


Feature Story
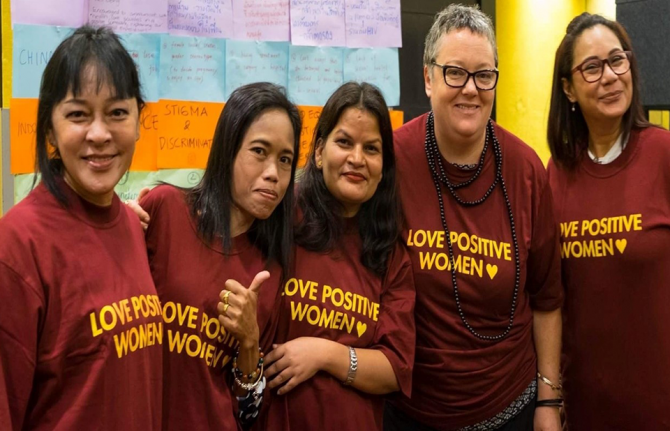
Asia Pacific women living with HIV speak out about rights violations
08 March 2023
08 March 2023 08 March 2023Nirmala Singh (not her real name) found out she was HIV positive after being tested during pregnancy. It was a surprise diagnosis, but she immediately knew how she had been infected. Before getting married she was raped. Nurses informed Nirmala’s husband of her positive result without her consent. She was immediately kicked out the home.
Sita Shahi, Regional Coordinator of the International Community of Women Living with HIV in Asia and the Pacific (ICWAP), has responded to this and many similar cases in her native Nepal.
“There is very little understanding of the rights of women living with HIV and how their experience is impacted by abuse,” Ms Shahi said. “Women are blamed for transmitting HIV because they are usually first in the family to be diagnosed. That is the starting point for them to experience human rights violations like intimate partner violence in the home and gender-based violence in the wider society.”
At a UNAIDS-supported ICWAP workshop organized in 2022 with participants from countries across the region, women living with HIV shared their personal stories.
One participant who was diagnosed during pregnancy was refused care by staff during childbirth. She delivered her baby on the floor of her ward, alone.
Some who have survived domestic violence said they were rejected by shelters run by government and non-governmental organisations based on their HIV status.
And there was consensus that in all countries domestic violence is common, but rarely reported.
The concerns of women living with HIV in the Asia Pacific region have remained relatively hidden and ignored. Rates of new infections and AIDS-related deaths among men in the region are more than double those of women. But for the estimated 2.2 million women living with HIV in Asia and the Pacific, smaller numbers do not mean smaller problems.
“Women in Asia and the Pacific continue to face discriminatory policies, social and cultural barriers, inequalities in healthcare access and threats to their security that violate their rights,” said UNAIDS’ Regional Adviser for Community-Led Responses, Michela Polesana.
“When women are free of any kind of stigma and discrimination, gender-based violence or breach of confidentiality by healthcare providers there is no accusing epidemic,” Ms Shahi reflected. “If a woman is free of violence at the policy level, society level and family level she can be mentally strong and her health could be as well as other people’s. Then there is no problem taking care of herself and her family while contributing to the economy.”
As a regional network, ICWAP is working to increase the capacity of organisations for and by women living with HIV so they can advocate around these issues at national level. A key priority is giving stakeholders including healthcare providers the information they need to help uphold the rights of women living with HIV.
One critical element of this strategy has been equipping its membership to advocate effectively using digital tools and spaces. UNAIDS supported social media advocacy training for ICWAP’s Young Advocates Social Media Team. Through the eight-week process, participants were introduced to social media basics, explored sexual and reproductive health and rights issues and practiced skills such as interviewing, blogging and editing.
“We embrace the role of technology in not only providing a space for community-building and psychosocial support for women living with HIV, but also the means to speak out about issues that affect them,” Ms. Polesana said.
To empower women living with HIV to meaningfully engage in decision-making spaces, ICWAP also held a feminist movement building training for women-led networks from six countries. This exercise built the capacity of women living with HIV to engage in programmes that promote gender equality and human rights and to lead advocacy efforts for high quality life-saving services for women and girls across the region.
On International Women’s Day 2023 under the theme “DigitALL: Innovation and technology for gender equality”, ICWAP called for the following:
- User-friendly digital platforms
- Access to the internet and digital tools
- Capacity building around social media advocacy
- Strengthened data security and redress mechanisms
- Online reporting mechanisms and rapid response for intimate partner violence
- Strategies to increase the economic empowerment of women living with HIV
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa




Feature Story
How harsh drug laws undermine health and human rights in Asia Pacific
01 March 2023
01 March 2023 01 March 2023Rosma Karlina and Bambang Yulistyo Dwi live with their two young children in the rainy hillside town of Bogor, south of Jakarta.
“Sometimes we go to museums to introduce the children to history or feed the deer at the Presidential Palace. It’s simple entertainment but can teach the children to learn to love even animals,” Ms. Karlina said.
