facilities – creating patient-facing shortages that undermine trust in treatment continuity. Some 46% of countries reported supply chain management issues.
- The repercussions of the USG shift on the global HIV commodity markets should not be underestimated in the medium term. Sustained predictability in HIV commodity demand forecasts is essential to guarantee a stable supply, maintain prices, and ensure the availability of affordable generic medicines for national HIV responses.
[1] Commodities include ARVs, HIV tests, VL and other lab tests, early infant diagnosis reagents and supplies, as well as prevention commodities (including PrEP and condoms).
[2] The data analysed comes primarily from three sources: 1) Open-text reporting by UNAIDS country offices through the UNAIDS tool “Monitoring HIV Programmes’ Continuity Amidst US Shifts” for the period 5 February – 28 April 2025; 2) UNAIDS country office ad-hoc email updates for the period 18 -24 March and 16-23 April, and 3) UCO / RST consultations with national and regional PLHIV networks on 18-20 March.
Related resources
Related




Feature Story
From violence to funding cuts, Asia Pacific women living with HIV face old and new challenges
18 March 2025
18 March 2025 18 March 2025“In our country we are not the priority,” Daisy Cruz says plainly.
She is surrounded by other women living with HIV who agree. They share stories that are not often told about the epidemic in Asia and the Pacific. In a region where men living with the virus outnumber women roughly two to one, the issues of women and girls are often overlooked. They are all members of the International Community of Women Living with HIV Asia Pacific (ICWAP).
Eva Dewa was diagnosed in Yogyakarta, Indonesia in 2017.
“I came home seeking a safe space to share my sadness. At that time, I believed that my partner would support me. Instead, he blamed me,” she says.
Ms Dewa has survived intimate partner abuse. She knows she isn’t alone: “A lot of women either experience violence and get infected with HIV, or contract HIV and experience violence.”
She gave birth to twins two years before her diagnosis. During her pregnancy she was never screened. Unaware, she went on to breastfeed for a couple years. When she learned her status, it was she rather than healthcare staff who suggested the children be tested. One child was HIV negative. The other wasn’t.
UNAIDS estimates that under two-thirds (64%) of women living with HIV in Asia Pacific receive treatment to prevent transmission to their babies. This is far lower than the global average of 84%. Ms Dewa reflects that while HIV services for pregnant women are expanding, smaller cities and rural areas benefit more slowly.
Cathy Ketepa understands the challenge of reaching remote districts. Every day in her native Papua New Guinea, five infants are born with HIV. The epidemic there has doubled since 2010 with new infections among women increasing by a staggering 67%.
“Only around half of mothers living with HIV receive antiretroviral therapy,” says Ms Katepa . “We must bridge this gap to protect the health and future of our children.”
But while the women advocate for expanded services to reduce vertical transmission, they are adamant that their dignity, privacy and agency must be respected. The International Community of Women living with HIV (ICW) has conducted a global analysis of the reproductive coercion, mistreatment and abuse experienced by women living with HIV. The study found that across regions, during pregnancy and infant feeding women were most subjected to force.
“There is an issue with coercive practices,” said Sophie Bryon, ICW’s Director of Global Programmes. “We are talking about women being told not to have children, not to have another child, to terminate and being pressured to undergo sterilization. There is still denial of contraception and pressure to use certain kinds of contraception. There are issues ranging from verbal abuse to physical violence.”
There is also stigma. When Ms Cruz went to the hospital in Manila to give birth in 2001, a nurse on the ward loudly asked why she wasn’t breastfeeding.
“All the patients looked at me like there is something different,” she said.
There is a sense from these women that they’ve been ambushed by a threat they didn’t know existed. But having been hit, they will speak up for themselves, and for others.
Christina Montoya didn’t think it was possible for a woman like her to be infected. She was married and only had sex with her husband.
“We must be informed!” she declared. “And all our friends must be informed!”
11 years of ICWAP
ICWAP builds the capacity of women and girls living with HIV and women-led organizations in 18 Asia Pacific countries. It provides coaching and mentoring, ensuring women participate in Global Fund processes and are meaningfully engaged in community-led monitoring.
