Feature Story
Civil society cooperation network for the Americas and the Caribbean launched
02 November 2018
02 November 2018 02 November 2018A new regional civil society cooperation network for the Americas and the Caribbean to support nongovernmental organizations working to end AIDS was launched on 30 October in Quito, Ecuador. Launched by Coalition PLUS, the initiative will support coordination and capacity-building among community organizations involved in the AIDS responses of North, Central and South America and the Caribbean.
“Although we have HIV services available, people do not have access because they are criminalized and stigmatized. The community movement is helping us to end the conspiracy of silence about discrimination. We need civil society to increase efforts to achieve the progressive policies that will clear the way for us to end AIDS,” said Michel Sidibé, UNAIDS Executive Director.
Since 2014, Coalition PLUS—an international alliance of more than 100 nongovernmental organizations contributing to the AIDS response—has been building and strengthening mechanisms for regional collaboration. Such networks already exist in western Africa, central Africa, the Middle East and North Africa, the Indian Ocean and Europe.
The President of Coalition PLUS, Hakima Himmich, said that the network will increase access by organizations to new resources and approaches relevant to their local contexts. She noted that it was especially important to strengthen civil society’s capacity around addressing the needs of the most vulnerable.
“We have huge challenges around stigma and discrimination against entire populations. In order to achieve epidemic control, we must also address human rights,” said Ms Himmich.
UNAIDS data show that in 2017 key populations and their sexual partners accounted for three quarters of new HIV infections in Latin America and two thirds of new infections in the Caribbean. Gay men and other men who have sex with men and transgender women are disproportionately affected, with a few countries reporting HIV rates of above 15% among those communities.
The activities of the network in the region will be coordinated by the Kimirina Corporation, a Ecuadorian organization focused on people-centred combination prevention and advocacy. Amira Herdoiza, Director of the Kimirina Corporation, explained that the platform will place strong emphasis on coordinated research, skills-building and advocacy, particularly around issues affecting young people and key populations.
“We need more multicountry research to show the nuances of our epidemics,” Ms Herdoiza said. “Through this network our organizations’ capacities to share and analyse data will be strengthened. We will also focus on sharing experiences and planning joint programmes.”
At present, there are three other members of the regional network: the Coalition of Quebec Community Organizations against AIDS in Canada; AIDES in the French Caribbean; and the Institute for Human Development in the Plurinational State of Bolivia. Other regional organizations are invited to be part of the initiative.
Region/country
Related


Feature Story
New data dashboard launched in the Asia and the Pacific region
02 November 2018
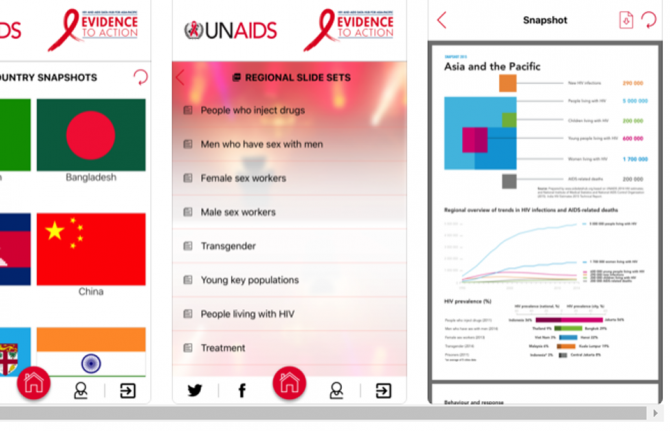
02 November 2018 02 November 2018A new data dashboard to enhance the HIV strategic information products that were already available on the AIDS Data Hub for the Asia and the Pacific region was launched on 30 October.
Developed by UNAIDS, the platform allows users to visualize data and indicators related to HIV epidemiology and the AIDS response in the region through customizable maps, graphs, tables and fact sheets by indicator, country and key population. It also facilitates integrated analysis and gives access to granular data. The data dashboard is a one-stop shop that offers HIV-related strategic information, data analysis products and reference documents.
“With concrete targets to be met on the way to end the AIDS epidemic by 2030, it is vital to have the right data tracking whether the Asia and the Pacific region is on course to meet the commitments made in the 2016 United Nations Political Declaration on Ending AIDS. Data show us how far we have come and how far we have to go,” said Eamonn Murphy, Director of the UNAIDS Regional Support Team for Asia and the Pacific.
