

Update
Statement from UNAIDS on the decision of the High Court of St. Vincent and the Grenadines to uphold discriminatory and harmful laws
25 February 2024
25 February 2024 25 February 2024UNAIDS is concerned about the impact on peoples’ health and rights following the decision of the High Court of St. Vincent and the Grenadines regarding sections 146 and 148 of the Criminal Code, which upholds discriminatory and harmful laws against LGBTQ people.
On Friday, February 16, 2024, the High Court, in an oral delivery, denied the claim by two Vincentian nationals, who reside outside of the country, that sections 146 and 148 of the Criminal Code criminalising buggery between any two persons with a penalty of up to 10 years imprisonment, violate the fundamental rights to privacy, personal liberty, freedom of conscience, freedom of expression and protection from discrimination. The Court dismissed in their entirety all claims by the two Claimants and awarded the sum of EC$7,500 prescribed costs to the Attorney General to be paid by each of the Claimants.
In the written decision published February 22, 2024, the Court in dismissing the consolidated claims of Javin Johnson and Sean MacLeish held that the Claimants had failed to establish on the evidence, a present or existing breach of any alleged rights due to lack of locus standi (the requisite standing to invoke a review by the Court) as the Claimants do not reside in the State and had not for years prior to the filing of the claims.
UNAIDS is particularly concerned that the judgment referred to protecting public health and tackling the HIV epidemic as justifying punitive anti-LGTBQ laws, because the evidence shows that such laws hinder efforts to protect public health and tackle the HIV epidemic. At paragraph 267 of the judgment the court asserted:
“to my mind the thought of a public health crisis occasioned by an unstemmed deluge of new HIV cases is a real and serious concern which reasonably justifies a public health response of the kind embedded in the challenged provisions”.
In fact, studies show that these laws have negative health outcomes. A punitive legal environment, including criminalisation of same sex relationships, drives people underground and away from vital health services, including HIV prevention, testing, treatment, and care. To achieve the goal of ending AIDS as a public health threat by 2030, it is vital to ensure that everyone has equal access to essential services without fear, stigma or discrimination.
UNAIDS has estimated that not achieving decriminalization of key populations in all countries would result in about 750 000 cumulative new HIV infections from 2020 to 2030.
The decision made in the High Court of St. Vincent and the Grenadines stands in stark contrast to the rulings in Belize, Guyana, Trinidad and Tobago, Antigua and Barbuda, St. Kitts and Nevis and Barbados where the courts ruled that laws which criminalise persons based on sexual orientation and gender identity violate the protected rights to dignity, privacy, personal liberty, freedom of conscience, freedom of expression and protection from discrimination.
Regardless of the outcome of this court decision, UNAIDS holds hope that the courts will serve as a vital last resort for social justice, the protection of human rights and the advancement of public health for improved health and wellbeing for all. UNAIDS work to end AIDS and to leave no one behind will continue in partnership with communities and with all branches of government, including the courts.
Punitive laws obstruct the end of AIDS and ultimately hurt everyone’s health. As we prepare for observance of the tenth anniversary of Zero Discrimination Day on March 1st, 2024, we pay tribute to the courage of communities, and call on all duty bearers to protect the health of all by protecting the human rights for all.
NOTE FOR THE EDITORS:
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals.
ZERO DISCRIMINATION DAY
March 1st this year is the tenth anniversary of Zero Discrimination Day. Upholding everyone’s rights is the responsibility of us all. Everyone can play a part in ending discrimination. On 1 March, and across the whole month of March, events, activities and messages will remind the world of this vital lesson and call to action: to protect everyone’s health, protect everyone’s rights. #ZeroDiscrimination
Contact
UNAIDS Multi-country Office for the CaribbeanRichard Amenyah, Multi-country Director
amenyahr@unaids.org
UNAIDS Latin America and Caribbean
Daniel de Castro, Regional Communications and Advocacy Adviser
tel. +507 6998 3175
decastrod@unaids.org
Our work
Region/country




Update
UNAIDS supports China to play a bigger role to end AIDS at home and globally
19 December 2023
19 December 2023 19 December 2023The collaboration between UNAIDS and China was the focus of a consultation that took place on the sidelines of the 53 meeting of the UNAIDS Programme Coordinating Board.