The organization was formed in 2014 to tackle the human rights violations and violence women living with HIV in the region experience, while removing barriers to treatment and care. Sita Shahi, its Regional Coordinator explains that the challenges can’t be tackled from a health angle alone.
“Women face a lot of stigma and discrimination. They also have an economic burden and are responsible for rearing children. There are so many intersecting issues,” she explained.
Now there are new challenges. ICWAP conducted an eleven-country survey on the impact of the United States development aid stop work order. It found that some country networks have either collapsed or scaled back, leaving women without crucial resources, including information about their rights and how to address gender-based violence or discrimination. There is also reduced access for many women who depended on community-based services for HIV or sexual and reproductive healthcare. While treatment is provided by government in most countries, many of the shuttered peer-led services were more accessible and friendly.
Some women who worked for US-supported programmes have lost their jobs, resulting in financial stress. ICWAP itself has been hard hit.
“We lost all funding. The core support we were receiving for managing staff and country interventions is gone. It is a devastating situation for us. There is now no funding to support our sisterhood at country level,” Ms Shahi explained.
UNAIDS has called for countries in Asia Pacific to support community-led HIV work including stigma and discrimination, adherence counselling, social support, monitoring and advocacy.
Related

Feature Story
The impact of the US funding freeze and cuts on Namibia’s civil society: A struggle for survival
10 March 2025
10 March 2025 10 March 2025A long-standing partnership threatened
For years, Namibia’s HIV response has been supported by US funding, particularly through the United States President's Emergency Plan for AIDS Relief (PEPFAR). These programmes have provided lifesaving drugs for HIV treatment, prevention services, and essential socio-economic empowerment initiatives, especially for adolescent girls and young women and the most marginalized and at-risk groups.
However, given the recent decisions by the US to freeze and cut foreign assistance, Namibians are struggling to fill the funding gaps. An emergency humanitarian waiver issued by the US Government allowed for funding to flow to some projects and organisations (government and non-governmental) – but as the funds were not transferred into their accounts, they are faced with serious cash-flow challenges and were at risk of contravening the labour laws of the country.
The US funding freeze has had a particularly devastating impact on community groups supporting the most vulnerable populations. In Katutura, for example, adolescent mothers who were benefiting from HIV prevention and socio-economic empowerment programmes saw their support vanish overnight. “For the past year, these adolescent girls and young mothers have received psychosocial support, life-skills education and socioeconomic empowerment, but all these abruptly stopped, and their livelihoods are at risk,” said a representative of Lidar Community Foundation, a youth empowerment programme for orphaned and vulnerable girls in Katutra-Central, Windhoek. The loss of these critical services jeopardizes not only health outcomes but the livelihoods of some of Namibia’s most marginalized individuals.
A fragile civil society left to cope
Namibia’s civil society had long been reliant on external funding, with the US and the Global Fund being major contributors of the civil society-led HIV programmes. The US funding freeze has left civil society organizations working on HIV prevention, human rights and youth empowerment issues in a precarious position, unable to provide essential services and continue operations, forcing them to lay off their staff, scale back their operations, or even completely close their programmes.
This situation is overwhelmingly affecting the most vulnerable and marginalized groups in Namibian society. Key populations—such as transgender people, sex workers, and people living with HIV—were already facing discrimination in accessing essential services. With the end of the US support, these groups are now at an even greater disadvantage. “This is such an emotional time,” said Kholi Buthelezi of the Sisonke National Sex Workers Movement in South Africa. “It triggers memories from that pre-ART times in the HIV era, when all we had was hope but no concrete resources to act on the challenges."
Young women, particularly adolescent girls, are another demographic severely affected by the US funding freeze. Many had been participating in HIV prevention programmes or socio-economic initiatives aimed at empowering them. These cuts have halted progress, leaving them more vulnerable to HIV and other socio-economic challenges.
The need for collective action
A meeting co-hosted by UNAIDS on 7 February to review the implications and impact of the U.S. funding freeze, highlighted the need for collective action to help Namibia’s civil society weather this storm. Many civil society organizations were left unsure of how to engage at the national and international levels to advocate for their cause due to a lack of clear communication and support from the Namibian government. “We wonder if civil society organizations will be consulted on how the country is going to respond to this funding challenge, so that we also contribute to the solutions,” said one participant, highlighting the need for civil society to be closely involved in the response to this unprecedented challenge.
