



Feature Story
With UNAIDS’ support, everyone counts
28 January 2019
28 January 2019 28 January 2019For five weeks in 2018, teams of up to 10 people in each of 120 clinics and hospitals across Lesotho sifted through more than 180 000 records of people diagnosed with HIV and receiving care. The goal: to count the number of people living with HIV who were on treatment in June 2018.
During the long and dusty days, the teams attached green stickers—indicating active on treatment—or other coloured stickers—specifying that a person had defaulted, transferred or died—to nearly 80% of all patient files in the country. Facility by facility, counts of the number of people found to be active on treatment were compared to counts previously reported to the Lesotho Ministry of Health and other partners, including the United States President’s Emergency Plan for AIDS Relief. All of this to confirm that the country’s reporting adds up.
“Together with our team, we reviewed the treatment status of more than 5000 people at the Senkatana Clinic in Maseru, Lesotho, one of the oldest and busiest treatment centres in the country. After two days of reviewing the paper-based files, we found about 30% more people on treatment than the clinic had reported to the Ministry of Health in June 2018,” said Motselisi Lehloma, Ministry of Health Officer. Overall, the exercise found an underreporting to the Ministry of Health of 3% for all the 120 facilities visited.
Since early 2017, UNAIDS and other international partners have supported more than 15 countries, primarily in sub-Saharan Africa, to verify that the number of people reported currently to be on treatment is accurate. This work also supports facilities to improve the accuracy of the data reported through their health information systems by reviewing patient registries and processes for collecting, aggregating and reporting treatment numbers.
“The exercise that Lesotho undertook to audit and validate treatment numbers underscores its commitment to accurately monitor programme impact,” said Kim Marsh, Senior Adviser, Epidemiology and Monitoring, UNAIDS. Thanks to these efforts, and the efforts of many other countries in the region, UNAIDS and stakeholders can be confident in treatment numbers that allow us to monitor progress towards 90–90–90. Through debriefings with clinical staff and written reports, minor deficiencies were addressed on the spot and larger systematic issues were brought to the attention of the ministry and implementing partners in order for them to adopt necessary corrective actions.
Lesotho has one of the highest burdens of HIV in the world. In 2017, 320 000 people were living with HIV in the country, an HIV prevalence of 23.8%.
Region/country
Related






Feature Story
Shelter founder reflects on 15 years of combining HIV treatment, care and prevention with faith
27 January 2019
27 January 2019 27 January 2019On the final morning of the 2019 World Youth Day Commemorations in Panama, Pope Francis will visit the Casa Hogar del Buen Samaritano. Named for the Biblical parable of the Good Samaritan, this shelter on the outskirts of Panama City offers comprehensive care to help people living with HIV recover and reintegrate into society.
Their only requirement for entry is need. As a policy, the home welcomes people regardless of sex, age, religion, occupation, sexual orientation, ability or geographical origin.
As volunteers zipped back and forth in feverish preparation for His Holiness yesterday, Buen Samaritano founder and Director, Father Domingo Escobar, took a moment to reflect on the evolution of the home.
It had begun as pastoral work carried out from the Parish of Santa Maria del Camino. People living with HIV—many of them homeless—would look to the church for comfort, counsel and food. The idea began to crystallize that the most marginalized needed more structured support. The Buen Samaritano Foundation and Home were founded 15 years ago with the broader vision of helping build a society free from discrimination, prejudice and stigmatization.
“I believe that it is necessary to highlight the dignity of the human being and to respect the other person, considering that we are all—as the Bible says—the Temple of the Holy Spirit… each one of us,” Father Escobar explained.
Since its inception, the Buen Samaritano has served more than 300 residents. The combination of spiritual care with medical treatment is key. By bolstering their faith, patients steadily become more optimistic, more “enthusiastic” about taking their medicines and more confident that their treatment will work. According to the Buen Samaritano Director, the most significant factors undermining people’s treatment adherence are lack of support and fear of prejudice.
