Feature Story
Stranded in Nepal without HIV medicine
15 March 2021
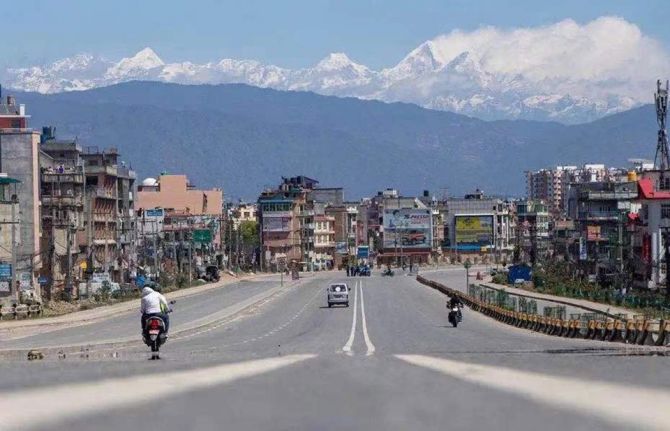
15 March 2021 15 March 2021Wang Tang (not his real name) had never been to Nepal before, but at the end of March 2020 it was one of the few countries that had not closed its borders with China. Since he was desperate to get away from Beijing after having had to stay at home for months after the coronavirus outbreak spread throughout China, he bought a ticket.
But days after he arrived, while he was staying in Pokhara, the fourth stop on his trip, the local government announced that the city would be shut down. He heard that the lockdown would not last longer than a month.
As someone who is living with HIV, he had brought along enough HIV treatment to last for a month. However, he soon learned that the re-opening of the city was to be postponed, which meant that he was at risk of running out of the medicine he needed to take regularly in order to suppress his HIV viral load and stay healthy.
Mr Wang swallowed hard while counting the remaining tablets. He had no idea how to get more.
As the lockdown dragged on, it seemed that no end was in sight. Mr Wang started to take his medicine every other day so that his supply would last a little bit longer.
He contacted his friends back at home, hoping that they could send medicine to Nepal, but they couldn’t. The country was under lockdown—nothing could be imported.
Then, Mr Wang contacted his friend Mu-Mu, the head of Beijing Red Pomegranate, a nongovernmental organization providing volunteer services for people living with HIV. It was with Mu-Mu’s help that Mr Wang learned how to obtain HIV treatment after he was diagnosed as living with HIV. Having known each other for many years, Mu-Mu had the trust of his friend. Mu-Mu contacted the UNAIDS Country Office for China to see if it was possible to deliver medicines to Mr Wang. A UNAIDS staff member quickly got in touch with the UNAIDS Country Office for Nepal.
Everything happened so quickly that Mr Wang was shocked when he received a message from Priti Acharya, who works for AHF Nepal and had been contacted by the UNAIDS Nepal office, saying that she would bring the medicine to him.
The next day, Ms Acharya rode her motorbike for 15 km on a dusty road before reaching the place where she would meet Mr Wang. When he came down from the mountains to meet her, Ms Acharya, drenched in sweat, was waiting under the midday sun.
“I was so happy and thankful for her hard work. She gave me a sunny Nepalese smile in return, as well as detailed instructions on the medicine’s dosage,” said Mr Wang.
They took a photograph together, then Mr Wang watched Ms Acharya as she left on her motorbike. Her image, disappearing in the distance, is carved into his memory. To attend the five-minute meeting, Ms Acharya had to ride a round trip of more than 30 km.
“For half a month or so, I had been suffering from pain and anxiety almost every day due to the lack of medication and the loneliness of being in a foreign country on my own. I could not believe that I got the HIV medicine in such a short time,” said Mr Wang. After the trip, he wrote to thank Ms Acharya, explaining how important the medicine he now had in his hand was: “it’s life-saving.”
At the end of his stay in Nepal, Mr Wang wanted to do something for UNAIDS. As he is an experienced photographer, he volunteered to carry out a photo shoot for UNAIDS’ Nepal office.
The subject he chose was former soccer player Gopal Shrestha, the face of an HIV charity in Nepal and the first person living with HIV to reach the summit of Mount Everest. After his HIV diagnosis in 1994, Mr Shrestha launched the Step-Up Campaign and spent many years climbing mountains worldwide, hoping to give strength and hope to people living with HIV.
In 2019, Mr Shrestha reached the peak of the world’s highest mountain, Mount Everest, recording a historic breakthrough for people living with HIV. “If 28 000 people have already climbed Mount Everest, why can’t I?" he said. “By climbing the highest mountain in the world, I want to prove that we are no different from anyone else and that we can all make a difference.”