Exploring alternative funding sources, including from the private sector and other partners, was deemed essential. All partners called for a united front, with CSOs coming together not only to advocate for the reversal of the Executive Orders but also to explore ways to ensure continued support for Namibia’s most vulnerable populations.
As a way forward, CSOs were urged to complete a rapid assessment tool to better understand the immediate effects of the funding cuts, as data collection and monitoring are crucial in advocating for the continued support of affected communities and developing detailed action plans and strategies.
Strengthening partnerships, supporting mental health and psychosocial well-being, and engaging with the government are also key to ensuring that Namibia’s civil society could survive in these uncertain times.
Despite all, Namibia’s civil society remains determined. While the challenges are significant, the collective power of advocacy, solidarity, and collaboration offers a glimmer of hope for the future. It is through these unified efforts that Namibia’s most vulnerable communities may continue to receive the care, support, and recognition they deserve.
Region/country
Related


Feature Story
Three Years On: From crisis to prospective recovery
20 February 2025
20 February 2025 20 February 2025Ukraine has been reeling from three years of war since 24 February 2022. One out of two Ukrainians have been affected by the conflict and more than 12 million people need humanitarian assistance and protection while another 6 million have still not been able to return to their homes.
A war-driven economic crisis has severely impacted healthcare funding, putting access to HIV services at risk. With HIV services entirely dependent on external aid and humanitarian support that is becoming increasingly unstable, the uncertainty of the continuity of U.S. funding has further worsened an already dire situation in Ukraine. In January, the new U.S. Administration froze all foreign assistance for a 90-day period. A waiver to allow life-saving services was subsequently issued allowing support for some HIV services.
The U.S. President's Emergency Plan for AIDS Relief (PEPFAR) contributed US$15.6 million to the HIV response in Ukraine during 2023 and 2024. This includes $11 million for antiretroviral therapy and $2 million for various types of rapid test kits, while the rest was used for laboratory expenses.
UNAIDS and partners estimate that 92,840 Ukrainian people could see their HIV treatment disrupted if U.S. funding was to be entirely cut – that is 78% of all people living with HIV on treatment. In addition, stocks of life-saving treatment and HIV prevention drugs are low, with people only getting three versus six months of drug supply.
The threat of a potential financial void left by the U.S. is forcing Ukraine’s health system to search for alternative sources of funding. From Global Fund reprogramming to private sector donations to bulk medicine offers from pharmaceutical companies. Many options are being explored to patch together a lifeline. However, even collectively these efforts may not be enough to fill the PEPFAR gap should the U.S. permanently withdraw its support.
There are hopeful signs of recovery like HIV testing increased 23% last year compared to 2023 but obtaining comprehensive epidemiological and clinical data remains difficult.
This inevitably affects the accuracy of overall assessments due to the ongoing conflict, loss of administrative control in certain regions, missing persons, and mass displacement.
Despite ongoing challenges, Ukraine remains committed to the HIV response, supported by a strong coalition of government, civil society, international organizations, and donors. The UNAIDS Secretariat, Co-sponsors, UN agencies, and member states continue working together to ensure essential services for women, people living with HIV, and key populations, reinforcing the response's sustainability even in the face of adversity.
Related information
Special page
Region/country
Related


Feature Story
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
18 February 2025
18 February 2025 18 February 2025On 20 January 2025 the United States announced a 90-day freeze on US foreign aid which has had a devastating impact on people living with and affected by HIV, on the people and organizations supporting them and on the global response to HIV as a whole.
Community organizations have been particularly impacted by the freeze in funding. Community healthcare workers are losing their jobs, clinics are having to be shut down and, as a result, people in need of HIV testing or prevention or who are living with HIV and dependent on daily antiretroviral medicine are unable to access the life-saving HIV services they need.