If their family life is traditional, their work life is anything but. Ms Karlina is the founder and Director of Suar Perempuan Lingkar Napza Nusantara (also called Womxn's Voice), an advocacy and care organisation serving women and transwomen who use drugs. Bambang, popularly known as Tedjo, founded the Indonesian Justice Action Foundation (AKSI). Since 2018 his team has provided legal aid and support to people who use drugs, and advocated for their rights.
Their workdays are a mix of community organizing, paralegal paperwork and responding to distress calls. A client reported her husband’s domestic violence. When the police arrived at the house, the husband informed the police of her drug use and the police arrested her instead.
The organisations successfully advocated for a man to be released from a compulsory rehabilitation centre so that he could access HIV treatment. Otherwise, he would have gone three months without his medicines.
The organisations have witnessed many examples of women living with HIV being faced with extreme scorn. A police officer once threw a pack of sanitary napkins into a woman’s cell instead of passing it to her, saying it was because he was afraid to be near her.
“Since 2018 I have seen many rights violations perpetrated by law enforcement officers—abuse physically, psychologically and even financially,” Ms Karlina said. “They extort families to pay to enable their loved ones to go home.”
The Rosma Karlina of today—nurturer and fierce advocate—evolved from almost two decades of drug abuse. She has been to rehabilitation centres 17 times. Rock bottom came during an 18-month incarceration for heroin possession.
“My family paid a lot of money to the prosecutors, but I was still imprisoned. I lost custody of my oldest child. The judge thought I did not deserve to be a mother because I was a drug user,” she recounted.
Tedjo also evolved from addiction to activism.
“I did drugs between 1989 and 2015. It has been a long journey,” he reflected. “When my life was a mess, I hurt many people. It was not easy to prove that I was better.”
The couple are leading voices on how harsh criminal laws for drug possession and use lead to rights violations against people who use drugs while also lowering access to health services.
A 38-country legal and policy analysis by UNAIDS and UNDP found that 14 countries in the region have corporal or capital punishment penalties for the use or possession of drugs. Some states have condoned extrajudicial killings for drug offences. In 2021 an estimated 12% of new HIV infections in Asia and the Pacific were among people who inject drugs.
“The war on drugs has created a lot of stigma, and a culture that views an entire community as criminals. When we access healthcare, we get treated as bad people,” Tedjo said.
Regional Coordinator of the Network of Asian People who Use Drugs (NAPUD), Francis Joseph, explained that in the absence of legally conducive environments people don’t have access to appropriate services.
“Healthcare providers and law enforcement agencies treat them with violence and abuse,” he said. “So they don’t want to come out the closet and say ‘I have shared needles and syringes and I need an HIV test’. Because drug users are not welcome in our health facilities that leads to them going into the shadows and staying there.”
Lord Lawrence Latonio, a Community Access to Redress and Empowerment (CARE) partner and law student noted that Philippines also criminalises the possession of what are seen as drug paraphernalia. This means that peer educators who disseminate clean needles and syringes have to be watchful so they are not apprehended.
Fortunately advocates successfully lobbied for the country’s HIV and AIDS Policy Act of 2018 to include protections for healthcare workers who provide HIV services. Part of CARE’s work is legal literacy training so communities understand their rights. CARE also has a network of peer officers working in different regions to support members of key population communities and people living with HIV with seeking redress in cases where there have been rights violations.
Twenty-one countries in the region operate either state-run compulsory detention and rehabilitation facilities for people who use drugs or similar facilities. These are a form of confinement where those accused of, or known to be using drugs, are involuntarily admitted for detoxification and “treatment”, often without due process. Conditions have been reported to involve forced labour, lack of adequate nutrition, and limited access to healthcare.
In 2012 and 2020 United Nations agencies called for the permanent closure of these compulsory facilities. But according to a 2022 report, progress on this issue in East and Southeast Asia has largely stalled.
“UNAIDS is working with the United Nations Office on Drugs and Crime (UNODC) to support countries to transition from compulsory facilities towards voluntary community-based treatment that provides evidence-informed and human-rights based services,” said UNAIDS Asia Pacific Human Rights and Law Adviser, Quinten Lataire.
UNAIDS Indonesia is working with Womx'n Voice to pilot a multi sector partnership shelter and education program for women and children in Bogor. Interventions include social protection, legal support, mental health support, HIV and health education and accompaniment to services.
Ms Karlina called for increased investments in mental health care, poverty alleviation and education. “We need proper assessments to better look at each situation and come up with an effective solution. Prison is not the answer. If you see us as humans, you will take care of us as humans,” she insisted.
Region/country




Feature Story
LGBTQ+ shelter in Lviv provides lifeline to displaced Ukrainians
27 February 2023
27 February 2023 27 February 2023Oleg Kucherenko (not his real name) traveled from the eastern part of Ukraine to Lviv, in the western part of the country when his city, Kherson, was occupied by Russian forces. He, like many other representatives of the LGBTQ+ community was desperately looking for a safe place to stay.
His friend recommended the Facebook group of the Alliance Global - the largest LGBTQ+ organisation in Ukraine, who helped him find a spot in a shelter.
Once there, he got food, a place to sleep, and was able to contact friends and colleagues courtesy of electric generators and internet service. Up to ten people can stay in this particular shelter. The shelter administrator, Vadim Pryzenko, sees this as a lifeline.