“The moment I saw him, I could tell he was a sophisticated man,” said Mr Wang. Without instructions, Mr Shrestha posed naturally in front of the camera. He displayed confidence and charm. His eyes, content and clear, reflected nature’s beauty. “The eyes surely are the window to the soul,” Mr Wang said.
Mr Wang is looking forward to his next trip to Nepal. After the pandemic, Pokhara’s lakeside will be flooded with tourists, and he looks forward to seeing the mountain town bustling with people like it used to.
Our work
Documents
Prevailing against pandemics by putting people at the centre — World AIDS Day report 2020
26 November 2020
Five years after a global commitment to Fast-Track the HIV response and end AIDS by 2030, the world is off track. A promise to build on the momentum created in the first decade of the twenty-first century by front-loading investment and accelerating HIV service provision has been fulfilled by too few countries. Read press release This document is also available in Arabic


Feature Story
Rich nations vaccinating one person every second while majority of the poorest nations are yet to give a single dose
10 March 2021
10 March 2021 10 March 2021US, UK and EU blocking proposals at WTO to help poorer countries get vaccines more quickly
One year on from the declaration of the COVID-19 pandemic, the People’s Vaccine Alliance is warning that developing countries are facing critical shortages of oxygen and medical supplies to cope with COVID-19 cases yet the majority have been unable to administer a single dose of a COVID-19 vaccine. In contrast rich nations have vaccinated their citizens at a rate of one person per second over the last month.
Many of these rich nations, including the US, UK and EU, are blocking a proposal by over 100 developing countries to be discussed at the World Trade Organisation (WTO) today, which would override the monopolies held by pharmaceutical companies and allow an urgently needed scale up in the production of safe and effective COVID-19 vaccines to ensure poorer countries get access to the doses they desperately need.
While more poor countries will see the arrival of doses in the coming days from the World Health Organisation’s COVAX facility, the amounts available mean only three per cent of people in those countries can hope to be vaccinated by mid-year, and only one fifth at best by the end of 2021.
Almost one million people worldwide have signed a call by the People’s Vaccine Alliance – a group of campaigning organisations including Oxfam, Frontline AIDS, UNAIDS, Global Justice Now and the Yunus Centre – for rich nations to stop protecting big pharma monopolies and profits over people’s lives. On 11 March protests will take place outside pharmaceutical headquarters as part of a global day of action by activists across the world.
Recent public opinion polls carried out by YouGov for the Alliance in the US, France, Germany and the UK found that on average, across these countries, more than two-thirds (69 per cent) of people thought that governments should ensure vaccine science and know-how is shared with qualified manufacturers around the world rather than remaining the exclusive property of a handful of pharmaceutical giants and that vaccine developers should be adequately compensated for this.
Oxfam International’s Executive Director, Gabriela Bucher, said: “Around the world, two and a half million lives have already been lost due to this brutal disease and many countries are battling without adequate medical care and no vaccines. By allowing a small group of pharmaceutical companies to decide who lives and who dies, rich nations are prolonging this unprecedented global health emergency and putting countless more lives on the line. At this crucial time, developing countries need support – not opposition.”
The Alliance warned that in South Africa, Malawi and other African nations history is in danger of repeating itself. Millions of people died in the early 2000’s because pharmaceutical monopolies had priced successful treatments for HIV/AIDS out of reach at up to $10,000 a year.
Lois Chingandu, activist and Director of Evidence and Influence at Frontline AIDS, said: “Here in Zimbabwe, I have lost many dear friends, struggling to breathe in their last moments. It is a cruel irony that activists who fought tirelessly for free medicines for HIV/AIDS are now being killed by COVID-19 because, yet again, pharma profits are being put ahead of people’s lives.”
Pharma monopolies were eventually overruled allowing the mass production of cheap effective treatment for those living with HIV/AIDS, meaning millions of people are alive today who would otherwise have perished.
On 10-11 March, more than 100 developing countries, led by South Africa and India will again make the case at the WTO for a waiver of Trade-Related Aspects of Intellectual Property (TRIPS), which would remove legal barriers for more countries and manufacturers to produce the vaccines, protect their people and join the economic recovery ahead.
Nobel Laureate Professor Muhammad Yunus, one of the leaders of the People’s Vaccine Alliance said: “For the rich world, this proposed act of human solidarity to ensure that medicines and vaccines get to the whole human family simultaneously is in their own self-interest, not just an act of charity.
“We should act now. There is no going back. It is totally unfair that rich countries, who have enough vaccines to protect their citizens, are blocking the TRIPS waiver, which could help poorer countries get the vaccines they need.”
All the leading vaccine developers have benefited from billions of dollars in public subsidies, yet pharmaceutical corporations have been handed the monopoly rights to produce and profit from them.