On 10 February, UNAIDS convened an emergency meeting with community organizations to monitor the impact of the unfolding crisis. Community groups reported that HIV services around the world are facing serious challenges. Some are grinding to a halt. Supplies of antiretroviral medication, pre-exposure prophylaxis (PrEP), post-exposure prophylaxis (PEP) and condoms have been disrupted, leaving many without essential tools of HIV treatment and prevention.
HIV testing kits are increasingly scarce and outreach services – essential for connecting people in need of HIV testing – are being suspended. As a result, HIV and sexually transmitted infection testing are disrupted, threatening detection and prevention efforts.
“The damage is immediate and severe,” said one advocate. “People who rely on [U.S.-funded] programmes for [safety and] survival are suddenly left with nothing.”
The US pause in administering foreign assistance while it reviews recipients is not just a bureaucratic delay; it is a direct threat to continued progress against AIDS and will quickly erode decades of hard-won gains in the global HIV response. It will destroy many community organizations without which the world cannot close the gaps in HIV testing, prevention and treatment.
The US Government has invested more than US$ 100 billion to date in the global fight against AIDS with the US accounting for around 73% of donor funding for HIV worldwide; millions of people at risk for and living with HIV rely on US funded clinics to stay healthy in the face of HIV.
Community-led data reveals community organizations are bearing the brunt of the pause
A survey conducted by the Uganda Key Populations Consortium found that 97% of respondents reported negative effects on their HIV service due to the freeze on US foreign assistance. A staggering 43% of organizations supporting key populations surveyed said they relied on US funding for at least 76% of their budgets.
Another joint survey by Aidsfonds, the Global Network of People Living with HIV (GNP+), and the Robert Carr Fund found similarly worrying results. Of 564 organizations surveyed across 25 countries, 95% reported direct impacts from the US funding freeze. 43% of programmes have paused implementation, while 35% have fully suspended operations.
“The results are alarming,” said Mark Vermeulen, Director of Aidsfonds. “More than half (57%) of the organizations estimate that this crisis will impact more than a million people. The longer these disruptions persist, the greater the risk of a new generation of preventable HIV infections. This threatens to undo the hard-earned progress in reducing new infections among children.” (New HIV infections among children had been reduced by 62% from 2010 to 2023, largely thanks to investment and commitment from the US Government).
It’s not just people living with or at risk for HIV that face an existential threat
The financial void left by the US aid freeze of its foreign assistance is forcing community groups to fire employees and/or to close up shop entirely. Many community organizations do not have sufficient funding reserves to stay afloat through the 90-day (or perhaps longer) period of no US funding.
“The leadership of national networks of people living with HIV have been forced to let go of community cadre staff- peer educators, adherence counselors, community health facilitators, and mentor mothers,” said Florence Anam, Co-executive Director of GNP+.
GNP+ recently convened with leaders from national and regional networks of people living with HIV and released a statement with the main concerns.
“These organizations are not a luxury – they are critical for ending AIDS,” said Christine Stegling, Deputy Executive Director, UNAIDS. “Serving as advocates, peer educators, care providers and watchdogs, community-led organizations ensure that lifesaving HIV testing, prevention and treatment reaches those most in need.”
Many organizations have spent years garnering the trust of the communities they serve. If these organizations disappear, even if others replace them one day, it will take years to reestablish the bonds of trust that allow them to be so instrumental in encouraging people to seek HIV care.
In a joint survey by Aidsfonds, GNP+ and the Robert Carr Fund 22% of organizations reported increased experiences of discrimination, including reports of discrimination within healthcare settings, where people faced barriers to accessing care.
LGBTQ+ communities in need of HIV testing, prevention and treatment fear increased risks of violence and discrimination as funding for protective services – led by HIV community groups – disappear.
Since the earliest days of the AIDS pandemic, communities and community-led services have been instrumental in ensuring equitable, accessible HIV testing, prevention and treatment – as well as the supportive services that make all three possible.
Communities have been at the forefront, driving the delivery of comprehensive care, life-saving treatment and offering regular monitoring and prevention services and psychosocial support. Their unwavering dedication has not only saved millions of lives but also reshaped the trajectory of the AIDS pandemic. Their leadership and work on HIV are a model for all other responses to communicable diseases.