“Our clients can get not only a place to live but also food and social and psychological support,” he said. “For those who are not living here, we provide humanitarian aid, food, hygienic products, and also individual financial support,” Mr Pryzenko said.
Since the war began a year ago, more than 7.9 million Ukrainians have fled abroad and another 6.5 million moved within the country.
Due to growing demand to find accommodation for internally displaced people that Alliance Global experienced, several organizations, including the Fondation de France, International Office of Migration (IOM) and UNAIDS’ Emergency Ukraine Fund, helped them set up the shelter. The shelter also provides health care and HIV services.
Mr Kucherenko got tested for HIV, hepatitis, and other diseases. His HIV test came back positive. He quickly met with a social worker, Andriy Kharatin, who accompanied him to the Lviv AIDS center where he got confirmation of his diagnosis, and additional tests.
"Several days later, with our help connecting him with to the health care system, Oleg started anti-retroviral therapy,” Mr Kharatin said.
Ukraine has the second - after the Russian Federation- biggest HIV epidemic in Eastern Europe and Central Asia (240 000 people are living with HIV according to 2022 estimates).
The country was making good progress in the AIDS response before the war – increasing the number of people living with HIV on antiretroviral treatment to nearly 60%.
However due to their destruction or occupation, more than 30 medical institutions providing HIV services have had to stop their operations, and logistics and supply chains have been broken. Despite this, Ukraine continues to help people living with HIV. Civil society has played a crucial role in adapting their response, engaging and reaching people in need.
“As a doctor, I am very pleased with the cooperation with Alliance Global,” said Dr. Olena Pavlishina from the Lviv Clinical Hospital. “Thanks to this cooperation we have the opportunity to be in touch with both internally displaced people and people who do not trust doctors much.”
In the past, she explains, a lot of the work was handled by health professionals.
“This part of the work that was previously done by health workers is now being done by social workers and civil society organisations,” she said.
And Mr Pryzenko doesn’t imagine that changing in the near future. He fears that if the war drags on, more people will come to the shelter and need services.
Meanwhile, Mr Kucherenko lives and works in Lutsk, not far from Lviv. He picks up his HIV medicine supply for three months and will get his next batch by mail when needed. He also stays in touch with his social worker for psychological support online.
Region/country
Related




Feature Story
“Silence is better” — How the criminalisation of sex workers keeps exploitation in the shadows
28 February 2023
28 February 2023 28 February 2023As a girl Ikka dreamed of becoming an accountant. She knew her parents could not afford to send her to university, so she resolved to pay for university herself by moving into a brothel. For almost three years she lived and worked there while studying.
Davi’s parents divorced when he was a baby and he was raised by caring grandparents. In high school he led lots of extracurricular activities. He was also gay. Just three months before his final exams Davi was raped by a teacher who threatened to “out” him. He ran away to the city. After a desperate search for work, he landed a job in a massage parlour.
From the Bangkok offices of Youth LEAD and the Asia Pacific Network of People Living With HIV and AIDS (APN+), the pair reflects on those chaotic adolescent years with halting candour. They unpack layers of vulnerability and abuse—the way poverty and trauma can propel young people toward sexual exploitation, higher HIV risk and a cascade of rights violations. And they say that the criminalisation of sex work only made their situations worse.
“No one tells you anything other than that you need to please your client. Just be submissive and quiet. There’s no protection, no information, no nothing,” Ikka remembers.
The brothel would occasionally force the women to undergo HIV and STI testing. Saying ‘no’ wasn’t an option. But when Ikka went to a clinic on her own to get condoms or contraceptives, she was turned away.
Customers sometimes didn’t pay, became violent or refused to stop having sex after even two or three hours. Abusive clients routinely threatened to report them.
“If someone called the police, they would arrest the sex worker. The customer is king,” Davi says. “So silence is better.”
“The police wouldn’t take your report. They think they have more important cases than you,” Ikka adds.
UNAIDS Asia Pacific Human Rights and Law Adviser, Quinten Lataire, explained that criminal laws against sex workers make it very difficult for sex workers to demand basic rights, substantially increasing their risk for abuse and exploitation, such as from law enforcement officers.
“The criminalization of sex workers does not end sex work. It simply makes people go underground, putting them at higher risk of violence and HIV transmission. This has a devastating impact on the sex workers themselves, their clients and the society at large,” Mr Lataire said.
Almost all (99%) new HIV cases in young people in Asia Pacific are amongst key populations and their sexual partners. In Cambodia, Indonesia, Lao PDR, the Philippines and Thailand, youth account for between 40% and 50% of new infections. Since 2010, HIV rates among young people have risen in Afghanistan, Fiji, Malaysia, Pakistan, Papua New Guinea, the Philippines and Timor-Leste.
At ages 18 and 19 respectively, both Ikka and Davi learned that they were HIV positive. In Ikka’s case she was tested as a VISA requirement for a student exchange programme. Her results were forwarded to her school even before she got them and she was kicked out. From breach of confidentiality to discrimination in both education and healthcare settings—one rights violation after another. Ikka had the agency to confirm her HIV status at a community-based sex worker clinic she’d looked up and immediately started treatment.