At the same time qualified vaccine producers all over the world stand ready to produce more vaccines if they were allowed access to the technology and know-how now being held under lock and key by these companies. New capacity could be brought on stream within months. Suhaib Siddiqi, former director of chemistry at Moderna, producer of one of the first approved vaccines, said that with the blueprint and technical advice, a modern factory should be able to produce vaccines in at most three to four months.
France has called for the expansion of production in developing countries, and the US has moved to achieve the same domestically. But so far both countries continue to defend the monopolies of pharma corporations.
To control the virus, enough doses of vaccines need to be produced in different geographies, priced affordably, allocated globally and widely deployed for free in local communities. Thus far, the world is failing on all four fronts.
Winnie Byanyima, Executive Director UNAIDS, said: “Amid so much personal selflessness, sacrifice and heroism, the People’s Vaccine Alliance denounces the hypocrisy, emptiness of human solidarity and myopic self-interest that defeats efforts to control the virus in countries. Only a truly global mobilization of vaccine production to rapidly scale-up the total number of low-cost doses available will get the job done.”
Nick Dearden, Director of Global Justice Now, said: “One year into the global pandemic, it’s an outrage that vaccine factories are lying idle, unable to produce COVID-19 vaccines because rich countries are prioritising the patents of pharmaceutical companies ahead of the lives of people across the world. A global suspension of patents is needed to speed up the production of these vaccines everywhere.”
Notes to editors:
- Drawing on data from OurWorldInData, Bloomberg, John Hopkins University and additional searches, of the 79 low and lower-middle income countries, as classified by the World Bank, the majority (at least 47 countries) are yet to vaccinate anyone. This figure is accurate as of 4 March and factors in reported planned deliveries of COVAX vaccines in the coming days even if vaccines are yet to be administered. We recognise that more unreported COVAX shipments may arrive in the interim.
- Since the start of 2021 high income countries have on average vaccinated citizens at a rate of one dose per second. This is based on the average daily COVID-19 vaccination doses administered between 1 January and 2 March 2021 and was drawn from OurWorldInData for countries classified as ‘High Income’ by the World Bank. An hourly rate was calculated by assuming countries are vaccinating 8 hours per day which was then divided into minutes and seconds. The average of these per second rates for these 68 high income countries was then calculated at 1.1 doses per second or 66 per minute. The average figure includes six High Income countries that have not yet begun vaccinating citizens.
- The YouGov poll results for the individual countries were: US – 69 per cent, France - 63 per cent, Germany 70 per cent and the UK 74 per cent, which gives a combined average across the countries of 69 per cent. All figures, unless otherwise stated, are from YouGov Plc. Total sample size was 1,351 adults in the US, 1788 adults in the UK, 1010 adults in France and 2039 adults in Germany. Fieldwork was undertaken between 23 – 26 February 2021. The survey was carried out online. The figures have been weighted and are representative of all adults (aged 18+) in each individual country of the US, UK, France and Germany.
- Last week, The Associated Press found factories on three continents whose owners said they could begin producing hundreds of millions of doses of COVID-19 vaccines on short notice, if only they had the blueprints and technical know how to do so.
- Countries like South Sudan, Yemen and Malawi have seen dramatic surges in cases in recent months. Malawi saw a 9500 per cent increase in cases as the South African mutation spread through the country and two of their cabinet ministers died in one day.
Contact
Matt Graingertel. +44-7730680837
matt.grainger@oxfam.org
Sarah Dransfield
tel. +44 (0)7884 114825
sarah.dransfield@Oxfam.org
Our work
Related


Feature Story
Tackling gender inequalities and gender-based violence during the COVID-19 pandemic in Asia and the Pacific
08 March 2021
08 March 2021 08 March 2021“It was hard for us before COVID-19, but it has become even harder now,” said Ayu Oktariani, the National Coordinator of the Indonesia Positive Network of Women Living with HIV (IPPI). For more than 10 years, she has been working with women and adolescents living with HIV who have been subjected to domestic violence in Indonesia, providing them with psychosocial support and counselling. Since the first COVID-19 outbreak, she has seen increased requests for help, as violence has escalated alarmingly.
Even before the COVID-19 pandemic, domestic violence was already one of the most significant human rights violations, but the pandemic has made a challenging situation even worse. Confinement is increasing the stress caused by security, health and money worries and is increasing the isolation of women with violent partners, separating them from the people and resources that can best help them.
According to a survey conducted by the International Community of Women Living with HIV in Asia and the Pacific (ICWAP) with support from the UNAIDS Regional Support Team for Asia and the Pacific, in June 2020 almost 30% of the respondents experienced some form of gender-based violence, including stigma and discrimination. In addition, more than 80% reported a lack of access to sexual and reproductive health services, including contraception.