By paralyzing frontline response efforts led by community groups, the US decision to freeze funding is weakening health systems across the Global South. The freeze not only jeopardizes precious gains made to date against HIV – it also threatens to usher in a new wave of entirely preventable HIV infections and AIDS-related deaths.
The community groups stressed that this crisis extends beyond HIV treatment. The funding cuts impact efforts to provide clean water, basic education and to prevent human trafficking of girls. The loss of funding is dismantling the fragile safety net that has been built over decades around the world
“We are deeply concerned about the sustainability of the HIV response, particularly support for key populations, HIV prevention, human rights and community led responses. We are re-orienting our own efforts to support the communities and organizations that are both bearing the brunt of the loss of funding and facing targeted attacks on their rights and their very lives,” said John Plastow, Executive Director of Frontline AIDS, a global partnership, headquartered in the UK and South Africa, that works with 60 partners across 100 countries around the world. Over 20 of their partners have said they are affected by the US foreign aid freeze.
Since the US funding freeze on foreign assistance was announced, UNAIDS has conducted daily assessments led by its regional and country teams to track disruptions and to relay urgent needs to donors and to governments of affected countries. At country and regional levels, UNAIDS has also been convening people living with HIV and other affected communities to assess the impact and discuss mitigation measures. For the latest updates: Impact of recent U.S. shifts on the global HIV response - The global impact of PEPFAR to date | UNAIDS
UNAIDS stands in solidarity with community leaders calling on the US, other donors and governments of affected countries to step in before irreversible damage is done. UNAIDS and communities call on the US to maintain its global leadership on, and unparalleled support for the global response to AIDS. Without immediate intervention, decades of progress in the global HIV response will be undone, leaving the world on the precipice of a public health disaster that we have the power and tools to avert.
Related

Feature Story
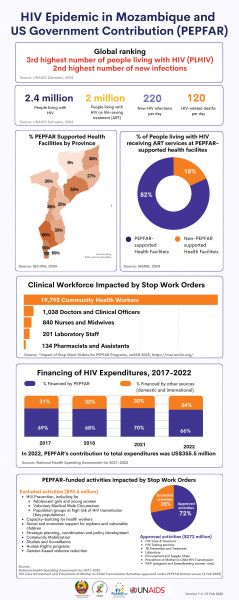
HIV Epidemic in Mozambique and US Government Contribution (PEPFAR)
18 February 2025
18 February 2025 18 February 2025

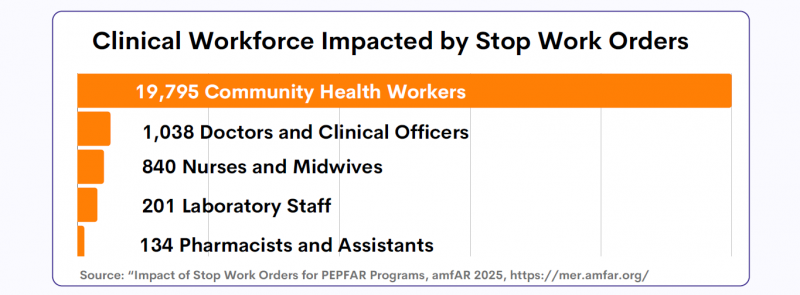
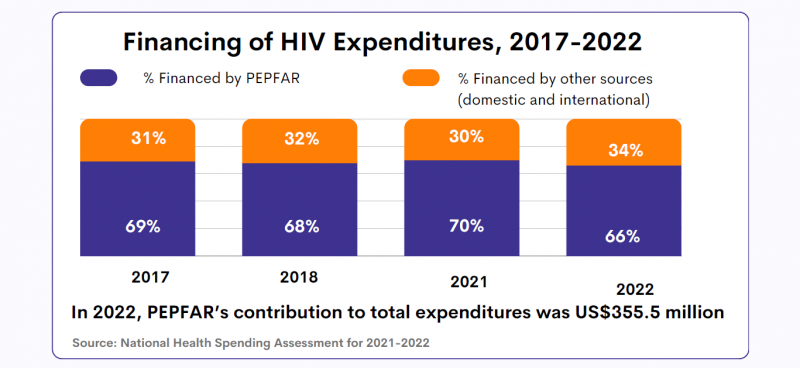


HIV epidemic in Mozambique and US Government contribution (PEPFAR)
Region/country
Related


Feature Story
A crisis unfolding: hard-won progress in Ethiopia’s HIV response at risk
13 February 2025
13 February 2025 13 February 2025Ethiopia has made significant progress in its HIV response in recent years and is on track to reach the UNAIDS 95-95-95 targets with 90% of people living with HIV in the country being aware of their HIV status; 94% of those diagnosed with HIV receiving antiretroviral (ARV) therapy; and 96% of people on ARV therapy achieving viral suppression.
