Feature Story
“We must do everything we can to keep the lights on for the HIV response” says UNAIDS Country Director for Ethiopia Tina Boonto
26 May 2025
26 May 2025 26 May 2025Ethiopia, with a population of 130 million, is Africa’s second most populous country. Despite steady economic growth approaching low-middle income status, the country faces a daunting number of challenges, from economic pressures and development needs to recurring natural disasters such as droughts and floods, as well as conflict and other man-made crises. These factors mean Ethiopia still relies heavily on external aid-particularly for food security and humanitarian assistance.
On top of these existing burdens, HIV remains a significant public health challenge. The country is home to an estimated 610 000 people living with HIV, with over half a million currently on life-saving antiretroviral treatment-most of which is funded by international donors. Recent cuts in US funding have put Ethiopia’s HIV response at risk, threatening to reverse years of progress and placing additional strain on an already fragile health system.
We sat down with Tina Boonto, UNAIDS Country Director for Ethiopia, to discuss the impact of the funding crisis, the government’s response, the resilience of communities, and what needs to happen next to protect Ethiopia’s HIV response.
Q: What is the current situation, and how has the recent US funding crisis impacted the HIV response?
Ethiopia has made significant progress in its HIV response in recent years and is on track to reach the UNAIDS 95-95-95 targets with 90% of people living with HIV in the country being aware of their HIV status; 94% of those diagnosed with HIV receiving antiretroviral (ARV) therapy; and 96% of people on ARV therapy achieving viral suppression. The US Government through PEPFAR and the Global Fund have been the primary funders for the HIV response, supporting treatment for over 530 000 of the estimated 600 000 people living with HIV in the country. However, the sudden cuts had a devastating impact. Critical services have stopped, people have lost their jobs, and many clinics have closed their doors. People living with HIV now face uncertainty about their access to medication, testing, and prevention services.
In Bahir Dar, for example, programmes for key population have stopped, outreach workers have lost their jobs, and peer support groups have been terminated. It’s heartbreaking to see the situation on the ground. Clients arrived at clinics to find them closed, and many were left without guidance or support.
Women are anxious about the availability of medication and prevention tools like condoms. Without these, the risk of HIV transmission increases, and the health of those already living with HIV deteriorates. Some cannot even afford basic necessities like food, let alone treatment.
Q: How are communities responding to the collapse of HIV services?
Despite the collapse, communities are showing incredible resilience and a fighting spirit. Peer educators, youth groups and mothers are stepping in where formal systems are failing. For example, in the Afar region, a case manager working with people living with HIV continued his outreach work despite funding cuts. He was able to get funding from the health bureau and shared “even if the money is not enough, I’m happy to continue to help reach people living with HIV, providing pregnant women information on how to prevent transmission to their babies”.
But while these community-led efforts are inspiring, they cannot replace the need for sustainable funding. Community members often live below adequate income levels, and they need support for basics like transport and food. UNAIDS is encouraging the government to consider a social contract with community organizations-similar to Ethiopia’s successful Health Extension Worker model-so that peer outreach workers can be formally supported and paid for their essential outreach work.
The reason why we are pushing for outreach workers to be supported is because stigma and discrimination remain significant barriers. Even after 40 years of the HIV epidemic, people living with HIV in Ethiopia still experience stigma, which deters them from seeking care at public facilities. Many fear being discriminated against or not receiving adequate services. This is why the role of community peer outreach is so vital. Without armies of community outreach workers, especially in high-burden areas, it’s impossible to have a successful HIV programme.
Q: What lessons can be drawn from this crisis for the future of HIV response in Ethiopia and beyond?
The crisis has exposed the fragility of systems built around a single funding stream. When the money stopped, so did services, trust, and hope. We must build resilience into the system from the start. Community-led organizations must be recognized as essential, and youth-led innovation must be scaled up. Emergency preparedness and integrated, people-centered solutions are crucial, especially as HIV intersects with conflict, displacement, and gender-based violence. HIV must remain central to humanitarian, development and recovery agendas-not as an afterthought, but as a foundation.
UNAIDS is also supporting by working on producing an investment case to prioritize key components of the HIV programme for government funding. There are ongoing discussions about new partnerships with the private sector and exploring alternative financing mechanisms. There is political will. The Ministry of Health is considering adopting the methodology of the HIV Sustainability Roadmap to develop a broader health sector sustainability strategy. UNAIDS is supporting these efforts by helping to produce a sustainability strategy and mobilizing resources alongside other donors
Q: What steps is the Ethiopian government taking to address the funding crisis?
The government recognizes this as a wake-up call and is actively considering solutions to find resources to cover priority health issues, including HIV, tuberculosis, and malaria. However, the scale of the challenge is enormous-external assistance for Ethiopia’s health, humanitarian and development needs amounts to around US$ 2.7 billion annually. The government is exploring options such as introducing a social tax, where all workers would contribute to health funding, but this is still under parliamentary discussion. While these efforts are encouraging, they are not yet sufficient to fill the gap left by international donors.