In Indonesia, a report released by the National Commission on Violence against Women shows that the number of reported cases of violence against women living with HIV has significantly increased during the pandemic. “A few months ago, I was contacted by a woman living in a rural area, who was forced by her husband to have regular unprotected sex. She was unable to negotiate the use of condoms because of fear of violence,” said Ms Oktariani.
With other organizations in Indonesia, IPPI is developing a referral system that will guide women living with HIV who have been subjected to violence to women-led organization for legal advice and support. IPPI is also part of a national coalition that connects women and girls, including women living with HIV, to emergency services, including the police and justice and social services.
In Nepal, women living with HIV are faced with similar ordeals as a result of the COVID-19 pandemic. Sara Thapa Magar, the President of the National Federation of Women Living with HIV and AIDS (NFWLHA), Nepal, reflects on Lily’s (not her real name) story, a woman living with HIV who was beaten by her husband after she went to the local hospital to get refills of her antiretroviral therapy. The current circumstances, including limitations on access to helplines and disrupted public services, have made reporting of abuse and violence even harder.
NFWLHA has played a critical role in addressing these challenges by offering legal support to women like Lily subjected to domestic violence and providing relief packages to women and children living with HIV. “Despite these efforts, we are struggling to cope with the knock-on effects of the pandemic, and one of the main reasons is the lack of funds,” said Ms Magar. “Women-led organizations need to be continuously supported in our frontline role.”
Kousalya Periasamy, the founder of the Positive Women Network (PWN+), explains the multiple impacts of COVID-19 on the life of women living with HIV in India. “Many women and girls were afraid of going to the hospital to get their antiretroviral therapy refill and access general health services out of fear of COVID-19,” said Ms Periasamy. “Women living with HIV who had COVID-19 were not able to provide for and look after children if they had to be admitted into the hospital.” Given the need to communicate with local network partners and members, PWN+ established a WhatsApp group to ensure that women living with HIV had access to reliable information on HIV and COVID-19. PWN+ also mobilized support from different local organizations to donate food and supplies and handed out pamphlets containing HIV and COVID-19 information.
Sarah Feagan, a Board Member of ICWAP, works for a local agency in Australia, Living Positive Victoria (LPV). During the lockdown in Melbourne, “I worked to ensure women living with HIV remained connected and supported during COVID-19. Since I could not meet anyone in person, I kept in touch on the phone, linking them together via online workshops and other women living in similar areas to meet up without breaking the 5 km rule,” she said. She was able to offer financial support, food parcels and legal and emotional support thanks to LPV and other HIV organizations.
“On International Women’s Day, we commend all our sisters across Asia and the Pacific, who, like Ayu, Sara Thapa, Sarah and Kousalya, are establishing supportive mechanisms for women and girls living with HIV, even in the face of adversities,” said Sita Shahi, ICWAP Regional Coordinator.
During the COVID-19 pandemic, the UNAIDS Regional Support Team for Asia and the Pacific has joined hands with ICWAP to raise awareness about the needs and challenges of women living with HIV and to support the implementation of small local relief projects in Nepal, Malaysia and India. “COVID-19 is already testing us in ways most of us have never previously experienced. We must emerge renewed, with women living with HIV as a powerful force at the centre of the recovery,” said Eamonn Murphy, Director of the UNAIDS Regional Support Team for Asia and the Pacific.
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa


Feature Story
From HIV survivor to COVID-19 responder
03 March 2021
03 March 2021 03 March 2021Ingrid Bretón learned that she was living with HIV when she was 19 years old. It was 1994 and HIV treatment was not yet available in the Dominican Republic.
“I lasted almost five years alive, but dead inside,” she remembers. “I went through every denial process that a newly diagnosed person goes through. Health centres did not want to assist me. I lived every kind of stigma and discrimination.”
In her town, La Romana, she was known as “the AIDS girl”. It was impossible to find work.
HIV treatment helped changed the trajectory of her life. With the guidance of her doctor, José Román, she became the first woman living with HIV in La Romana known to have given birth to an HIV-free baby. As she continued treatment it occurred to her that she was perfectly healthy and could live a more meaningful life.
“I thought to myself, “I am not getting sick, my hair is not falling off, I do not have sores, I do not have AIDS. I want to do things,”” Ms Bretón remembers.
In 2002 she formed the Paloma Group Foundation (La Fundación Grupo Paloma), which provides psychosocial support, legal assistance and job opportunities for people living with and affected by HIV in the eastern region of the country. The organization also plays a key advocacy role, bringing visibility to issues such as treatment adherence, prevention and stigma and discrimination.
One of the foundation’s innovations is an agriculture project that employs people living with HIV.
“It’s a beautiful process,” Ms Bretón says while walking through the sunny, red earth fields, past tomatoes, papayas and bananas. “The idea is that people living with HIV are able to move forward, working and providing for their families.”