The consultation brought together members of UNAIDS senior leadership, representatives from WHO and the Global Fund, and Chinese health authorities, to develop a bilateral strategic action framework and a memorandum of understanding (MoU) to expand and quicken the pace of the HIV response in China and globally.
“We are at a critical time in the HIV response, and we have a great opportunity that the Chinese delegation is here for our Programme Coordinating Board meeting”, said Rosemary Museminali, UNAIDS Director of the Office of Multilateral Systems, in her introductions.
Building on China’s long-standing international cooperation on health, participants acknowledged the potential to engage China more prominently in global efforts to end AIDS, especially under the South-South Cooperation framework and in line with China’s development schemes including Belt and Road Initiative and Global Development Initiative which aim at promoting global development and helping other developing countries to achieve the Sustainable Development Goals.
UNAIDS pointed out that China has a pivotal role to play in promoting local production of medicines and health commodities. At the same time, there is a need to build and expand relationships with other government departments to leverage all available resources to implement international best practices, promote access to quality services and support civil society’s engagement in HIV response.
Ren Minghui, Director of Global Health Institute of Peking University Health Science Center, is helping UNAIDS develop the framework and MoU. He outlined some initial key points in positioning HIV in the overall health strategy and broader development agenda. He also highlighted China’s specific context, including its increased contributions to global health and the HIV response, China-led initiatives and South-South collaboration, as well as a special call from President Xi to build a community with a shared and healthy future for mankind.
“There are important elements for China and for the global AIDS response, but for these we need to address equality and have a multisectoral mechanism,” said Ren Minghui.
Participants shared ideas on how to facilitate the development process of the two documents, which will take place over the next six months.
Prior to the consultation meeting, UNAIDS Executive Director Winnie Byanyima met with the Chinese delegation for the PCB meeting. She congratulated China’s progress in HIV prevention and treatment and urged more efforts to be made to address challenges such as providing quality treatment for people living with HIV, increasing testing, improving HIV prevention and eliminating stigma and discrimination.
“I hope China can play a bigger role to end AIDS at home and globally”, Winnie Byanyima told the delegation.
Region/country


Update
Upholding UNAIDS responsibility to communities
24 February 2023
24 February 2023 24 February 2023UNAIDS holds a duty to serve and safeguard people in need.
We are a Joint Programme which works on the frontlines, in partnership with civil society, to protect and promote the human rights of people living with, affected by, and at risk of HIV. We place the highest priority on our safeguarding responsibility.
The online activity and comments of a temporary staff member were unacceptable, contrary to our values and responsibilities, and put at risk our vital mission to serve communities.
The temporary staff member’s contract has been terminated.
We are deeply concerned at gaps in safeguarding, contracting, recruitment, and management processes which this case demonstrated. We are taking action to close these gaps and are instituting an external review to identify further actions needed.
UNAIDS is determined that we live up to the trust of the people we serve.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.




Update
Former UNAIDS Country Director, Michel de Groulard, remembered for championing communities
10 October 2022
10 October 2022 10 October 2022UNAIDS is saddened by the passing of long-time HIV and public health adviser to the Caribbean, Dr. Michel de Groulard. Michel had more than 30 years’ experience in International Public Health, with around 25 years dedicated to HIV.
Michel was a French citizen who made the Caribbean his home. He lived in Trinidad and Tobago for several years and up to the time of his passing.
A medical doctor by training, Michel worked on several public health projects for the French Ministry of Foreign Affairs and provided healthcare to remote, desert villages in Mauritania and Cameroon. He also served as a Public Health Officer in the Grenada Health Ministry and an HIV Project Manager at the Caribbean Epidemiology Centre.