Q: How is UNAIDS supporting the government and the HIV response during this crisis?
UNAIDS is playing a critical role. In response to the funding crisis, we conducted immediate impact surveys to understand which programmes have stopped or are ongoing, and what the consequences are on the ground. This information feeds into the national plans and sustainability plan.
We are also producing an investment case to help the government prioritize key components of the HIV programme for domestic funding. Our costing data enables us to propose affordable models, like social contracting with community organizations.
We are reviving HIV prevention efforts, including using AI-powered digital platforms and chatbots to reach young people with real-time information. Ethiopia was also piloting long-acting injectable antiretroviral medicine to prevent HIV or ‘PrEP’ before the funding cuts stopped this progress.
Finally, we are working closely with the Ministry of Health, the Global Fund, and community organizations to mobilize resources and advocate for integrated, sustainable solutions.
Q: What is your message to the international community at this critical juncture?
We need global solidarity now more than ever. We are so close to ending AIDS as a public health threat by 2030. Over half a million people in Ethiopia are on antiretroviral treatment—we cannot let them down. The world has come too far, and too many have sacrificed too much to let progress slip away now. We must do everything possible to keep the lights on for the HIV response, both in Ethiopia and globally.
The resilience of Ethiopian communities is inspiring. People are refusing to give up, finding new ways to support each other and keep the response alive. With renewed commitment from the government, partners, and the international community, we can protect the progress made and continue moving towards ending AIDS as a public health threat.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads the global effort to end AIDS as a public health threat by 2030 as part of the Sustainable Development Goals.
Following the US funding cuts in January, UNAIDS is working closely with governments and partners in affected countries to ensure that all people living with or affected by HIV continue to access life-saving services. For the latest updates, please visit unaids.org
Related resources
Watch: Tina Boonto, Ethiopia Country Director: Communities are going out of their way but they need help
Watch: UNAIDS asking government to increase domestic funding for the HIV response in Ethiopia
Watch: "We cannot let people down," says Tina Boonto, Country Director in Ethiopia
Region/country


Feature Story
Global leaders convene to accelerate access to long-acting HIV prevention technologies amidst funding cuts
23 May 2025
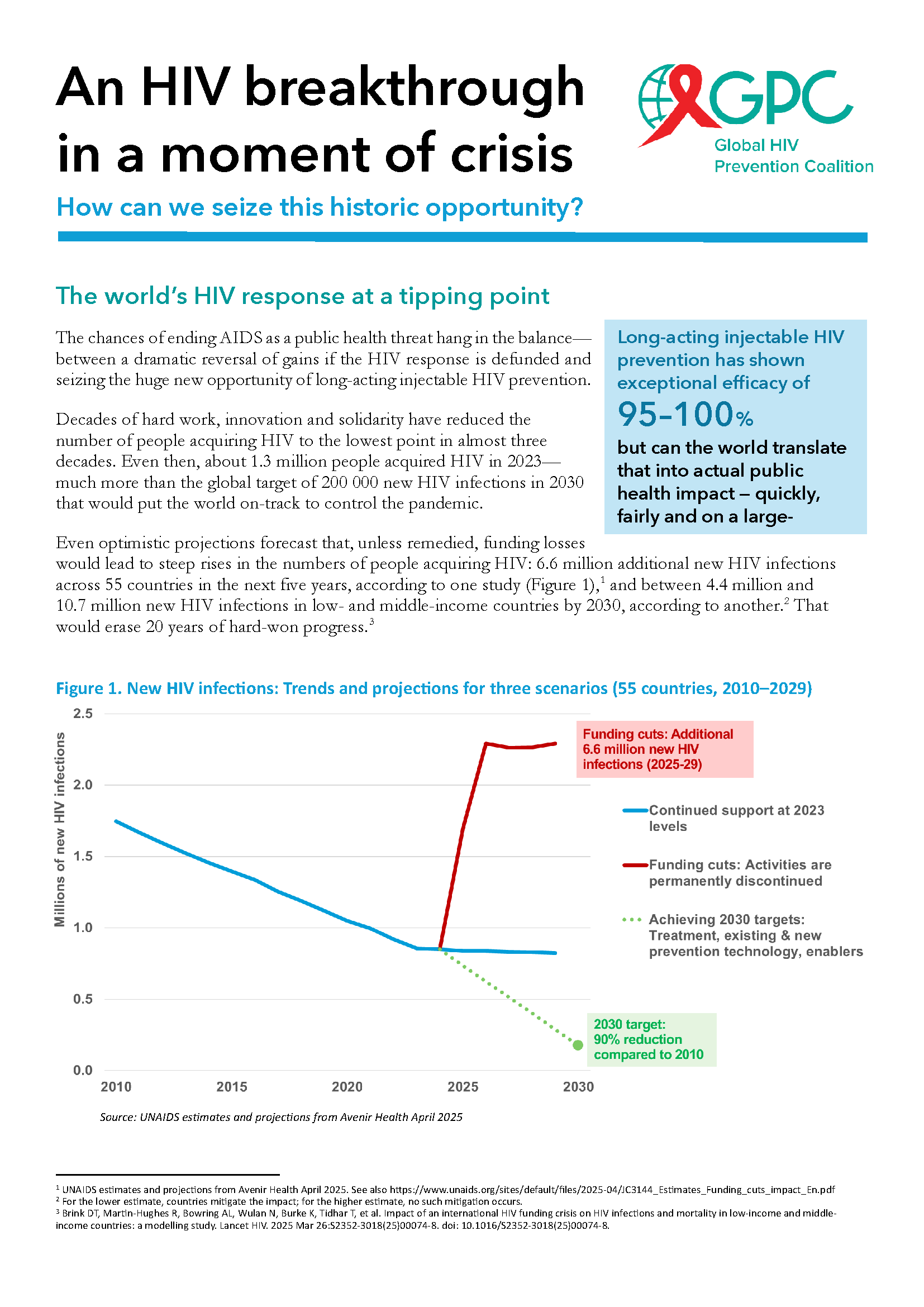
23 May 2025 23 May 2025The global response to HIV has reached a crucial juncture. Groundbreaking scientific advances, including the development of long-acting HIV prevention technologies like lenacapavir and cabotegravir, offer a transformative opportunity to curb the epidemic.