The families with whom the Paloma Group Foundation works have been directly affected by the COVID-19 pandemic. The work of the foundation has been critical during this time. Its volunteers do home deliveries of food, medicine and clothing. The foundation is a source of connection and emotional support at a time when communities living with HIV are more isolated than ever due to social distancing measures.
The first Rapid Survey on the Needs of People Living with HIV in the Dominican Republic in the context of COVID-19 found that while 92% of respondents received their antiretroviral therapy, roughly one in six had less than one month’s supply left. Thanks to the advocacy of the UNAIDS Country Office for the Dominican Republic, protocols have now been amended so that people living with HIV and accessing treatment through the public health system can receive a three- to six-month supply of their medicine at one time.
The country office has urged the government to strengthen comprehensive care programmes, including through alliances with civil society. For example, the Paloma Group Foundation provided assistance to people living with HIV at the Francisco Gonzalvo Provincial Hospital during a five-month period in 2020 when medical personnel were not available at the La Romana facility.
The UNAIDS Country Office for the Dominican Republic has also called for particular attention to be given to the social protection and food security needs of people living with HIV who are in economically fragile situations. The office responded quickly to the fallout of COVID-19, offering support to the Paloma Group Foundation and other community organizations contributing to the national HIV response. UNAIDS’ comprehensive response included the provision of personal protective equipment and information specifically for the community of people living with HIV. The second stage of their response included mobilization of nutrition support.
“This was of great value to families given the economic crisis caused by COVID-19,” Ms Bretón says.
“Civil society plays the leading role of bringing awareness to communities and advocating on their behalf,” says the UNAIDS Country Director for the Dominican Republic, Bethania Betances. “As we respond to two pandemics—HIV and COVID-19—is it vital that they are at the decision-making table to help shape an effective, humane response.”
Watch: The extraordinary story of a woman living with HIV in the Dominican Republic
Region/country


Feature Story
COVID-19 spurs on multimonth dispensing of HIV treatment in Cambodia
25 February 2021
25 February 2021 25 February 2021When the COVID-19 pandemic broke out in Phnom Penh, Em Ra, pictured above, was worried.
She lives with HIV and she only had supplies of medicine to last a month.
“First, I was afraid that the medicine could not be shipped to Cambodia, the second is that when we don’t have medicine for a few months we have to come to the clinic often,” she said. “This increases my expenses but also raises my chances of getting COVID-19.”
During a recent visit to the National Center for HIV/AIDS, Dermatology and STDs (NCHADS) clinic, her doctor, Prak Narom, informed her that she would qualify for multimonth dispensing of HIV treatment. “Because of COVID-19, a patient in good health who takes their treatment daily can be prescribed HIV medicine for more than three months, and for some patients we can give them up to six months,” he explained.
Ms Ra is one of thousands in Cambodia who can now pick up a stock of medicine in one visit. There are an estimated 73 000 people living with HIV in Cambodia and now nearly 50% of people on treatment have access to multimonth dispensing of HIV treatment. Before the pandemic, that number stood at 34%.
The multimonth dispensing of HIV treatment programme in Cambodia began in 2019, long before the COVID-19 pandemic, but it has proven to be a godsend.
“When we started multimonth dispensing, there were some challenges because we had a shortage of drugs, but today we have overcome that so we can give medicine to people for up to six months,” said Ly Penh Sun, Director of NCHADS, pictured above.
The UNAIDS Country Director for Cambodia, Vladanka Andreeva, had feared the worse when COVID-19 shut down the country. “The biggest and oldest HIV treatment site in the capital was repurposed to serve as a COVID-19 centre and our outreach activities had to cease with public venues closed to the public.”
But UNAIDS, with the national AIDS programme and communities, worked together and helped with moving people to another treatment site, while providing face coverings and hand sanitizer to people living with HIV. UNAIDS also advocated that people living with HIV be integrated in the emergency cash transfer programme. As a result, more than 2500 households benefitted.
And more importantly, UNAIDS and partners pushed to introduce the home delivery of treatment and the rollout of multimonth dispensing of HIV medicine at the national level.
“We have used COVID-19 as an accelerator to further scale up and promote the multimonth dispensing of medicine,” Ms Andreeva said, pictured above.
It has been so successful that Mr Narom can’t believe it.
“In the past we used to see 30 patients in the morning, but now with multimonth dispensing we can reduce that by half or more than half,” he said. “I can now spend more time with my patients and carry out more in-depth check-ups.”
When a person is unable to take antiretroviral therapy regularly, their viral load increases, impacting the person’s health, which can ultimately lead to death. Even relatively short-term interruptions to HIV treatment can have a significant negative impact on a person’s health and potential to transmit HIV.
UNAIDS is advocating that all countries, ministries of health and national AIDS programmes grant access to three months or more of antiretroviral therapy for all people living with HIV, including refugees and migrants.