Michel joined UNAIDS in 2001 as a Senior Partnerships Adviser. He went on to serve the Caribbean region in a number of positions with UNAIDS, including Senior Program Adviser to the region for more than seven years. He had just last month concluded a two-year appointment as interim Country Director for the Guyana/Suriname office which he opened in Georgetown in 2005.
In his HIV work over the years, he continuously placed a strong emphasis on the role of civil society at all levels of the response to address risk and vulnerability, gender issues and barriers to access services. Michel provided technical support for the creation of the Caribbean Network of People living with HIV in 1996 and the establishment of the Caribbean Vulnerable Communities Coalition in 2005. For several years he was Vice Chair of Community Actions Resource, Trinidad and Tobago’s oldest organization serving people living with HIV.
Above all Michel was a champion for the marginalized and excluded, especially people living with HIV and key populations. He ensured that communities’ concerns and voices were put at the centre of planning and advocacy. He is remembered by civil society and for championing their critical importance in shaping public policy and delivering services.
Michel never truly retired. Always energetic and committed, he took on several challenges following his initial departure from UNAIDS in 2013. This included the role of Regional Manager for the USAID/PEPFAR LINKAGES programme for the Eastern and Southern Caribbean. He also volunteered with the Alliance Française in Port of Spain.
His interests in epidemiology and public health were enduring. Since the start of the COVID-19 pandemic, for example, he compiled and disseminated daily country and regional graphs tracking new infections and deaths in the Caribbean. His nightly WhatsApp messages to friends and colleagues continued until the night before his passing.
Michel loved to cook and would often entertain friends at home with his famous quiche. He encouraged us all to eat healthily and work out.
Michel served with distinction as an international civil servant, and he touched many lives. He was a real champion for ending inequalities. We have lost a great brother, a wonderful human being and a very committed professional with exceptional leadership skills and understanding of human rights and inclusion. We extend our deepest condolences to his family. We shall miss him.

Update
UNAIDS Country Director in Nigeria shares how lessons from the AIDS response apply to the Monkeypox response
24 August 2022
24 August 2022 24 August 2022Dr Leo Zekeng, UNAIDS Country Director and Representative in Nigeria, has shared how lessons from the AIDS response apply to the Monkeypox response.
Dr Zekeng said:
“Monkeypox is endemic in Nigeria, and in recent weeks there has been a significant increase in suspected and confirmed cases. The Nigeria Center for Disease Control (NCDC)’s most recently published sitrep (7th August 2022) indicates that in 2022 there have been over 473 suspected Monkeypox cases (407 of which are since 30th May), of which have been 172 confirmed (151 of which are since 30th May). In the most recent weekly data published (1st to 7th August), 60 suspected cases were recorded in one week, out of which 15 were confirmed.
The Nigerian government, civil society organisations, development partners and the UN are working together to respond to the increase of suspected and confirmed Monkeypox cases in Nigeria. On 26th May 2022, the Nigeria Centre for Disease Control and Prevention (NCDC) activated a national multisectoral Emergency Operations Centre for Monkeypox to strengthen and coordinate ongoing response activities in-country while contributing to the global response.
Lessons we have learnt in the AIDS response apply to the Monkeypox response too. The Monkeypox response in Nigeria is being impacted by both social stigma and by global inequality in access to essential medicines, including vaccines.
Local staff in the most affected states have reported that stigma, connected with commentary from across the world blaming gay people for Monkeypox, is discouraging some people from seeking care. Local staff report that there have been situations of people being too afraid to access medical care because of stigma. State Health officials are working to ensure that staff at health clinics are sensitized to break down such stigma, and not to reinforce it. State Ministry of Health officials are also embarking on community sensitization on Monkeypox, emphasizing identification of symptoms, prevention, and the need to get tested.