Accurate and credible data on the HIV epidemic are the cornerstone of the AIDS response. Over the years, a detailed understanding of the HIV epidemic has been built up through the collection, analysis and dissemination of data, helping programmes to reach the right people in the right place and at the right time. Having high-quality data on the AIDS response coupled with cutting-edge analysis has been critical for countries to track their progress towards ending the AIDS epidemic.
UNAIDS and the Data Hub team work with all the countries in the region to collect and analyse data on their AIDS responses and to help build their capacity to generate and use strategic information. In the region, no major report, speech or policy initiative on HIV is launched or made without referring to data collected and released by UNAIDS.
The Data Hub team works closely with civil society, particularly on strengthening the capacity of young community members on data literacy and the interpretation and use of data. “Research and data, coupled with the lived experience of our community, provide the evidence we need for an effective response to HIV. The AIDS Data Hub is an essential tool for helping community-based HIV workers across the Asia–Pacific region access relevant research and data to amplify their advocacy for better services, more funding and the scaling up of programming,” said Midnight Poonkasetwattana, the Executive Director of APCOM.
Asia Pacific AIDS Data Hub
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa


Feature Story
HIVR4P 2018 highlights new possibilities for HIV prevention
31 October 2018
31 October 2018 31 October 2018The possibilities for new and improved HIV prevention options were showcased at the recent HIV Research for Prevention (HIVR4P) conference, although the participants heard that many new tools are still several years from being ready for implementation.
The importance of pre-exposure prophylaxis (PrEP), including PrEP delivered by a vaginal ring and long-acting PrEP, including injectable PrEP, was featured in many presentations. Vaginal ring PrEP offers better female-controlled prevention options that can protect women without their partner’s knowledge, while injectable PrEP would mean that daily pill-taking and the risk of forgetting to take the pill would be history. Both vaginal ring PrEP and long-acting PrEP are still some way from being available, however, with the vaginal ring currently being reviewed for regulatory approval by the European Medicines Agency and trials for long-acting PrEP not due to deliver results until 2021 or later.
If antibodies and engineered molecules that mimic them can be shown to prevent HIV infection, the way to six-monthly injections for either prevention or treatment could be opened up, along with the possibility of a vaccine that made people develop their own similar antibodies. The participants heard that much progress had been made in discovering and developing such antibodies. The first proof of principle trials showing their effectiveness will report their results in 2020.
“Science has delivered us extraordinary advances in technologies for the diagnosis, treatment and monitoring of HIV infection. There is now real excitement that over the next years it will also lead to effective affordable prevention tools,” said Peter Godfrey-Faussett, Science Adviser, UNAIDS.
The participants heard that there are high levels of sexually transmitted infections (STIs) among the populations at higher risk of HIV and that, as we have known for decades, STIs lead to increased HIV acquisition. The rates of the major treatable bacterial STIs have been rising steadily and are at alarming levels among gay men and other men who have sex with men and young people in eastern and southern Africa, in part due to declining condom usage. The high rates of the major treatable STIs have become particularly evident with the advent of increased screening accompanying the roll-out of PrEP.
Many STIs have no symptoms and can only be diagnosed with modern diagnostic tests—these are simple, but still far too expensive for the countries that need them the most. Along with geography and age group, STIs are among the strongest indicator of risk of HIV. An integrated STI and HIV prevention approach could offer PrEP to people who are HIV-negative but have an STI and live in an area where HIV is prevalent.
New prevention technologies are likely to be relatively expensive and hence will need to be focused on populations at higher risk in order to be affordable and cost-effective. Mathematical modelling shows that these new HIV prevention technologies may have only a limited impact on new HIV infections in eastern and southern Africa. For example, modelling of the impact of the dapivirine ring—a vaginal ring with a slow release of an antiretroviral medicine that protects against HIV infection—shows that only 1.5–2.5% of HIV infections would be averted over the next 18 years in Kenya, Uganda, Zimbabwe and South Africa. With the cost of averting one HIV infection through the use of the dapivirine ring varying from US$ 10 000 to US$ 100 000, many of the participants argued for integrating and combining both HIV treatment and prevention, and the responses to HIV and other diseases, for maximum effect.
The biennial HIVR4P conference was held in Madrid, Spain, from 21 to 25 October.




Feature Story
Training the next generation of Russian doctors on HIV-related stigma and discrimination
30 October 2018
30 October 2018 30 October 2018Stigma and discrimination among health-care workers is among the most severe barriers that people living with HIV experience in accessing life-saving health services. In order to encourage a new generation of health-care workers in the Russian Federation to provide medical services in a non-stigmatizing and discrimination-free setting, 20 medical students from across the country are participating in a new week-long course at the Vera HIV Medical School.