“Because of fear of rejection and of discrimination they keep it to themselves and do not share it with family or with others,” he said.
In direct response to this challenge, one branch of the foundation evolved specifically to serve people living with HIV who live with their families but have limited resources. Apart from food and medicines, Buen Samaritano provides sensitization and training for family members, strengthening their ability to provide emotional support for their loved ones.
The foundation has also reached beyond HIV care and treatment to support prevention efforts through seminars and interventions for children, young people including youth at risk, and adults. Last year their prevention programmes reached more than 4500 people. Their Youth Information program promotes “sex education with values” in secondary schools.
UNAIDS has partnered with Buen Samaritano for many years, helping to broker the provision of antiretroviral medicines from the Ministry of Health, as well as partnering around visibility and advocacy.
The work of Father Domingo with underserved people living with HIV in Panama shows the incredible capacity of faith communities to build bridges, not only around treatment and care, but also around eliminating stigma and discrimination and prevention.
The foundation provides a valuable contribution to the community, country and AIDS response. In Panama, an estimated 25 000 people are living with HIV. The country has achieved strong progress related to treatment and reducing mortality. Three-quarters (76%) of diagnosed people in Panama were on treatment by the end of 2017 and there were fewer than 1000 AIDS-related deaths. But with an estimated 1600 new infections that year, the need for strengthened prevention initiatives is clear. For Father Escobar the challenge requires all hands-on deck.
“We must all feel and understand that the task of prevention is a cross-cutting challenge,” the priest explained. “It has to be present in the family, in public policy, in childhood, for the youth and in pastoral work. It is a problem for all, and we can all contribute.”
Region/country
Related



Feature Story
She Conquers in South Africa
24 January 2019
24 January 2019 24 January 2019When she was four years old, Selokela Molamodi’s teacher asked the class what they wanted to be when they grew up. While her classmates volunteered more conventional professions, such as nurses, doctors and lawyers, Ms Molamodi’s answer, given with a fiery determination, was, “I want to be Minister of Education.”
Her love for education, and her characteristic fieriness, has stood 19-year-old Ms Molamodi in good stead. Last year she graduated top of her class, having been head girl in both primary school and high school. Armed with an unshakeable self-confidence and her core principles of transparency, honesty and humility, Ms Molamodi has avoided the fate of many young South African women—HIV infection, unintended pregnancy and an abandoned high school education.
She says she has had to deal with the same harsh realities as other young women—financial difficulties, crime, violence, peer pressure, the temptation of “blessers” [older men] and drug and alcohol abuse. Staying in school kept her focused, she explained.
“There are still a lot of misconceptions about HIV among young people. Sex is not talked about openly. Young people are given knowledge about sexual and reproductive health, but they are not given knowledge on how to make a decision about sex.”
“There are still a lot of misconceptions about HIV among young people. Sex is not talked about openly. Young people are given knowledge about sexual and reproductive health, but they are not given knowledge on how to make a decision about sex,” she says.
In South Africa, 1500 young women and adolescent girls between the ages of 15 and 24 are infected with HIV every week. They accounted for 29% of all new HIV infections in the country in 2017. Research has shown that older men, generally five to eight years older, are mostly responsible for passing on HIV to younger women; once women reach their mid-twenties, they pass on the virus to men their own age.
“There is a perception among young women that we should have a high number of sexual partners when we are young because that is what it means to be free. Then, when we reach our mid-twenties we will leave that life behind and settle down. But girls don’t understand that they don’t have control over these sexual relationships, that their consent doesn’t count,” she says.
To start a dialogue about these and many other issues facing young women, Ms Molamodi started You for You while she was in her final year of school.
“I call it a movement, not an organization,” says Ms Molamodi. “It is about accepting and loving yourself for you. While we can exist as a community and a collective, we must first love ourselves as individuals,” she says.