The scarcity of key medicines is also holding back Nigeria's Monkeypox response. There is a need to support expansion of the supply of medicines, equipment, and sample collection materials. Unlike the US and EU, Nigeria does not have any supply of vaccines for Monkeypox. This brings amongst people in affected areas a sense of frustration that they have been left behind by the world. This inequality in access to vaccines and other key medicines must be urgently put right by sharing doses, sharing production rights and sharing know-how.
Support in efforts to challenge stigma, and in enabling access to essential medicines, are key to ensuring that everyone impacted by Monkeypox in Nigeria gets the care they need. Support for the response in Nigeria is essential for the success of the global response."
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Region/country
Related


Update
Fifth episode of UNAIDS podcast series ‘Against the Odds’ released
05 October 2022
05 October 2022 05 October 2022Our guest this week is David Gere, who calls himself an ‘Artivist.’ He is that rare being, a creative artist and writer, academic and activist, who crosses traditional boundaries with ease. David remembers the experience of seeing close friends affected and dying of AIDS in 1980s San Francisco, and his growing conviction that it might be possible to use art to change behaviours and attitudes, ‘I really thought of art as being about expression, getting things out, having a full life … it was about beauty … yes, it was about beauty, but it was also about Action.’
David started his professional career as an arts critic in the San Francisco Bay area, was co-chair of the International Dance Critics Association, and is the founding director of the Art and Global Health Center at UCLA, the University of California, Los Angeles. He is a writer and essayist with many publications to his name, including the prize-winning book How to Make Dances in an Epidemic: Tracking Choreography in the Age of AIDS. And he has created and curated a series of exhibitions and projects, showcasing art that shines a light on public health issues, especially the HIV/AIDS epidemic. His most recent endeavor is the multi-media photo-storytelling project ‘Through Positive Eyes.’
Can artistic work have a real impact on attitudes and prejudices? And if so, how? David reflects on what happened when the hero in a popular soap opera in India reveals himself as HIV positive, and on handing cameras to HIV positive people to tell their own stories.
More about David here
Through Positive Eyes photo storytelling project here
UNAIDS is pleased to announce the launch of a podcast series called ‘Against the Odds.’ This is a series of frank conversations with guests whose lives have been touched in many different ways by HIV. We find out about the challenges they’ve faced, and what inspires them to strive for what may seem impossible goals.
In this brand-new podcast, UNAIDS asks some extraordinary people what made them winners when all the odds were stacked against them. How did they overcome life changing challenges? And what have they learned along the way?
Featured are a prize-winning photographer, a top-level lawyer, committed social activists, artists and creators - all amazing individuals who are passionate about what they do. All have been affected by HIV and AIDS, either directly or indirectly, and all share personal stories of challenge and survival.
At UNAIDS, we guide and bring together the global effort to end AIDS. What we’ve learnt in the HIV response is that progress is never given, it is won. It depends on the power of people challenging the people in power.
Brought to you by UNAIDS, you can listen to ‘Against the Odds’ wherever you get your podcasts. If you can, do please subscribe so you’ll get the next episode delivered straight to your inbox.