Davi voluntarily tested with a community organization that visited the massage parlour to conduct sensitization sessions and offer services. He kept his status a secret at work but began attending support meetings on the weekend. He sometimes told the pimp that he was going out to meet a client, handing over the stipend he got from the organization when he got back.
“For eight months after I knew I was positive, I felt like I didn’t want to do sex work, but I needed the money. I told clients to use condoms but some of them would give me more money not to,” Ikka remembers.
The events that finally prompted her to leave the brothel still evoke strong emotions. Her best friend there also contracted HIV.
“I told her, ‘let’s go together to get antiretroviral treatment’. I showed her my medication as evidence. But she didn’t want to go. She would not get support from her parents and if the pimp found out, he would kick her out. She felt it was better to die,” Ikka remembers. Her friend passed away just two months after her diagnosis.
In both cases these young people demonstrated incredible resilience and were supported by community-led organizations with tailored services for sex workers and people living with HIV. Ikka joined an organization addressing sex workers’ rights, health and social support needs. She quickly carved a niche representing the interests and perspectives of young sex workers. She would go on to lead national young key population organizations and sit on the Global Fund’s Youth Council. Today she is the Regional Coordinator of Youth LEAD.
“I told myself I needed to help my community,” Davi says. “I don’t want no more people in my situation; no more students becoming victims of sexual violence; no more 19-year-olds HIV positive. I just chose to leave (the parlour) and volunteer with the community organization instead.” Encouraged and supported by community, Davi would go on to graduate from high school and earn a sociology degree. He is now aiming for a Masters qualification while working as APN+’s Youth Officer.
The issues Ikka and Davi faced remain today.
“I still use a condom, but many clients refuse,” says Rara, a 22-year-old sex worker. “When we’re desperate for money, we have no choice but to agree. In addition to gonorrhea, I got syphilis and got treated for it. Thankfully I’m still HIV negative.”
UNAIDS and the Inter-agency Task Team on Young Key Populations are working to address the inequalities faced by young key populations in Asia Pacific. Learn more about their work.
Region/country




Feature Story
Thailand partners develop community-led HIV care curriculum
23 February 2023
23 February 2023 23 February 2023For 20 years Kochaphan Wangtan has been a community health worker, serving other people living with HIV (PLHIV) in Thailand.
“I’ve seen many friends living with HIV come to care very late with opportunistic infections,” she said.
“I focus on helping to bring them in and provide support to start antiretroviral treatment right away and I also conduct home visits, counselling and psychosocial screening so I can link them to services they need,” Ms Wangtan explained.
Ms Wangtan is from the Jai-Prasan-Jai Comprehensive Continuum of Care Center (CCC) from the Phan District Hospital in Chiang Rai province. She is one of almost one thousand PLHIV health workers who are embedded in more than 230 Thai hospitals and serve almost 60,000 PLHIV annually.
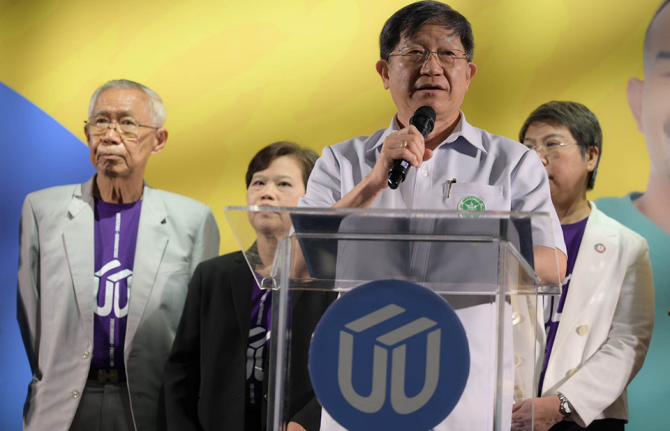
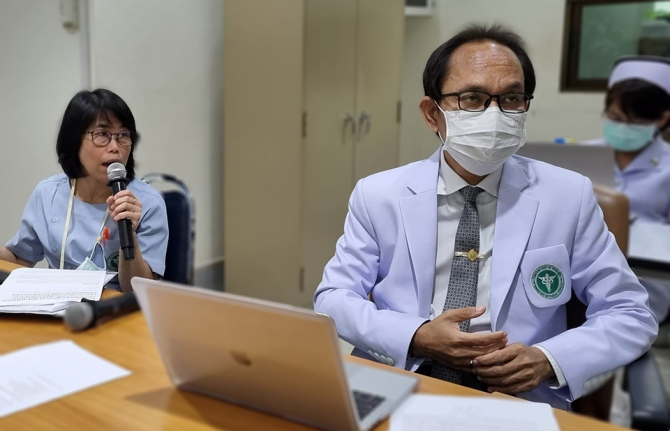
For the first time, the country has rolled out a national community health worker certification for these volunteers. The initiative is called “A Comprehensive Continuum of HIV/AIDS Care and Support for and by People living with HIV.” The curriculum was developed by the Ratchasuda College of the Mahidol University through close collaboration with the Thai Network of People Living with HIV/AIDS (TNP+) as well as support from the Health Ministry’s Division of AIDS and STIs and the National Health Security Office. USAID-PEPFAR via the III Unify Collaboration Programme and UNAIDS provided technical and financial support.