As for Ms Ra, she has joined a Telegram group started by the clinic for people living with HIV in case they have questions about their health or their medicine.
Watch: COVID-19 spurs on multimonth dispensing of HIV treatment in Cambodia
Photo credit: UNAIDS/S.Dara
Our work
Watch: COVID-19 spurs on multimonth dispensing of HIV treatment in Cambodia
Region/country


Feature Story
Making a mark on the COVID-19 pandemic: joint efforts to meet the needs of young key populations in Asia and the Pacific
10 February 2021
10 February 2021 10 February 2021Ralph Ivan Samson, the President of Y-PEER Pilipinas, and his team of young volunteers have been working tirelessly throughout the COVID-19 pandemic to supply antiretroviral therapy to young people struggling to get refills. “How could I sleep at night knowing that community members were depressed and anxious about their refills. I had young people texting me they were down to their last couple of pills,” said Mr Samson, remembering the initial COVID-19 outbreak in the Philippines in March 2020. It was at this moment that he knew he had to do something.
Throughout the region, civil society organizations like Y-PEER Pilipinas began looking into ways of overcoming the barriers and challenges that prevent young people from accessing HIV services due to COVID-19 restrictions. For example, Y-PEER gained support from local governments with special travel passes to enable the delivery of antiretroviral therapy from the hospital straight to the doorsteps of young people living with HIV.
Y-PEER Pilipinas was one of several beneficiaries of the COVID-19 Emergency Relief Fund, a regional small-grants programme established by Youth LEAD to support initiatives led by young people across Asia and the Pacific during the COVID-19 pandemic. The COVID-19 relief fund supported 12 organizations led by young people in nine countries with various projects, including the delivery of antiretroviral therapy, hygiene products, opioid substitution therapy, emergency supplies and food, cash transfer programmes for businesses run by transgender people and housing for key populations.
Youth LEAD’s efforts to mobilize resources during the early days of the pandemic are a testament to young people rising up to the occasion and working in coordination with regional partners of the HIV response in Asia and the Pacific. In their efforts to raise funds, Youth LEAD relied on the findings of a regional assessment on the needs of young key populations and young people living with HIV during the COVID-19 pandemic conducted by the Inter-Agency Task Team on Young Key Populations Asia Pacific (IATT on YKP), a regional coordinating platform comprised of United Nations agencies and young key populations regional networks. The results of this assessment helped to inform the IATT on YKP and its regional and national partners on ways to support organizations led by young key populations during the COVID-19 response. The evidence gathered through the survey was used to inform preparedness response plans and local strategies on providing timely information on COVID-19 prevention, supporting the delivery of antiretroviral therapy and tackling stigma and discrimination.
With the support received from Youth LEAD, Mr Samson and his team of volunteers provided condoms and lubricant and emergency supplies to young key populations and young people living with HIV across several provinces in the Philippines. The programme is known online as #GetCondomsPH, and a similar initiative led by young people from the COVID-19 Emergency Relief Fund supported the delivery of antiretroviral therapy to people’s doorsteps in Goa, India.
Aadi Baig, Programme Manager, and his team at Wasaib Sanwaro, an organization that works with gay men and other men who have sex with men and male sex workers in Pakistan, have also benefited from the COVID-19 Emergency Relief Fund. Mr Baig revealed a troubling picture of how the COVID-19 pandemic has made things worse for key populations. “The pandemic has created a greater divide among people, socially and economically, and has uncovered the lack of social security and protection programmes for key populations.”
With the support received, Wasaib Sanwaro donated food and supplies to key populations and provided basic HIV and COVID-19 training. Although there are limited funding schemes for organizations of young people across the region to access grants, regional networks of young people, such as Youth LEAD, Y-PEER and YVC, and the coordinated response by the IATT on YKP, which in 2020 was co-chaired by the UNAIDS Regional Support Team for Asia and the Pacific, the APCASO nongovernmental organization and the United Nations Development Programme, have stepped in to provide support.
As part of the work of the IATT on YKPs, a website that pools together COVID-19 resources for young key populations and showcases how young people have stepped up to respond to the COVID-19 pandemic was developed. The website also focuses on resources on the mental health of young key populations and the well-being of adolescents and young people at higher risk of HIV.
The most crucial aspect of all these activities was visibility, the visibility of young people, to ensure that young key populations and young people living with HIV had a voice during the pandemic. To keep the issues and needs of young key populations on the top of the advocacy agenda in the region, the IATT on YKP, with support from the UNAIDS Regional Support Team for Asia and the Pacific and Youth LEAD, held the first Spill the T with YKPs webinar—an online panel with young people from across the region that offered a platform for young people to talk about their initiatives and their roles in the COVID-19 response. The series continued through the collaboration of the IATT on YKP with partners and explored issues of young people’s leadership, mental health and sexual and reproductive health and rights.