Listen on:
- UNAIDS https://www.unaids.org/en/podcasts
- SPOTIFY https://open.spotify.com/show/4dledFQe4BqFndhoJqeFCd
- APPLE https://podcasts.apple.com/ch/podcast/against-the-odds/id1635168572?l=en
- AMAZON MUSIC https://music.amazon.com/podcasts/265102e0-836a-4467-a0dd-ba5b30da47ee/against-the-odds
- DEEZER https://www.deezer.com/us/show/3894807
- PLAYER FM https://player.fm/series/against-the-odds-3373661
- PODCAST INDEX https://podcastindex.org/podcast/5590860
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Powell Media
Powell Media specializes in podcast production services in the heart of international Geneva. Learn more at PowellMedia.ch
Listen on:

Update
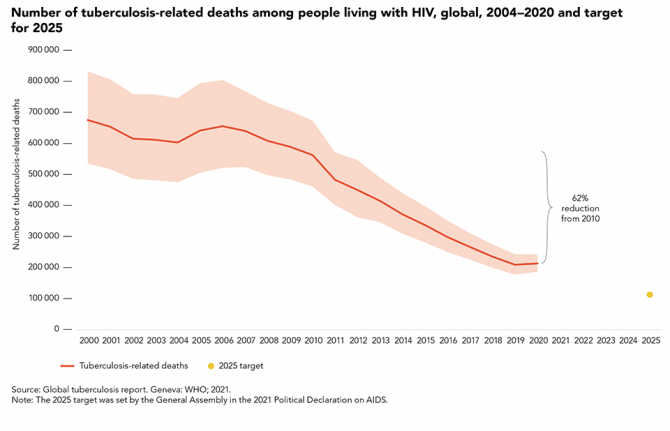
TB disease and deaths declining among people living with HIV, but there have been some reversals due to the COVID-19 pandemic
23 March 2022
23 March 2022 23 March 2022Tuberculosis (TB) is a preventable and treatable disease, yet it continues to claim millions of lives each year and remains the leading cause of death among people living with HIV.
While progress has been achieved in recent years, there have been some reversals due to the COVID-19 pandemic. There has been a steady decline in the estimated number of incident TB cases among people living with HIV. However, just 48% of the estimated 787 000 TB episodes globally among people living with HIV in 2020 were diagnosed and notified. This reflects a decline for the first time since 2004 in the percentage of estimated incident TB cases among people living with HIV that were notified, from 56% in 2019.
Fully 88% of people living with HIV who were diagnosed and notified with TB were provided with antiretroviral therapy, corresponding to 42% of people living with HIV estimated to have developed TB in 2020. While until 2019 there had been a gradual increase in the number of TB patients living with HIV who were on antiretroviral therapy, 2020 data reflect a decline in the percentage of incident TB cases of people living with HIV who received antiretroviral therapy for the first time since 2004, from 49%. There was also a decline in the number of people living with HIV who received TB preventive treatment between 2019 and 2020.
While the United Nations High-Level Meeting on Tuberculosis target of 6 million people living with HIV having received TB preventive treatment between 2018 and 2022 has been reached ahead of time, with 7.5 million people living with HIV having received TB preventive treatment between 2018 and 2020, there is still a long way to go to reach the 2025 target of 90% of people living with HIV having received TB preventive treatment.
There were an estimated 214 000 TB-related deaths in 2020 among people living with HIV, a 62% reduction since 2010, when TB claimed the lives of 563 000 people living with HIV. For the first time since 2006, there was an increase in the estimated number of TB-related deaths among people living with HIV between 2019 and 2020, from an estimated 209 000. The 2021 United Nations Political Declaration on AIDS requires an 80% reduction by 2025 (compared to a 2010 baseline).
Related

Update
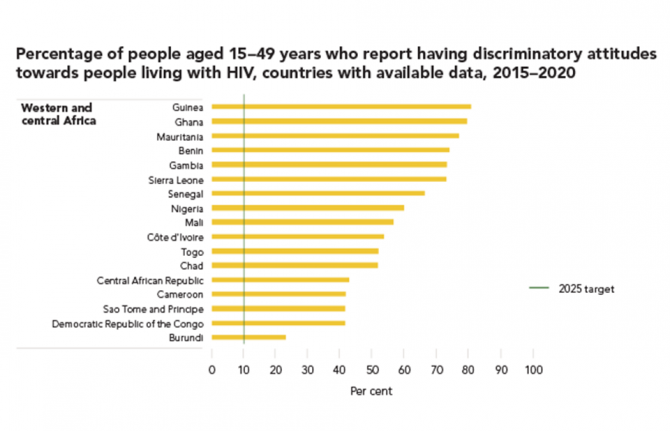
Discriminatory attitudes remain common
14 March 2022
14 March 2022 14 March 2022The prevalence of discriminatory attitudes towards people living with HIV varies widely. Across nearly all regions, there are countries where large proportions of adults continue to hold discriminatory attitudes towards people living with HIV.