“PLHIV volunteers have provided the first community engagement in the HIV response since the start of the epidemic in Thailand,” said UNAIDS Country Director, Patchara Benjarattanaporn. “Peer-led support boosts treatment initiation and retention and is central to the HIV response,” she said. This initiative ensures that PLHIV-led health services are standardized, recognized and valued.
Two modules are delivered over 90 hours. The first module focuses on theoretical training, including on holistic follow-up care, treatment adherence counselling and developing a comprehensive service plan. The second module is practical. Along with its HIV focus, the curriculum also integrates tuberculosis, sexually transmitted infections, Hepatitis C and non-communicable diseases. Earlier in the month the first cohort of 46 PLHIV health workers received their certification.
Dr. Wachara Riewpaiboon, a rehabilitation physician and former Ratchasuda College Dean, developed the curriculum.
“The health system is not only for health professionals… It belongs to everyone,” she said. “Getting an HIV diagnosis does not help clients understand what they are facing. When people living with HIV tell their story, it is very different knowledge they are imparting. The knowledge that helps people make decisions for themselves usually comes from peers, not doctors.”
For her, care goes beyond medicine.
“It is not only biology that we are dealing with, but also psychology and our interaction with our social environment—how people look at people living with HIV and how they perceive themselves,” Dr Riewpaiboon continued. “It is very important to help people see the positive side of their experience.”
According to Nurse Chulaporn SingPae, an HIV Coordinator at the Phan District Hospital, PLHIV volunteers help with counselling, adherence, missed appointment follow-up, home visits, treatment deliveries, overcoming stigma including self-stigma and promoting understanding of U=U, undetectable equals untransmittable. (An undetectable viral load means the virus is not transmittable aka untransmittable.) The training ensures that these contributions are recognized by the health system as meeting quality standards.
Now that the course has been developed and tested, the curriculum has been recognized by the National Health Security Office (NHSO). Thai civil society organizations, who provide HIV and STI services with certified community health workers have been accredited and are eligible to register as health service units in the Universal Health Coverage scheme. Having supported the development and pilot of the curriculum, UNAIDS is now supporting a study to cost these services. The office is also working to promote sufficient and sustainable financing for community-led health services for PLHIV and key populations.
“This training is going to become the guarantee that a peer educator provides a high quality of service, in a holistic way, which encompasses not just the physical but also the mental, emotional and social aspects,” said Apiwat Kwangkeaw, Chairperson of the Thai Network of People living with HIV/AIDS. “As this becomes institutionalized, we are sending a message to the health system as a whole to let the community of peer educators be an equal partner,” he said. Mr Kwangkeaw hopes this will translate into sustainable domestic financing for community-led health services and better quality of life for PLHIV.
Region/country




Feature Story
By bringing an end to societal and economic inequalities, we can end AIDS in Tanzania
05 December 2022
05 December 2022 05 December 2022Following a one-week visit to Tanzania and Zanzibar to launch the 2022 Global World AIDS Day report; to commemorate World AIDS Day; and to see first-hand the extraordinary work of joint efforts by the government, partners and communities to end AIDS in Tanzania and Zanzibar, UNAIDS Executive Director Winnie Byanyima issued the following statement:
“I observed strong commitment from the Government of Tanzania, our partners and activists at the frontlines fighting the HIV epidemic.
In particular, I thank Tanzania for hosting the launch event of this year’s World AIDS Day report “Dangerous Inequalities” on 29th November in Dar es Salaam, and for inviting me to join the World AIDS Day commemoration on 1st December in Lindi, Tanzania.
For the report launch, I thank our guest of honour, Hon. Minister George Simbachawene, Minister of State in the Prime Minister’s Office, for committing to end inequalities to end AIDS in Tanzania. The civil society representative, Chair of the National Council for People Living with HIV, Ms Leticia Mourice Kapela, added the commitment of communities to the theme “Equalize”, as did Deputy Minister of Health, Hon. Godwin Modell, on behalf of the Ministry of Health.
We are honoured by Her Excellency President Samia Suluhu Hassan leading the World AIDS Day commemoration, and grateful for her Government’s commitment to ending the AIDS pandemic. H.E. President Hassan spoke powerfully on the need to overcome inequalities in the AIDS response and called on TACAIDS to reduce inequalities, prevent new HIV infections and address stigma and discrimination. I commend H.E. President Hassan for her country joining the Education Plus Initiative in the lead up to World AIDS Day.
I also congratulate Tanzania for being the first country to join the Global Alliance to End AIDS in Children and I thank H.E. President Hassan for agreeing to host and participate in the launch of the Alliance early next year. No baby should be born with HIV, and no child living with HIV should be without treatment.
I welcomed the opportunity to visit the Mukikute Harm Reduction programme in Tanzania, which gives hope and dignity to people who inject drugs. I was uplifted by the passion of this community to mobilize and empower.