Our work
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa


Feature Story
How was a COVID-19 vaccine found so quickly?
09 February 2021
09 February 2021 09 February 2021As COVID-19 vaccination begins around the world, UNAIDS spoke to Peter Godfrey-Faussett, UNAIDS Senior Science Adviser and Professor of International Health and Infectious Diseases at the London School of Hygiene and Tropical Medicine, about what is holding up an HIV vaccine.
Many people are asking, “How was a COVID-19 vaccine found so quickly?”
The SARS-CoV-2 virus, which is the virus that causes COVID-19, jumped from animals into humans in 2019. Whereas for HIV, that jump occurred 100 years ago in around the 1920s, and it became a problem in the 1980s when it started spreading among humans to a much greater extent.
The reason we’ve seen such a push on the COVID-19 vaccine is because of the urgency. In 2020, COVID-19 has infected almost 100 million people on the planet. COVID-19 has already killed 2 million people in 2020.
So, this urgency comes about, despite the fact that we’ve seen dramatic changes in everybody’s life, with changes to travel and social distancing and masks and hand washing and sanitizer, and yet we've still seen a rapid rise in infections. This produces a huge urgency to make a vaccine. And, of course, it has a massive economic impact.
HIV and SARS-CoV-2 are quite different, right?
There are fundamental differences between SARS-CoV-2 and HIV. Although they are both viruses, SARS-CoV-2 is a very simple infection. The disease can be complicated, and sometimes mysterious, but almost everyone infected with SARS-CoV-2 develops antibodies to the spike protein and this neutralizes the virus and leads to recovery with a clearance of the virus.
In contrast, almost everybody infected by HIV develops antibodies and we use those antibodies in regular HIV tests. But, unfortunately, very few clear the infection and those antibodies are not sufficient to neutralize the HIV. The HIV envelope, which is more or less like a spike, is a complex structure on the surface of the virus. It’s coated with sugars and the active site is deep inside, so it’s hard to engage with it.
Over time, as people are infected with HIV some people do develop antibodies able to neutralize HIV, but that can take many years, and furthermore HIV is a retrovirus—that’s why we talk about antiretrovirals. A retrovirus is a virus that copies its genetic code and integrates it into the human genetic code. And as it copies, it copies its genetic code, but it doesn’t do it accurately, it makes many mistakes. What that means is that the envelope protein and the HIV itself is constantly changing, shifting its shape, making it difficult for antibodies to protect against it, so even the neutralizing antibodies from one individual often fail to neutralize the virus from a different individual.
We have now found some so-called broadly neutralizing antibodies, as in antibodies that neutralize many different strains of HIV. And those are the antibodies that people are studying at the moment and trying to see whether or not they protect people from catching different strains of HIV. They could be an important part of the process for developing a vaccine against HIV if we could get broader neutralizing antibodies to be generated before the HIV infection occurred.
Finally, we have to remember that, unlike COVID-19, or maybe partly unlike COVID-19, HIV depends a lot on T-cells—the other half of the human defence system. The human immune system has antibodies, but it also has so-called cellular immunity, which is led by T-cells, and that’s much harder to study and much more varied and it also makes HIV difficult and different from COVID-19 when it comes to developing a vaccine.
How much money is being invested in HIV vaccines?
Each year for the past decade we’ve invested around US$ 1 billion in research and development to try to produce an HIV vaccine. Is that a lot or is it not enough? It’s about 5% of the global HIV response budget. There has been some limited success. Back in 2009 there was great excitement when a vaccine candidate in Thailand did produce some protection against HIV infection, but not enough for it to be taken into widescale production.
And then over the next decade, subsequent trials have taught us a lot about the immunology, about the way human bodies and immune systems interact with HIV, but they haven’t led to a reduction in new HIV infections. Hope is currently resting on two large studies that are in the field at the moment, and there are many other candidates in the pipeline. So, I think there is hope, but we clearly won’t have a vaccine in the short term in the way that we have with COVID-19.
COVID-19 has taken the headlines—what about other infectious diseases?
In Africa, tuberculosis, malaria and HIV each kill more than five times as many people per year as COVID-19 has killed in Africa this year. These are huge problems and they've been going on for a long time. We have a vaccine against tuberculosis, the BCG vaccine, first used 100 years ago, starting in 1920, but unfortunately it doesn't really protect against the common adult forms of tuberculosis. Just recently, new vaccines have been discovered against both tuberculosis and malaria, but they don’t work particularly well. There are discussions about whether to scale them up because they only have a protective efficacy of 30% or less.