In 52 of 58 countries with recent population-based survey data, more than 25% of people aged 15 to 49 years reported holding discriminatory attitudes towards people living with HIV, and more than 50% held discriminatory attitudes in 36 of 58 countries.
Our work

Update
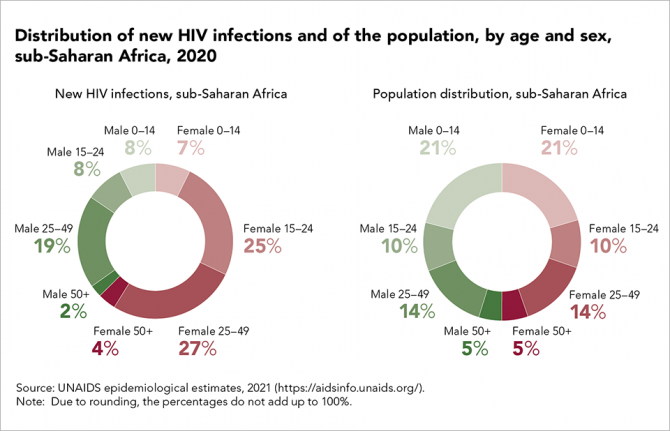
Women and girls carry the heaviest HIV burden in sub-Saharan Africa
07 March 2022
07 March 2022 07 March 2022Gender inequality and discrimination robs women and girls of their fundamental human rights, including the right to education, health and economic opportunities. The resulting disempowerment also denies women and girls sexual autonomy, decision-making power, dignity and safety.
These impacts are most pronounced in sub-Saharan Africa, where adolescent girls and young women (aged 15 to 24 years) accounted for 25% of HIV infections in 2020, despite representing just 10% of the population.

Update
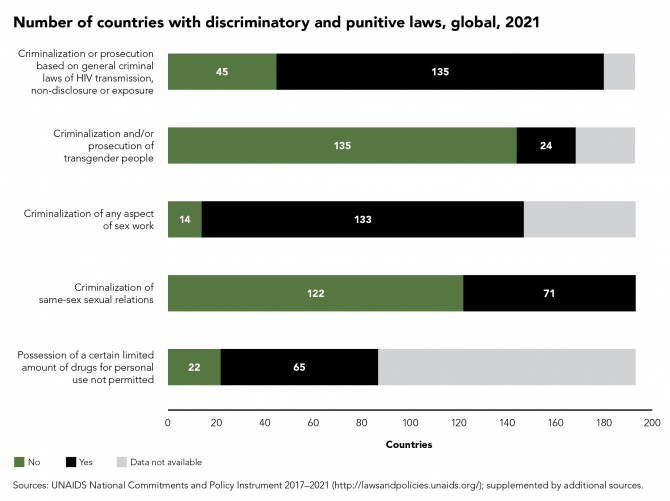
Discriminatory and punitive laws alarmingly common
28 February 2022
28 February 2022 28 February 2022Criminalization of same-sex sexual relations, sex work, drug possession and use, and HIV exposure, non-disclosure and transmission have been shown to block HIV service access and increase HIV risk.
Countries that criminalize key populations saw less progress towards HIV testing and treatment targets over the past five years—with significantly lower percentages of people living with HIV knowing their HIV status and achieving viral suppression than in countries that avoided criminalization. Even greater gains were achieved in countries where laws have advanced human rights protections, particularly those that protected rights to non-discrimination and responded to gender-based violence. Despite this compelling evidence, discriminatory and punitive laws remain alarmingly common.



