Ms Molamodi, along with two friends who started the movement with her, have one-on-one mentoring sessions with other young women on issues such as self-esteem, body positivity, sexual and reproductive health and drug and alcohol abuse. She has also organized two events that focused on empowering young women as leaders “so we can rise as young women and stand up against discrimination, together.”
She looks at DREAMS—the initiative led by the United States President’s Emergency Plan for AIDS Relief—as the matriarch of a family of young women like her. In South Africa, DREAMS works closely with She Conquers, a government-led national campaign aimed at empowering young women and adolescent girls to take responsibility for their health.
“Yes, give girls access to discrimination-free HIV prevention and treatment services and family planning, but also ask for our feedback. Give us education and information and teach us that actions have consequences which are responsible for our progress or regress.”
“DREAMS/She Conquers has provided us with a space to have natural conversations about things that affect us as young women with other young women. It gives us a voice and brings enlightenment to us. For instance, most of the girls I know have tested for HIV, but none of them ever got to talk about it, until DREAMS/She Conquers came to our school,” she says.
“These are the kinds of initiatives that increase the effectiveness of what UNAIDS is trying to achieve,” says Ms Molamodi. “Yes, give girls access to discrimination-free HIV prevention and treatment services and family planning, but also ask for our feedback. Give us education and information and teach us that actions have consequences which are responsible for our progress or regress.”
She says she would like to see conversations about HIV prevention and sexual and reproductive health being brought together more often with those about careers, empowerment and entrepreneurship.
As for her ambition for You for You, “I want to help grow a continent of young women who are confident enough to speak out; who are able to stand up for each other and empower each other. If I have someone say, “I did not give up” then I know I had a purpose; that I was someone’s reason not to give up.”
Region/country


Feature Story
Oral fluid HIV testing for gay men and other men who have sex with men in the Lao People’s Democratic Republic
17 January 2019
17 January 2019 17 January 2019Only one third of gay men and other men who have sex with men know their HIV status in the Lao People’s Democratic Republic, partly because stigma and discrimination remains a barrier for accessing HIV testing in public hospitals and clinics. Complicated protocols, uneven and at times judgemental treatment by health providers and non-confidentiality of testing results further impact on HIV testing.
“Many of our friends are scared of getting an HIV test because they think the testing steps are challenging and often unfriendly,” said Phoulikhan Siphabouddy, a community-based supporter of LaoPHA, a Lao nongovernmental organization.
To address this, USAID supported the government and LaoPHA to pilot oral fluid screening in three provinces.
Most people assume that testing involves taking a blood sample. But oral fluid testing detects antibodies for HIV, not the virus itself. A test swab is gently wiped along a person’s upper and lower gums once, then the swab is placed inside a test tube containing a reagent. The result is known within 20 minutes.
Members of the community, so-called peer educators, train volunteers for the oral fluid screening. The screening is fast, easy and can be done anywhere.
Around 82% of people reached agreed to have an HIV test through oral fluid screening, compared to only 17% of referrals to clinics, according to the Ministry of Health.
“The new approach dramatically exceeded Laos’ HIV testing targets by more than 200%,” said Bounpheng Philavong, Director of the Lao Centre for HIV/AIDS and STI.
He, along with LaoPHA, are convinced that community-led services provide an enabling environment for key populations to access HIV services in a non-discriminatory manner. Linkages to care and support for people living with HIV has also improved for people who test positive, with the same community volunteers providing support for referral to trusted clinics.
Related information
Region/country




Feature Story
Traversing rivers and jungles to reach indigenous peoples in remote parts of Brazil
10 January 2019
10 January 2019 10 January 2019Indigenous health worker Jijuké Hukanaru Karajá works as a nurse in the Indigenous Health District of Araguaia, named after one of Brazil’s major rivers located in the eastern Amazon basin. She has been working with indigenous peoples for many years and criss-crosses between Brazil’s cities and indigenous villages to provide crucial health services. Ms Karajá feels very proud to be a part of the Brazilian indigenous public health system, having followed in her father’s footsteps.