“Medical students often only hear second-hand stories about how to treat or care for people living with HIV. But if they receive the right training and practical support, they can be a bridge between people at risk of HIV and access to life-saving services,” said Anton Yeremin, the course’s coordinator, who is also an infectious diseases doctor who specializes in HIV treatment and care. “If doctors unknowingly promote stigma or explicitly discriminate against people living with HIV, or people at risk of HIV, it can result in patients being denied access to treatment, or even avoiding contact with medical services," he added.
The course is designed to complement what students learn at university. “We encourage future doctors to develop skills specific to the HIV context, such as relating to patients and understanding some of the social and legal aspects of their diagnosis,” said Mr Yeremin. The course consists of lectures and workshops on non-discriminatory approaches to people living with HIV and meeting people living with HIV, doctors, lawyers, psychologists, HIV activists and representatives of nongovernmental organizations to hear their stories.
According to Dmitry Petrov, a peer counsellor at the Svetlana Izambayeva Charitable Foundation, his clients are often denied admission to hospital. “An ambulance will arrive and the ambulance crew will say we can drive him to a hospital, but they won't admit him,” he said. Not long ago, he was helping a client to be admitted to a hospital; two official referrals from the local AIDS centre made no difference, and the woman was denied admission. Only after formal complaints filed by the patient’s family to the local government did the client get admitted. When asked about the most recent time a client was refused hospital admission, Mr Petrov answered “Yesterday,” without hesitation.
The stories shared by the Svetlana Izambayeva Charitable Foundation’s staff are consistent with the findings published in a recent Human Rights Watch report, which notes that people living with HIV regularly face stigma and discrimination from health-care workers. The situation is said to be worse outside of the major cities.
The course was initiated and organized by the National Union of Medical Students and was featured on a crowdfunding platform called No One Left Behind, a joint project of the Russian AIDS Center Foundation and UNAIDS.
Vera Brezhnevа, UNAIDS Goodwill Ambassador for Eastern Europe and Central Asia, has sponsored the course. “Every doctor must expect to see a person living with HIV at some point. We want medical students to understand that people living with HIV are a large and diverse group of people and their diagnosis is not a reason to hold negative attitudes towards them,” said Ms Brezhnevа. "I hope these first graduates of the Vera HIV Medical School will be the beginning of the end of HIV-related discrimination in health-care settings,” she added.
No One Left Behind
Region/country
Related

Feature Story
Global HIV prevention targets at risk
29 October 2018
29 October 2018 29 October 2018As the world grapples with how to speed up reductions in new HIV infections, great optimism is coming from the world of HIV prevention research with a slate of efficacy trials across the prevention pipeline. Major HIV vaccine and antibody efficacy trials are under way, as is critical follow-on research for proven antiretroviral-based prevention options.
However, a new report by the Resource Tracking for HIV Prevention R&D Working Group shows that rather than bolstering the new research by increasing investments into these exciting new advances, resources for HIV prevention research and development are actually slowing down.
In fact, in 2017, HIV research funding declined for the fifth consecutive year, falling to its lowest level in more than a decade. In 2017, funding for HIV prevention research and development decreased by 3.5% (US$ 40 million) from the previous year, falling to US$ 1.1 billion.
“Make no mistake, we are in a prevention crisis and we cannot afford a further funding crisis,” said Mitchell Warren, AVAC Executive Director. “It is unacceptable that donor funding for HIV prevention research continues to fall year after year even as research is moving new options closer to reality. We need continued and sustained investment to keep HIV prevention research on track to provide the new tools that will move the world closer to ending AIDS as a public health threat.”
The report warns that meeting the UNAIDS HIV prevention Fast-Track target of less than 500 000 new infections by 2020 (new HIV infections were at 1.8 million in 2017) will not only require the expansion of existing options such as voluntary medical male circumcision and pre-exposure prophylaxis, but also the development of innovative new products, including long-acting antiretroviral-based prevention options and a vaccine.
Indeed, sustained funding will be critical to keep the full gamut of HIV prevention research moving forward in a timely manner, as even small declines in funding could delay or sideline promising new HIV prevention options that are needed to end the AIDS epidemic.
“With 5000 people becoming infected with HIV every day, it is critical that we both scale up the effective HIV prevention programmes we currently have and invest in new technologies and solutions so that they can become a reality for the populations most affected by HIV,” said Tim Martineau, UNAIDS Deputy Executive Director, a.i. “Doing both will avert new infections, save lives and reduce the rising costs of life-long antiretroviral treatment.”