I was equally grateful for the opportunity to meet with allies, including ZAPHA+ and the Zanzibar Key and Vulnerable Population Forum (ZKVP-Forum).
Over the past 12 years, Tanzania has been able to reduce new HIV infections by almost 50% and to cut AIDS related deaths by 50%. 86% of Tanzanians who live with HIV are on treatment. I congratulate Tanzania on their leadership in the AIDS response. Together, with the required commitment and resources, and by bringing an end to societal and economic inequalities, we can end AIDS as a public health threat by 2030.
In closing let me reiterate the commitments that I made to Tanzania and Zanzibar in our joint efforts, namely to:
- Strengthen UNAIDS presence in Dodoma, the national government capital of Tanzania, to support TACAIDS, Ministry of Health and other Ministries in the AIDS response.
- Collaborate with the Ministry of Health in hosting the Ministerial launch of the Global Alliance and the development of the country action plan.
- Move forward Education Plus in Tanzania by ensuring that more children get enrolled in and complete secondary school.
- Support Tanzania and Zanzibar in the funding request application for the Global Fund HIV/TB grant.
- Support and strengthen collaboration between the governments of Tanzania and Zanzibar and networks of people living with HIV and other community groups that are vulnerable and at high risk for HIV infection.
I thank the government, civil society and partners of Tanzania and Zanzibar for my visit.
Region/country
Related



Feature Story
Preventing transmission and tackling stigma: The power of U=U
12 December 2022
12 December 2022 12 December 2022U=U, which stands for Undetectable = Untransmittable, is a vital public health message for the HIV response. Undetectable = Untransmittable means that people living with HIV who achieve an undetectable viral load through consistent antiretroviral treatment and monitoring cannot transmit HIV. As Thailand has shown, the message of U=U also helps in combatting the stigma which people living with HIV can face in healthcare settings and wider society.
U=U is a priority activity in Thailand’s 2017 – 2030 National Strategy to End AIDS. The approach has already been tested in the capital city, Bangkok. A same-day treatment initiation programme there has resulted in more than 95% of people on treatment achieving viral suppression after just six months of antiretroviral therapy. The national initiative brings together Thailand’s Institute for HIV Research and Innovation (IHRI), the Department of Disease Control, the Ministries of Public Health, Education and Labor, the National Health Security Office, and the Subcommittee on the Promotion and Protection of AIDS Rights, supported by UNAIDS.
Thailand’s wider HIV response has achieved strong results, with an estimated 94% of people living with HIV aware of their status, 91% of diagnosed people on treatment and 97% of those on treatment virally suppressed. But despite these successes, barriers remain as a result of stigma. There are too many late diagnoses, and some people remain fearful about accessing HIV services. To increase use of HIV services, to achieve U=U for all people living with HIV, it is vital to ensure that every person is treated with respect and dignity by the healthcare system.
Dr. Nittaya Phanuphak, Executive Director of the IHRI, emphasized that knowing one’s HIV status is the critical first step to enrolling in antiretroviral treatment.
“People at risk of contracting HIV and people living with HIV from all groups in Thailand must have equal and convenient access to HIV testing and, if positive, to antiretroviral treatment as soon as possible, which will lead to U=U,” said Deputy Minister of the Public Health Ministry, Dr. Sopon Makthon.
Thailand’s U=U initiative embraces a community-led approach which enables people living with HIV to support others who are newly diagnosed to start and stay on antiretroviral treatment. “Community leadership is vital to communicate U=U effectively,” said Patchara Benjarattanaporn, UNAIDS Country Director for Thailand. “This will help tackle stigma and self-stigma, and help boost positive health-seeking behavior.”
Apiwath Kwangkaew, president of the Thailand HIV/AIDS Network, urged all health workers to amplify the message of U=U: “Today's medical personnel must confidently explain U=U to enable social understanding. Health services must be brave and speak up. New understanding will bring change,” Mr. Kwangkaew said.
“UNAIDS welcomes amplification of the message that U=U. It is key to reaching the goal of zero new HIV infections, zero discrimination and zero AIDS-related deaths,” concluded Taoufik Bakkali, UNAIDS’ Regional Director.
Region/country




Feature Story
Thailand’s Mplus: HIV services delivered in style
13 December 2022
13 December 2022 13 December 2022“This isn’t your mother’s clinic!” said one amazed visitor.
From banners to brochures, all promotional materials are slick and cheerful. Smiling faces and toned torsos are everywhere. A purple colour scheme covers the whole building. Even files and staff face masks are colour coordinated. A pair of Facebook Live hosts have the good looks and energy of K-pop stars. And the organization’s slogan is decidedly upbeat: “where community fulfills your happiness”.
Over almost two decades, Thailand’s Mplus Foundation has refined a unique approach to providing comprehensive HV services to key population clients including men who have sex with men and transgender women.
Their method goes far beyond a cool brand identity. Mplus has leveraged domestic and international partnerships to create a key population-led health service with impressive results. They dispense more than half of the PrEP in Thailand’s Chiang Mai province.
This year they tested 95% of the almost 8000 people they reached with face-to-face services. Of those who tested positive, 91% were placed on treatment while the other 9% are in follow-up case management. And 100% of their clients who received viral load testing were found to be virally suppressed.