“I’ve worked in town and in my indigenous village with my own people, and it’s extremely gratifying to help them in this way,” she said.
Ms Karajá believes that being indigenous eases communication and cultural differences. HIV and syphilis prevalence remains low among indigenous peoples in Brazil, but she fears that growing interaction with nearby cities will change that.
Established in 2010, the indigenous health services deliver services to every indigenous community, regardless of their remoteness. An 800-strong team of doctors, nurses, health-care technicians, psychologists, advisers and indigenous health workers work tirelessly, covering huge distances. They carry out tests for HIV, syphilis and other sexually transmitted infections. According to Ms Karajá, indigenous communities welcome them.
“Testing always follows a series of talks and workshops in villages about prevention of HIV and other sexually transmitted infections, and so the whole process flows naturally,” she said. If anyone tests positive for HIV, immediate counselling is available. Importantly, in the scope of this unique system, all HIV response efforts incorporate cultural beliefs.
Over a decade ago, a groundbreaking project pioneered by Adele Benzaken, at the time a researcher at Fundação Alfredo da Matta in Manaus, received funding from the Bill & Melinda Gates Foundation to test more than 46 000 indigenous peoples within their own communities. Activities focused notably in Amazonas and Roraima, remote forested states that are home to more than half of the indigenous peoples in Brazil. Stopping gender-based violence and keeping children from being born with congenital syphilis and HIV were among their priorities.
“Before the project, this indigenous population had very little access to any kind of diagnosis, treatment and prevention,” remembers Ms Benzaken, who today runs the national STI, AIDS and Viral Hepatitis Department of the Ministry of Health in Brazil. “They were vulnerable and didn’t have access to programmes.”
In 2012, rapid testing became a public policy for Brazil’s indigenous and general population. In five years, rapid HIV test distribution to the 34 operating indigenous health districts almost tripled to 152 000 in 2017; syphilis rapid test distribution more than doubled to more than 65 000 in the same year.
By boat, road and foot, health workers travel across the vast territories to test, raise awareness and discuss preventive methods, such as condoms.
Brazil is home to almost 900 000 indigenous peoples, with indigenous lands representing more than 12% of the country. Altogether, the country has 305 ethnicities speaking 274 different languages. The largest ethic group among them are the Tikuna.
Vinicios Ancelmo Lizardo—or Pureenco, in his original Avaí indigenous name—works as a health worker mainly in the Amazon region. “To help my people, I have to help them understand what health really means to them,” he said. Before explaining HIV prevention to a group of Tikuna in their own language, he speaks to them about love, sex and freedom, and he makes them laugh by teaching them—with the help of a lifelike dildo—how a male condom should be used.
Mr Lizardo admits that breaking cultural barriers and building bridges between science and tradition is challenging. But he knows that as most indigenous communities can no longer stay isolated, they cannot be left behind.
Region/country
Related

Feature Story
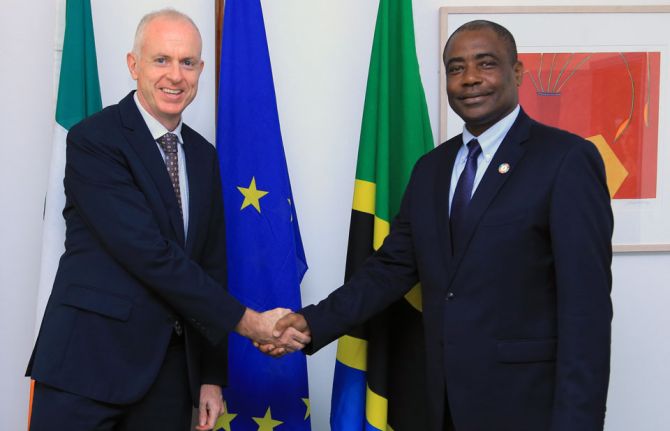
Ireland to support HIV services for the most vulnerable in the United Republic of Tanzania
14 December 2018
14 December 2018 14 December 2018Ireland has pledged €400 000 to UNAIDS for a project to provide HIV services for the most vulnerable populations in the United Republic of Tanzania, with the first tranche, €200 000, already received.