But now, that progress is at risk. The recent pause in United States foreign assistance poses a direct threat to the lives and well-being of thousands of people living with HIV in Ethiopia and millions globally. Critical services are grinding to a halt, leaving people who rely on them facing an uncertain and dangerous future.
Ethiopia is heavily reliant on external funding for its AIDS response. PEPFAR provides 53% of HIV funding in the country. In 2023, UNAIDS’ estimates show that there were 610 000 people living with HIV in Ethiopia, 510 000 of whom were accessing antiretroviral treatment.
For women living with HIV, uncertainty is growing. Limited and unclear communication from healthcare providers and policymakers has left them in the dark about treatment changes, medication availability, and service disruptions. With no clear answers, they are forced to rely on rumors, fueling fear and anxiety.
“We don’t know what’s happening. Are services being cut permanently? Will we still get our medication next month? No one is telling us anything,” one woman shared.
To make matters worse, case workers and counsellors—once a vital source of medical and emotional support—are disappearing. These professionals were more than healthcare providers; they were trusted confidants who ensured women received care in a stigma-free environment. Their absence is leaving many feeling abandoned.
“They understood our struggles, checked in on us, and made sure we had what we needed,” another woman explained. “Without them, we feel forgotten.”
As services become increasingly unreliable, distress and fear are taking hold.
Shortages and desperate measures
Funding cuts bring shortages, and for women living with HIV, the fear of running out of medication is overwhelming. Access to antiretroviral therapy (ART) is essential—it keeps people alive. Yet many are already facing supply disruptions, and whispers of medication shortages are spreading panic.
“If I can’t get my medicine, what happens to me?” one woman asked. Women living with HIV who have been healthy for years now fear an uncertain future where their treatment is no longer guaranteed. People living with HIV who do not access antiretroviral therapy will eventually develop AIDS and die. To cope, many have resorted to stockpiling medication, traveling long distances and spending entire days at clinics in hopes of securing extra supplies. While understandable, this survival strategy comes at a heavy cost—disrupting work, family life, and daily routines. No one should have to live in fear of their next refill. The urgent need for stable, uninterrupted HIV treatment cannot be overstated.
Adding to the crisis, shortages extend beyond medication. The dwindling supply of test kits, including viral load tests, is threatening the future of diagnosis and monitoring. These tests are crucial to ensure that people living with HIV maintain undetectable viral levels, reducing transmission risks and protecting their health.
Fears have also been expressed around the availability of medications for HIV prevention, particularly for the prevention of vertical transmission of HIV. If the current pause in the supply of medical resources continues, the availability of these vital medications could be severely compromised, putting the lives of women and children at even greater risk. For women living with HIV who are pregnant, a lack of lifesaving medications for themselves also means their children can be born with HIV even though this is entirely preventable.
Without test kits and prevention measures, undiagnosed and untreated cases could rise dangerously. “We can’t afford to go backward,” one woman said.
A Plea for Action
The voices of these women reveal a stark and urgent reality—funding cuts have left people living with HIV in a state of uncertainty, with no clear path forward.
"Urgent intervention is needed,” stressed Tina Boonto, Country Director for UNAIDS Ethiopia. “UNAIDS is gathering information and developing funding solutions to address the shortfall, with proposals for both the government and external partners to ensure continuity of critical services. We hope Ethiopia's government will step up and lead in covering these essential services. We must act now to safeguard gains that have been made and succeed in securing sustainable support to people living with HIV."
While the future remains uncertain, one thing is clear: without swift action, the hard-won progress in Ethiopia’s HIV response is at risk.