“Community organizations can best reach key populations to receive services. We find that people who do not want to get tested at the hospital are comfortable with peers who they know understand their life,” explained Pongpeera Patpeerapong, Director of the Mplus Foundation.
Since its formation in 2003 Mplus has evolved to deliver a full range of services. They now have health centres in four provinces, while their mobile testing units serve clients in another five districts. They support a local hospital in each province, linking people to care and helping them with adherence. Mplus provides rapid testing, CD4 and viral load monitoring, and is also authorized to dispense medication. A small fleet of motorcycles even makes PrEP deliveries to clients in remote areas.
Both their online and offline engagements are anchored by a peer-led strategy. Their social media presence is commanding—everything from Twitter to Tik Tok. There are closed Facebook groups and special applications for clients to connect with community. Offline, they go beyond information booths to host parties and sport meet-ups. These aren’t just bonding exercises. Clients book appointments online and face-to-face interactions usually result in receiving an HIV test.
Mplus also provides technical assistance to other countries. It has supported an organization in Laos with online interventions and helped community groups in Cambodia develop campaigns to promote PrEP.
They played a key role in advocating nationally for the accreditation of community health workers. All Mplus staff are certified by the Department of Disease Control following a rigorous programme of study, evaluation and practice.
The programme continues to progress. Mplus is strengthening their mental and emotional health support offering, and is working towards becoming certified to provide HIV and sexually transmitted infection (STI) treatment.
While in the past the programme was more heavily funded by the U.S. President's Emergency Plan for AIDS Relief through the United States Agency for International Development, today half of their investments come from branches of the National Health Security Office.
“Domestic funding is very important to develop our systems,” Mr. Patpeerapong said. “Community-based organizations have to be able to access domestic funding to cover more issues, including stigma and discrimination.”
Empowering key population-led health services has been crucial in improving Thailand’s HIV programme results. One of five people living with HIV in Thailand were identified and referred by a key population-led health service under the domestic health financing scheme. Four out of five people on PrEP in the country are served by community-led organizations. These services play a critical role in Thailand’s strategy of Reach, Recruit, Test, Treat, Prevent, Retain.
“Thailand is well-positioned to be a leader in addressing the need for a sustainable community-led response as a critical part of the health infrastructure,” said UNAIDS Country Director for Thailand, Patchara Benjarattanaporn. “By creating an enabling system for health outreach we can address the challenge of late diagnosis and better reach key population communities with services.”
Thailand has integrated HIV services into its Universal Health Coverage scheme and increased investments in key population- and community-led health services. UNAIDS Programme Coordinating Board (PCB) members visited Mplus and other community-led health services ahead of the 51st PCB meeting in Chiang Mai, Thailand.
Region/country


Feature Story
Tanzania commits to invest in secondary education as part of efforts to keep boys and girls free from HIV
16 December 2022
16 December 2022 16 December 2022Tanzania became the 13th African country to join the Education Plus Initiative, committing to provide greater investments to ensure boys and girls complete secondary school.
Education Plus is an initiative spearheaded by UNAIDS to accelerate action and investments in education to prevent HIV. Evidence shows that completing secondary education reduces the risk of HIV infection and early pregnancy and improves their livelihoods and prosperity for girls and young women. The education Plus initiative is centred on empowering adolescent girls and young women and achieving gender equality in sub-Saharan Africa.
On 30 November 2022, during the HIV week commemoration, the Office of the Prime Minister, led by the Minister of State for Policy, Coordination and Parliamentary Affairs, Mr George Simbachawene, alongside the Deputy Minister of Health Dr Godwin Mollel, launched the initiative in Lindi region, Tanzania.
"Young people aged 15-24 years make up one of the largest groups of new infections, among all new infections every year, approximately 30% are among people aged 15–24. That means for every 10 new infections, three are from this age group,'" said Mr. Simbawachane
The launch of Education Plus in Tanzania will accelerate the ongoing country's adolescent education, health and wellbeing agenda. Tanzania has been particularly affected by HIV. In 2021 around 1.7 million people were living with HIV; 74% of new HIV infections among young people aged between 15 and 24 were among young women, showing the disproportionate impact HIV is having on young women and girls.
Minister Simbachawene said the country would increase primary education opportunities for adolescents and enable them to stay in school by removing all barriers to completion of primary and secondary school education. Through the initiative, Tanzania will strengthen efforts to bring HIV education, reproductive health, and life skills to adolescents inside and outside of school.
The initiative comes at a time when Tanzania has made good progress in adopting global treaties and agreements to address gaps in education and health rights and increase opportunities for girls and boys. Most commitments have been translated into national policies and strategies, as demonstrated by the government’s commitment to offering free basic and secondary education. Tanzania has also adopted policy decisions to implement a re-entry program for children who drop out and to include comprehensive sexuality education into the curriculum. The country has also amended the HIV and AIDS Act to lower the age of consent for HIV testing and allow HIV self-testing.
The minister also pledged to do more to eliminate gender-based and sexual violence by providing youth-friendly education, skills building, and enhancing referrals by connecting youth to health and community services.