“Through our development programmes, Ireland supports the most marginalised in society to access key services so that they can live with dignity. Ireland is pleased to collaborate with UNAIDS to improve the plight of populations that are in most need of timely HIV services,” said the Irish Ambassador to the United Republic of Tanzania, Paul Sherlock.
UNAIDS will work in close collaboration with the Ministry of Health, the Benjamin Mkapa Foundation and civil society organizations to address issues that hinder the most vulnerable populations from accessing HIV prevention, treatment and care in a timely manner. Support that UNAIDS will provide includes convening stakeholders, providing technical leadership and strategic guidance and ensuring participation and representation.
Stigma and discrimination, inequality and violence against women and girls and criminal and punitive laws that affect vulnerable populations remain among the major barriers to an effective response to HIV in the country.
The 18-month project will help its beneficiaries with legal literary skills, raise awareness on the right to health and address HIV-related stigma and discrimination.
Ireland is a long-standing partner of UNAIDS, providing US$ 2.56 million in core funding to UNAIDS in 2018.
“UNAIDS and Ireland share a goal of ensuring that the AIDS response leaves no one behind. The funding from Ireland offers us a timely opportunity to give the most vulnerable populations in the United Republic of Tanzania a chance to live in dignity and good health,” said Leopold Zekeng, UNAIDS Country Director, United Republic of Tanzania.
Region/country




Feature Story
First Lady of Botswana champions revitalization of HIV prevention among adolescent girls and young women
27 December 2018
27 December 2018 27 December 2018While Botswana has made excellent progress in achieving the UNAIDS 90–90–90 treatment targets, evidence shows it has experienced a 4% increase in new HIV infections from 2010 to 2017, from 13 000 to 14 000. This is against the backdrop of a massive 30% decrease in new HIV infections across the eastern and southern African region.
Adolescent girls and young women are particularly at risk of HIV infection, as well as unintended pregnancy and sexual and gender-based violence. In 2017 there were 1 500 new HIV infections among adolescent girls between the ages of 10 and 19 years, compared to fewer than 500 new infections among adolescent boys the same age.
As a result, Neo Masisi, the First Lady of Botswana, uses her voice to advocate for better health outcomes for adolescent girls and young women. In an effort to drive high-impact, age-appropriate and gender-sensitive interventions, she holds dialogues with adolescent girls and young women about their experiences.
On 9 December 2018, she hosted a post-World AIDS Day event attended by 100 adolescent girls and young women, to bring to light to issues they face on a daily basis—unintended pregnancy, gender-based violence, access to sexual and reproductive health rights and how these intersect with HIV. “I am concerned about how young people have not known a life without HIV and hence they are more vulnerable to social ills,” said Mrs Masisi.
During the dialogue, Richard Matlhare, a representative from the National AIDS Coordinating Agency, emphasised that “the five-year Botswana National Strategic Framework on HIV/AIDS provides a paradigm shift, which is a sector-specific strategy explicitly focusing on adolescent girls and young women and their male partners.”
Participants at the dialogue also previewed the Pan-African movie Faces, directed by Joseph Adesunloye and starring South African actress, Terry Pheto, who plays the character of Aisha, a woman who has to deal with HIV infection and gender-based violence.
Ms Pheto, who attended the dialogue, spoke about her role as an actress and influencer and how she aims “not simply to entertain, but also educate, adolescent girls and young women and men on HIV and gender-based violence.” She added that projects such as these are “very close to my home and heart.”
Region/country

Feature Story
The need to scale up HIV programmes for key populations in western and central Africa
12 December 2018
12 December 2018 12 December 2018Key populations—gay men and other men who have sex with men, sex workers, transgender people, people who inject drugs, prisoners and other incarcerated people and migrants—and their sexual partners account for 40% of new HIV infections in western and central Africa.