The Government of the United States of America continues to be the major funder of HIV prevention research, contributing almost three quarters of overall funding in 2017. However, this was also a decrease of almost 6%, bringing funding from the United States to a five year low of US$ 830 million. The report highlights that the uncertainty around continued political will to fund the AIDS response is a serious concern.
This week, researchers, implementers, advocates and funders are gathering at the HIV Research for Prevention (HIVR4P 2018) conference in Madrid, Spain, to review progress in HIV prevention research. There is much to be optimistic about in HIV science and in the accumulated knowledge of how to end the epidemic; however, the sobering changes in the funding and policy environments are raising some serious concerns about the future of the response to HIV and the world’s ability to respond to the continued challenges that HIV presents.
The report and infographics on prevention research investment are online at www.hivresourcetracking.org and on social media with #HIVPxinvestment.
Since 2000, the Resource Tracking for HIV Prevention R&D Working Group (formerly the HIV Vaccines & Microbicides Resource Tracking Working Group) has employed a comprehensive methodology to track trends in research and development investments and expenditures for biomedical HIV prevention options. AVAC leads the secretariat of the working group, which also includes the International AIDS Vaccine Initiative and UNAIDS.
Report and infographics on prevention research investment


Feature Story
Botswana’s First Lady visits UNAIDS to drive change for young women
24 October 2018
24 October 2018 24 October 2018The First Lady of Botswana, Neo Masisi, visited UNAIDS headquarters in Geneva, Switzerland, on 24 October to discuss improving health outcomes for young people, especially adolescent girls.
The First Lady met the Executive Director of UNAIDS, Michel Sidibé, and UNAIDS staff members.
“We can work jointly to address issues affecting 8-18-year-olds to ensure that the future generation that will lead and build Botswana is healthy, HIV-free and is equipped with life skills,” said Ms Masisi.
Botswana has made important gains towards ending the AIDS epidemic, but action is needed to curb the recent rise in new HIV infections, particularly among young people—a total of 14 000 people became newly infected with HIV in 2017. Women and girls are particularly vulnerable: 67% of women experience gender-based violence and teenage pregnancy stands at 9.7%.
Ms Masisi has been advocating for the empowerment of adolescent girls and young women to reduce their vulnerability. She listed social protection grants, economic programmes and promoting sexual and reproductive health as vital so that women live healthy and fulfilling lives.
“You are in a strategic position to be a champion and driver of change for young women,” said Mr Sidibé. “UNAIDS is committed to support you and Botswana.”
Related

Feature Story
Young people have a say in Fiji
19 October 2018
19 October 2018 19 October 2018Twenty-four young people gathered in Suva, Fiji, to take stock of the country’s progress in meeting the commitments in the 2016 United Nations Political Declaration on Ending AIDS and to identify what puts young people at risk of HIV.
The participants recognized that Fiji has taken important steps to establish laws and policies that enhance young people’s access to sexual, reproductive and HIV services. However, they noted that there are many factors that jeopardize young people’s health, including stigma and discrimination, limited access to condoms and a lack of harm reduction programmes for young drug users.
“Many young people have basic knowledge about HIV, its transmission and prevention. Many of them are not aware that antiretroviral treatment exists. It is critical that young people have access to information which is detailed and are informed on where they can obtain it,” said Swastika Devi, from the Reproductive Family Health Association of Fiji.
Greater technical and financial support for participation by young people in community responses to HIV was identified as important. The consensus from the group was that capacity-building of youth leaders should be supported, including leaders from communities, key populations and people living with HIV, in order to enhance their engagement in advocacy and decision-making.
The participants also agreed to form a sexual and reproductive health and rights youth network, which will finalize an advocacy road map focusing on their priority issues, which are youth-friendly services at clinics, developing a standard package of youth-centred services and comprehensive sexuality education that goes beyond puberty. The network has established contact with the Ministry of Health and Medical Services and Fiji’s national steering committee for World AIDS Day to strengthen youth-focused activities for World AIDS Day.
“The #UPROOT consultation has given us the reality of how the commitments in the 2016 United Nations Political Declaration on Ending AIDS affect young people in Fiji,” said Renata Ram, UNAIDS Country Director for Fiji. “Young people continue to be left behind in the AIDS response, despite being the age group most affected by the epidemic. The future of the HIV epidemic in Fiji will be determined by how we package our services towards young people. Failing to do so will push us further from ending AIDS.”