However, key gaps remain, with national surveys showing increased rates of teenage pregnancy, school dropouts, and high levels of gender-based violence. Around 27% of young women aged between 15 and 19 years already have a child or are pregnant and 50% of ever-married women aged between 15 and 49 report experiencing physical, sexual, or emotional violence.
The total number of students enrolled in secondary education is still below 50%, and for those in school, there is a high dropout rate, and some do not complete their schooling. The country has a low completion rate in secondary schools at 11.3%, and dropout in secondary schools due to pregnancy was reported at 4% in 2020.
Despite increased political will and significant achievements, women's and girls' vulnerabilities remain very high. Adolescent girls and young women in Tanzania continue to shoulder the burdens of domestic work, gender inequality in education, and harmful norms. Many are entrenched in cycles of poverty and extreme vulnerabilities.
At the launch, the government committed to strengthening policies to facilitate the provision of education and essential skills to prepare and equip young people for employment and other economic opportunities.
The launch was attended by key partners including Dr Leonard Maboko, the Executive Director for Tanzania Commission for AIDS (TACAIDS) youth representative Pudensiana Mbwiliza; Permanent secretary office of the Prime Minister, Dr John Jingu and Hon Judith Nguli from Lindi Regional Commissioner’s office and Tanzania PEPFAR coordinator Jessica Greene; representatives from UNAIDS, UNESCO, International Labour Organisation (ILO), UNICEF and the World Health Organisation (WHO).
The event brought together civil society organisations, young people’s networks, and representatives of people living with HIV and partners. Co-lead by five United Nations agencies working with governments, women’s and youth movements; the initiative is of even greater urgency as the COVID-19 pandemic has pushed millions of African girls out of school.
Region/country
Related



Feature Story
The power of bringing together government and community HIV services
15 December 2022
15 December 2022 15 December 2022The Sanpatong Hospital in North Thailand has reinvented and refined its HIV programme for more than three decades. It began attending to people living with HIV in 1989, and in 1996 started offering antiretroviral treatment.
“We have patients who have been with us for 30 years,” says Dr Tawit Kaewprasert, Deputy Director of Provincial Public Health Office and Director of Sanpatong Hospital.
In the last five years the hospital has not had a single case of mother-to-child HIV transmission. An impressive 96% of people on treatment who received viral load tests there this year were virally suppressed, with 98% of those patients being undetectable. Management speaks about the 92% retention rate for clients who were on treatment in 2022 in terms of how those results can be improved.
“We have not achieved that target just yet,” Dr Manusin Kongka says, referring to the proportion of people who stayed on antiretroviral therapy. “But we can reach the target and even achieve beyond 95%.”
The team even aims to achieve 100% viral suppression among people who have been on treatment for at least five years. The current 96% result isn’t considered to be good enough.
This ambitious goal-setting flows from the National HIV Policy and Thailand’s commitment to end AIDS by 2030 through a well-articulated strategy to reach, recruit, test, treat and retain people in care, while also working to prevent new infections.
Of course the strategy relies heavily on Sanpatong and institutions like it. This 130-bed facility boasts a central lab that serves surrounding hospitals in Chiang Mai, Lamphun and Mae Hong Son with HIV diagnosis, CD4, viral load monitoring and some opportunistic infections testing.
Their approach includes the adoption of HIV response best practices including PrEP, index testing and same-day treatment initiation.
“Patients can start treatment before they even get their CD4 result,” Dr Kongka explained.
All staff have received anti-stigma training as well as orientation around the U=U, undetectable = untransmittable, initiative. The facility uses a differentiated approach for antiretroviral treatment delivery. Depending on their health status, some clients can collect multiple month dispensing at district health promoting hospitals while others can receive their medicine by mail.
But a major key to Sanpatong’s success is the linkages it has made with groups of community-led organizations to drive case detection, linkage to care, psychosocial support and the monitoring of services. The Hospital works with Mplus, CAREMAT and FHI360 on prevention, testing and retention in care. Organizations of people living with HIV run support groups. The Community Led Monitoring team even helps primary care nurses to contact patients who have been lost to follow up and conduct home visits. The people living with HIV network collaborated with key community-based organizations in Chiang Mai to conduct community-led monitoring to improve the quality of HIV services at the Sanpatong hospital.
“Our collaboration with community organizations increases awareness about HIV, improves quality of care and access to care, decreases the waiting in community clinics and increases continuity of care for HIV patients,” said Ms Sineenuch Suwansre, HIV Coordinator.
This close collaboration with communities is enhanced by the Thailand Government’s move to integrate HIV services into the Universal Health Coverage scheme. Now certified organizations and lay HIV service providers can access domestic financial support within the national health infrastructure.
“Universal Health Coverage is a mechanism for the sustainable financing of HIV prevention as well as sustainable financial support to key population- and community-led health services. The Thai government’s move to fund Community-led Health Services as an element of the mainstream public health system is a win for people living with HIV, for HIV prevention and for sustainability,” said UNAIDS Thailand Country Director, Patchara Benjarattanaporn.