However, key populations still have insufficient access to HIV prevention, treatment and care services. Fragile health systems, stigma and discrimination, sexual and gender-based violence and lack of supportive policies are some of the barriers that key populations face.
While high-quality programmes for key populations do exist in western and central Africa, there are limited opportunities to learn from each other and to strengthen South–South capacity. Monitoring of commitments made by all stakeholders, including governments, is also an issue. Three regional meetings took place in November to address those shortcomings.
The West Africa Health Organisation (WAHO), the United Nations Development Programme and ENDA Santé, a civil society organization, in collaboration with UNAIDS, met in Dakar, Senegal. The meeting brought together representatives of national AIDS commissions or programmes from 14 Economic Community of West African States (ECOWAS) countries and members of the Africa key populations expert group to chart the process for the development of a regional strategy on HIV/tuberculosis and sexual and reproductive health and rights for key populations, scheduled to be finalized in early 2020.
In 2015, under the leadership of WAHO, and in collaboration with UNAIDS and USAID, ministers of health, heads of national AIDS commissions, public prosecutors and inspectors general of police of ECOWAS Member States signed the Dakar Declaration on Factoring Key Populations in the Response to HIV and AIDS in ECOWAS Member States. The declaration aims to better take into account key populations in the response to HIV in the ECOWAS region in core areas, including strengthening of strategic information, health systems and community services and addressing stigma and discrimination.
In November, WAHO, UNAIDS and USAID commissioned a review of the progress made against the declaration and organized a regional progress review workshop attended by country representatives of 13 countries. The declaration has created a significant momentum, coupled with a number of achievements, innovations and good practices at the country level.
Ending AIDS in West Africa, a five-year cooperative agreement funded by USAID and led by FHI 360 and its core partners, Johns Hopkins University and ENDA Santé, facilitated the fourth key population regional meeting in western Africa, in partnership with the Government of Togo and partners.
The meeting was a key opportunity to bring together members of key populations, government officials, donors, academics and representatives of implementing partners and United Nations agencies to share lessons learned and promising practices from implementation, relevant and novel research and programmatic data, and to build networks and platforms for technical exchange. Country delegates also formulated country action plans to improve the quality, efficiency and scale of HIV-related programmes for key populations.
“The more the response to HIV is multisectoral, multidisciplinary and inclusive, the more impactful results we will have,” said Vincent Palokinam Pitche, Coordinator of the Permanent Secretary of the National AIDS Commission in Togo.
“There is a need to support the collection and analysis of strategic information to guide efforts to facilitate access by key populations to prevention, care and treatment services, to intensify services that are evidence-informed and rights-based and to invest in programmes for an enabling legal and social environment,” said Christian Mouala, UNAIDS Country Director for Togo.







Feature Story
Launch of a global partnership to eliminate HIV-related stigma and discrimination
10 December 2018
10 December 2018 10 December 2018Despite the existence of human rights obligations and policy commitments, HIV-related stigma and discrimination continues to be widespread around the world and in all sectors of society.
Following a call from civil society in 2017 to accelerate and scale up action to address stigma and discrimination, UNAIDS, UN Women, the United Nations Development Programme and the Global Network of People Living with HIV (GNP+) agreed to co-convene the Global Partnership to Eliminate All Forms of HIV-Related Stigma and Discrimination.
The global partnership was launched on 10 December on the 70th anniversary of the adoption of the Universal Declaration of Human Rights, during an event in Geneva, Switzerland. The panel of people speaking at the event included Phanpob Plangprayoon, the Deputy Permanent Representative of Thailand to the United Nations Office and other International Organizations in Geneva, Dan Namarika, the Secretary for Health of Malawi, Raquel Duarte, the Deputy Minister of Health of Portugal, and Simran Shaikh, a community representative to the UNAIDS Programme Coordinating Board (PCB).