The consultation was part of the #UPROOT youth-led political agenda, launched by the PACT, a global coalition supported by UNAIDS of more than 80 youth organizations and networks working on HIV to respond to the barriers that put young people at risk of HIV. Similar #UPROOT meetings have taken place in Panama, Cameroon and Ghana.
Related information
Region/country


Feature Story
Defending opioid substitution therapy services in Kazakhstan
19 October 2018
19 October 2018 19 October 2018To defend her access to life-saving opioid substitution therapy, Marzhan Zhunusova overcame her fear of flying and, for the first time, took a flight to Astana, the capital of Kazakhstan. She was visiting the city to take part in a country-wide mobilization of people accessing the country’s harm reduction pilot programme, with people from all over Kazakhstan publicly showing the importance of opioid substitution therapy.
After injecting drugs for more than 25 years, Ms Zhunusova had lost hope for a better life. “When I first heard about opioid substitution therapy, I thought that it may be the way out and that it could help me. Drugs, my HIV-positive status, I thought my life was over. I’m 45 years old and only now thanks to methadone have I started to live life fully.”
The campaigners marched in Astana on 27 June and were joined by activists from other groups, including people living with HIV and gay men and other men who have sex with men.
The people who mobilized for the event share similar backgrounds. Their use of drugs may have deprived them of their health and their dreams. Some do not have jobs or have served time in prison. Many are isolated from society and the majority are living with HIV.
Ibrahim Dolgiev tried drugs for the first time in the 1970s, when he was 22 years old. “After many years of trying to stop using drugs, for the past year I’ve been in the opioid substitution therapy programme. It has been a salvation for me. My life has changed dramatically for the better, and for the first time in many years I can get through the day without heroin,” he said.
The people taking part in the mobilization came together to express their hope that the opioid substitution therapy programme will remain and that it will be further expanded.
In partnership with international and national partners, UNAIDS provided the Government of Kazakhstan with evidence-informed arguments on the effectiveness of opioid substitution therapy in controlling the HIV epidemic among people who use drugs.
“Access to opioid substitution therapy is one of the main factors enhancing adherence to antiretroviral therapy among people who use drugs,” said Alexander Goliusov, the UNAIDS Country Coordinator in Kazakhstan.
“Over the past three years, people who use drugs in the opioid substitution therapy pilot project in Pavlodar demonstrated 100% adherence to antiretroviral therapy,” said Zhannat Musaevich Tentekpayev, Chief Doctor of the Pavlodar AIDS Centre.
Unfortunately, however, the future of the programme in Kazakhstan remains uncertain, and no one has been enrolled in the programme since December 2017.
At the end of June 2018, a government commission announced that the pilot programme would continue, but that it would not be expanded to other regions of the country. An investigation into the cost-effectiveness of the programme is under way and the results will be presented by November. The Kazakhstan Union of People Living with HIV has appealed to the President of Kazakhstan not to close down the programme, noting that support for effective national responses to HIV is critical to making progress towards the 90–90–90 targets.
"While the law enforcement agencies are deciding whether the opioid substitution therapy programme is appropriate or not, the number of people accessing the programme remains very limited. The programme has to be not only maintained, it must exit its pilot status and be available and accessible everywhere in Kazakhstan for people who inject drugs,” said Oksana Ibrahimova, the coordinator of the Kazakhstan Union of People Living with HIV.
Today, there are 13 opioid substitution therapy centres in Kazakhstan, in nine of the 16 regions of the country. Since the beginning of the programme in 2008, more than 1000 people have been enrolled. Currently, 322 people are enrolled in the programme, the majority of whom have stopped using drugs, become employed and are enjoying a family life.
Related information
Region/country
Related




Feature Story
Race to ensure that people living with HIV get treatment after Central Sulawesi earthquake
19 October 2018
19 October 2018 19 October 2018On 28 September, Central Sulawesi, Indonesia, was struck by a powerful earthquake and a subsequent tsunami. Thousands of people are known to have died and tens of thousands of people have been displaced. In the event of a major humanitarian disaster, the basic needs of people are always difficult to fulfil—this is especially true for people living with HIV in Central Sulawesi.
The hospitals in the town of Palu are heavily damaged but remain operational. There are still stocks of antiretroviral therapy in those hospitals, but there are concerns about how long those stocks will last. Before the disaster, according to government data, there were an estimated 1913 people living with HIV in Central Sulawesi, with 334 people, including three children, on antiretroviral therapy.