Long-acting injectables, which were hailed by Science magazine as one of the major breakthroughs in science in 2024, have shown exceptional efficacy, with lenacapavir demonstrating nearly 100% protection against HIV infection.
Despite these unprecedented advancements, the HIV response faces a dire threat from severe funding cuts. With more than 1.3 million new HIV infections annually, three times the target for 2025, financial constraints and a lack of sustained political will threaten to undo decades of progress. Global health experts warn that without urgent action to ensure continued investment, the ability to scale these life-saving technologies will be jeopardized, leaving millions at risk.
On the eve of the 78 World Health Assembly, global health leaders, government ministers, pharmaceutical companies, and civil society representatives gathered at UNAIDS headquarters in Geneva for the High-Level Multisectoral Leadership Dialogue on HIV Prevention. This High-Level dialogue, organized by the Global HIV Prevention Coalition and co-hosted by UNAIDS in collaboration with UNFPA, WHO, and UNDP, the Federal Republic of Brazil, and the Kingdom of the Netherlands, focused on accelerating access to long-acting HIV prevention technologies and advancing sustainable prevention systems.
Referring to the current funding crisis, Winnie Byanyima, Executive Director of UNAIDS, warned that “If we continue down this path, we could see an additional 6 million HIV infections and 4 million AIDS-related deaths by 2029. Put simply, we will lose control of the AIDS pandemic. But we have an opportunity today. We have new, long-acting HIV prevention tools that could fundamentally reshape the HIV response, putting us back on the right path.”
Global leaders presented successful national models from Africa, Asia and Latin America, illustrating how innovative prevention strategies are being implemented despite financial challenges. Mariangela Simao, representing Brazil, said “PrEP in Brazil is now a reality. We initially set a target of reaching 50,000 people with PrEP by 2025, but we’ve already surpassed that milestone, with 122,000 people currently using it. Our next goal is to reach 300,000 users by next year. Data shows that HIV incidence is declining in cities with more than 100,000 inhabitants where PrEP coverage is higher.”
Global HIV Prevention Coalition co-chair and CEO of AVAC, Mitchell Warren called for choice in HIV prevention.
“Condoms work well for some people and situations. Oral PrEP is safe and effective for those who can adhere to daily pill taking. The monthly dapivirine vaginal ring is a preferred option for some women, as is voluntary medical male circumcision for many men, while harm reduction is highly effective for people who inject drugs. Now, long-acting injectables offer an additional option for the many people who struggle to protect themselves from HIV and want more convenient and discreet prevention options.”
Key panel discussions focused on the cost of inaction, the significance of equity in access, and the role of long-acting prevention in the future HIV prevention toolkit.
The event underscored the urgent need for a multisectoral approach to overcoming structural barriers to prevention, including regulatory, financial, and societal challenges. The discussions highlighted that global solidarity and sustained political will are essential to closing the prevention gap and achieving the UNAIDS 2030 targets of fewer than 200 000 new HIV infections annually.
Ambassador Paul Bekkers, Permanent Representative of the Netherlands to the UN, closed the dialogue with a powerful call to action: “Not acting now means leaving a larger HIV epidemic to the next generation. Or we can put the world on course to achieve HIV epidemic control and eventually the end of AIDS as a threat to public health. As members of the Global HIV Prevention Coalition, we can achieve this together.”
As part of this pivotal moment, UNAIDS and the Global HIV Prevention Coalition launched a new brochure titled An HIV breakthrough in a moment of crisis: How can we seize this historic opportunity?