The panellists presented programmes that have proved to be effective in reducing HIV-related stigma and discrimination in the areas in which the global partnership will focus—health care, schools, the workplace, the family, justice systems and emergency and humanitarian settings.
“This partnership aims to translate Member States’ commitments into well-resourced programmes that are proved to work and that can result in the enjoyment of HIV-related rights for all,” said Michel Sidibé, Executive Director of UNAIDS.
“The Global Network of People Living with HIV is pleased to be a co-convenor of this critical and ground-breaking global partnership that seeks to transform our communities’ best strategies for addressing and measuring HIV-related stigma and discrimination into actionable and accountable global targets and goals,” said Javier Hourcade Bellocq, GNP+ Board Chair.
People living with HIV, adolescents, young people and key populations experience discrimination, including discrimination based on their gender and gender identity, race, ethnicity, age, drug use, sexual orientation and migration status. These added layers of stigma and discrimination increase their vulnerability to HIV and undermine their rights, including the right to health, work and education.
At the end of the event, the UNAIDS PCB nongovernmental organization delegation called on Cosponsors, Member States, civil society, key populations, communities and partners to join the global partnership and lead and support concrete country actions and investments to end HIV-related stigma and discrimination.





Feature Story
Rwanda’s leadership provides model for advancing global agenda towards ending AIDS
10 December 2018
10 December 2018 10 December 2018Rwanda is a critical ally in the global AIDS response. Through political commitment from its leadership, the country has convinced its peers to drive the necessary change that has helped to ensure that the AIDS response delivers bold results for Africa and beyond.
In 2011, Paul Kagame, President of Rwanda, was the first African leader to convene a meeting at the United Nations General Assembly about the future of the AIDS response and the establishment of a sustainable road map for health and development.
AIDS Watch Africa was re-established as an outcome of that meeting, providing a platform for African heads of state to meet under African Union leadership to monitor progress against the targets for HIV, tuberculosis and malaria, ensuring African ownership and leadership of the African health response.
The country has made steady progress in its response to HIV. New HIV infections in Rwanda dropped by 20% between 2010 and 2017—from 9300 to 7400. AIDS-related deaths almost halved in the same time period, from 6000 to 3100. This is due to a robust HIV treatment programme, where 83% of all people living with HIV were on HIV treatment in 2017.
In 2017, 92% of pregnant women living with HIV accessed treatment to prevent of mother-to-child transmission of HIV, which translated into 1900 new HIV infections being averted.
With this history in mind, on 7 December, Michel Sidibé, Executive Director of UNAIDS, visited Kigali, Rwanda, to demonstrate solidarity with the Government of Rwanda and amplify the leadership role it has played towards ending AIDS as a public health threat by 2030.
In a special ceremony, Mr Sidibé appointed Jeannette Kagame, the First Lady of Rwanda, as UNAIDS Special Ambassador for Adolescent Health and Well-Being. Mr Sidibé commended her for being a champion for the empowerment of women and girls in Rwanda and Africa and for her leadership in girls’ education and promoting young people’s sexual and reproductive health and rights.
“Jeannette Kagame, you have been by UNAIDS’ side since the worst days of the epidemic. It was a time of great sadness and despair. But with your help we discovered hope. It is with the utmost respect and gratitude that I say thank you for everything you have done and everything you continue to do,” said Mr Sidibé.
“We cannot sit back with the satisfaction that the worst is behind us. As the face of HIV continues to change, we must remain vigilant, in order to respond to emerging challenges in a timely manner. We must also be deliberate in strengthening our defence against HIV and equip all men, women and children with the resources to live safe and healthy lives,” said Ms Kagame
Mr Sidibé also met with Mr Kagame, the President of Rwanda and the current Chair of the African Union. They discussed health financing and the overall sustainability of the AIDS response across the African continent. In a meeting with Richard Sezibera, Minister of Foreign Affairs and Cooperation, Mr Sidibé raised the need for revitalized global health diplomacy to keep health high on the international agenda.
