People in the region have been rallying as champions for people living with HIV. Yuli works for the Indonesia AIDS Coalition, a civil society organization monitoring support for antiretroviral therapy, in Makassar in South Sulawesi, Indonesia. On 2 October, while on her way to Donggala, a region affected by the earthquake, to check on her family, she heard from her employer about severe disruptions in the supply of antiretroviral medicines in Palu.
Yuli and her colleagues headed to Palu to provide help, contacting hospitals and other service providers to gather the remaining stocks of antiretroviral medicines to distribute to those in need. Her mission quickly became a commitment to support the HIV response in Palu, including helping in contact tracing and providing social support for people living with HIV in the region.
“The reason I’m still here more than two weeks after the disaster is because it is impossible to see the conditions and not lend a helping hand,” Yuli said, explaining that, in addition to antiretroviral medicine, people in Central Sulawesi need support for their basic needs and psychosocial support.
By 16 October, 92 out of the 344 people previously on antiretroviral therapy had accessed a one-month supply of antiretroviral medicines, either from Yuli and her team or directly from clinics.
“My main concern is that I want to make sure that even though the disaster happened, people living with HIV still get access to antiretroviral therapy and not stop their treatment,” Yuli said.
UNAIDS and partners in the region have joined together as the National Core Team for HIV Response in Humanitarian Settings. The team is actively working to support the HIV response in the affected areas, trying to find out the status of the people living with HIV yet to be found and ensuring the distribution of antiretroviral medicines to those who need them. A command post for HIV has been established in Palu, with a team monitoring the availability of antiretroviral medicines in the affected region.
“HIV is often overlooked in emergency situations. We must work hard to ensure that people living with HIV are not forgotten in times of need. We applaud the quick initiative and commitment of Yuli and her fellow outreach workers and will continue to provide them with support,” said Krittayawan Tina Boonto, UNAIDS Country Director for Indonesia.
The UNAIDS office in Indonesia has mobilized resources to fund six field visits by peer supporters for people living with HIV to Palu to provide immediate assistance. UNAIDS will also conduct a full needs assessment for HIV, tuberculosis and malaria in Central Sulawesi to develop funding requests for medium- and long-term assistance and will establish contingency plans for use in the event of future disasters in Indonesia.
Region/country


Feature Story
UNAIDS revises its policy on adoption, paternity and surrogacy leave
15 October 2018
15 October 2018 15 October 2018UNAIDS has revised its internal adoption and paternity leave policy and introduced new rules on surrogacy leave, marking an important step in ensuring a more inclusive working environment.
The revised policy includes the extension of adoption leave from eight to 16–18 weeks, depending on the number of children being adopted, the extension of paternity leave from four to 16 weeks and the introduction of 16 weeks of leave for a single birth by surrogacy and 18 weeks for multiple births by surrogacy.
The new policy is the result of concerted advocacy efforts by the UNAIDS Secretariat Staff Association (USSA), in collaboration with UNAIDS management, and is one of the commitments made in the recently launched UNAIDS Gender Action Plan 2018–2023.
“The revised policy will allow fathers to spend more time with their families at a critical stage in life,” said a staff member who will soon become a father. “Men can and have to play an important role in childcare and actively challenge gender norms that pass most responsibility for childcare onto women,” he said.
Adopting a more equitable policy framework that supports caregiving by both men and women can help in overturning perceptions that women of childbearing age are potentially too expensive or an absentee risk when compared with similarly qualified men.
“The UNAIDS Secretariat Staff Association welcomes this important milestone in our internal policy framework, which will not only bring direct benefits to staff who will become parents, but to all staff, as it challenges pervasive gender norms,” said Pauliina Nykanen-Rettaroli, USSA Chair.
The introduction of specific leave for births by surrogacy reflects UNAIDS’ commitment to diversity. “It doesn´t make a difference if you become a parent by natural birth, adoption or surrogacy; you still become a parent and should be entitled to the same benefits,” said a staff member. “This policy reflects the organization’s commitment to be as inclusive as possible and walk the talk of what it advocates for, which is dignity and respect for all,” she added.
“In our new Gender Action Plan, we committed to adopting a single parental leave policy and I am proud that UNAIDS has now delivered on this. All parents should be supported to spend time with their children. By supporting this, UNAIDS is contributing to shifting the burden of care and advancing gender equality,” said Gunilla Carlsson, UNAIDS Deputy Executive Director, Management and Governance.