The good news is that a new malaria vaccine has just gone into big phase three trials in Africa, and in fact it’s produced by the same setup that has produced the AstraZeneca Oxford COVID-19 vaccine, so the hope is that the research that’s being done on COVID-19 vaccines may act as a shot in the arm for all the other important infectious disease killers that actually kill many, many more people in Africa and other resource-constrained parts of the world.
Watch: UNAIDS Science Adviser explains some differences between HIV and COVID-19
Watch: UNAIDS Science Adviser explains some differences between HIV and COVID-19
Our work
Related


Press Statement
UNAIDS calls for the release of five humanitarian workers detained in the Bolivarian Republic of Venezuela
29 January 2021 29 January 2021GENEVA, 29 January 2021—UNAIDS is deeply troubled and concerned about the detention by military police of the Venezuelan citizens and humanitarian workers Johán León Reyes, Yordy Bermúdez, Layners Gutiérrez Díaz, Alejandro Gómez Di Maggio and Luis Ferrebuz, who are members of the nongovernmental organization Azul Positivo. The five have been held since 12 January 2021.
“I call on the Venezuelan authorities to release from police custody the five humanitarians working for the nongovernmental organization Azul Positivo, and to return essential equipment seized at the time of their arrest,” said Winnie Byanyima, UNAIDS Executive Director. “A strong and empowered civil society plays a central role in providing much-needed services to the most vulnerable people and is critical to making progress against the HIV pandemic and other health threats in the Bolivarian Republic of Venezuela.”
Azul Positivo was established in 2004 to work on the prevention of HIV in the state of Zulia, Bolivarian Republic of Venezuela. UNAIDS has supported Azul Positivo’s work for many years and has witnessed the positive impact of their contributions to the community.
UNAIDS is strongly supportive of the full empowerment and engagement of civil society organizations in the AIDS response and in humanitarian work. It looks forward to continuing its partnership with community and civil society organizations in the Bolivarian Republic of Venezuela, as well as with government officials, in ensuring that all people affected by HIV have access to HIV prevention, treatment and social support services and that their human rights are protected.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Region/country




Feature Story
Hand sanitizer donated by Reckitt Benckiser to people living with HIV
25 January 2021
25 January 2021 25 January 2021Russian HIV community centres in Moscow, Voronezh, Kaluga, Kursk, Orel and Vladimir have received 35 000 bottles of Dettol hand sanitizer donated as part of an initiative by Reckitt Benckiser. The donation was made in the light of the increasing COVID-19 pandemic in the country and the increase in other viral diseases, and is a joint effort of the Reckitt Benckiser office in the Russian Federation and the UNAIDS Regional Support Team for Eastern Europe and Central Asia. The nongovernmental organizations Medical Volunteers, Volunteers to Help Orphans and Center Plus also partnered in the initiative, distributing the donations to the community centres.
“This is very timely support for people from key populations, those who are at risk and work on the front lines of the fight against both pandemics, HIV and COVID-19, as well as those who do not have an opportunity to take care of themselves on their own,” said Vladimir Mayanovsky, head of Center Plus.
A study conducted by the Central Research Institute of Epidemiology of Rospotrebnadzor (the Federal Service for Surveillance on Consumer Rights Protection and Human Wellbeing), in cooperation with the Treatment Preparedness Coalition with the support of UNAIDS, found that the number of people living with HIV with COVID-19 markers was four times higher than that of HIV-negative respondents. And people living with HIV were two times less likely than HIV-negative respondents to be tested for coronavirus and less often sought medical help, even if they had symptoms.
The study also found that the majority of respondents living with HIV were found to have a higher risk of contracting COVID-19, owing to the significant number of infections in their neighbourhood and their low level of use of personal protective equipment, and underestimated their personal risk of COVID-19 disease. Hand sanitizer can help to protect people from contracting the coronavirus.
“Reckitt Benckiser’s mission is to protect, heal and nurture, creating a cleaner and healthier world. In the countries where we operate, we strive to promote the idea of a responsible attitude to health and consider hygiene to be the basis of a healthy lifestyle. Keeping hands clean is one of the most important simple habits. For Reckitt Benckiser, this is more than a business, it is a contribution to a healthier and happier future,” said Igor Radakovich, the General Director of Reckitt Benckiser Healthcare in the Russian Federation, Ukraine and the Commonwealth of Independent States countries.
“UNAIDS welcomes and supports such initiatives from the private sector in the fight against the colliding epidemics. We are ready for further cooperation with Reckitt Benckiser in the field of health. We share Reckitt Benckiser’s vision given in its slogan for educational initiatives in the Russian Federation, “Your health is your responsibility”, not only in terms of COVID-19 prevention but also HIV prevention by the promotion of condom use,” said Alexander Goliusov, Director, a.i., of the UNAIDS Regional Support Group for Eastern Europe and Central Asia.