


Feature Story
Forty years of campaigning for equal access to life-saving medicines
17 September 2021
17 September 2021 17 September 2021A look back at the early days of AIDS activism highlights stark parallels with the global response to COVID-19.
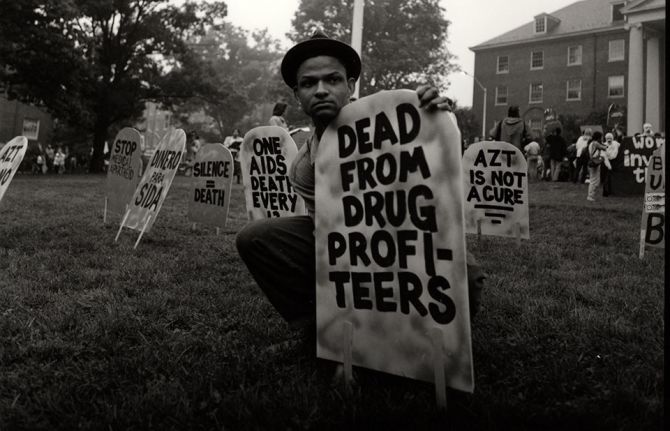
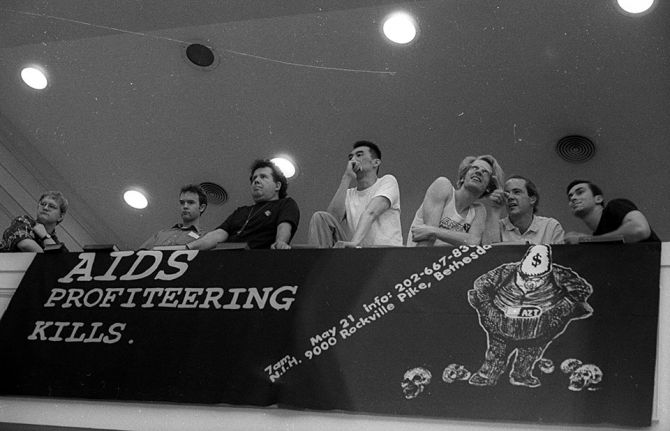
Previously unseen images from the early 1990s of AIDS activists campaigning for life-saving medicines show that, with slogans such as “Dead from drug profiteers” and “AIDS $ now”, the AIDS activists of yesterday mirror today’s activists in their demand for equal access to COVID-19 vaccines.
However, the photos also highlight how, 40 years after the discovery of the first AIDS cases, the world is repeating the same mistakes in its response to COVID-19, as inequalities continue to be the driving force of infections and deaths.
The photos, taken by French photographer Elizabeth Carecchio, show people marching for HIV treatment at a demonstration in May 1990 at the National Institutes of Health in Washington, DC, United States of America. They are a reminder of the central role played by activists over the years, including today as they continue to advocate for fairer access to treatment and vaccines. In short, they are campaigning for the world to put people before profits, a central call of the People’s Vaccine for COVID-19, which UNAIDS is proud to be part of.
Photos: Elizabeth Carecchio
Our work
Related


Feature Story
More than 140 former heads of state and Nobel laureates call on candidates for German chancellor to waive intellectual property rules for COVID vaccines
14 September 2021
14 September 2021 14 September 2021More than 140 former heads of state and government and Nobel laureates today called on the candidates to be the next German chancellor Annalena Baerbock, Olaf Scholz, and Armin Laschet to declare themselves in favour of waiving intellectual property rules for COVID 19 vaccines and transferring vaccine technologies, and “to make these the policies of any future coalition government”.
The signatories underlined that ending German opposition to waiving patents is vital to overcoming vaccine monopolies, transferring vaccine technology and scaling up vaccine manufacturing around the world to prevent millions more deaths from Covid-19.
Former world leaders including former President of France François Hollande, former Prime Minister of the United Kingdom Gordon Brown, former President of Colombia Juan Manuel Santos, former President of Malawi Joyce Banda and Nobel prize winners including Professor Joseph Stiglitz, Professor Francoise Barre-Sinoussi and Elfriede Jelinek express that they are “deeply concerned with Germany’s continued opposition to a temporary waiver of the World Trade Organization’s (WTO) intellectual property rules”, at a time in which “the artificial restriction on manufacturing and supply is leading to thousands of unnecessary deaths from COVID-19 each day”. Less than two per cent of adults are fully vaccinated in low-income countries compared to almost 50 per cent in high income countries.
Signatories urge the three candidates to support a wide and comprehensive waiver of the TRIPS intellectual property agreement on all COVID-19-related technologies at the WTO, and join over 100 countries including the United States and France in doing so. Despite that, Germany continues to oppose a waiver of the trade-related aspects of intellectual property (TRIPS) agreement for Covid-19 vaccines and treatments at the WTO. First proposed by India and South Africa in October 2020, a waiver is now supported by more than 100 nations, with France and the United States announcing their support earlier this year.
The letter emphasizes that “Having helped create the most successful vaccine technology against COVID-19, by overcoming pharmaceutical monopolies and insisting that the technology be shared, Germany has the ability to help end this pandemic”. In addition to supporting the waiver they call on the next Chancellor to ensure that German pharmaceutical companies openly and rapidly share life-saving mRNA vaccine technology with qualified producers around the world.
Helen Clark, former Prime Minister of New Zealand, said: “Germany’s support for a TRIPS waiver in the exceptional circumstances presented by COVID-19 would send a clear signal that all peoples should be able to benefit speedily from available vaccines and therapeutics. Widespread vaccination now and further scaling up of vaccine production will play a significant role in curbing the pandemic.”
Joseph Stiglitz, Nobel Economics Prize Laureate, said: “The new Chancellor of Germany will hold extraordinary power to turn the tide on this horrific pandemic and can be the world leader remembered for helping save millions of lives. Intellectual property rules are today locking out people across the world from the benefits of life-saving science - it is time for Germany to ensure the transfer of vaccine technologies and join the rest of the world in backing a temporary waiver at the World Trade Organization”.
As the Heads of State and Government and Nobel Laureates write to the candidates for Chancellors, activists around the world have organized protests to demand the German government to stop blocking efforts to vaccinate the world. Protests will take place from the city of Nairobi to the Sydney Opera House in Australia, from the Union Buildings in Pretoria to Brazil's famous Cristo Rei and the famous Golden Gate Bridge in San Francisco.
The letter, which was coordinated by the People’s Vaccine Alliance, a coalition of more than 70 organizations including Club de Madrid, Oxfam and UNAIDS, warned that extreme vaccine inequity is bound to last as long as there will be no remarkable increase in vaccine production. While high-income countries are now starting to offer their citizens booster shots, the global supply falls far short of the levels needed to provide global vaccination coverage.
Notes to editors
Read the full letter and list of signers.
The letter was coordinated by the People’s Vaccine Alliance, a coalition of more than 70 organizations including Club de Madrid, Physicians for Human Rights, Oxfam, UNAIDS, the Nizami Ganjavi International Center, Global Justice Now, the Yunus Centre and Avaaz, as well as Progressive International.
Our work
Related




Feature Story
UNDP and UNAIDS support more than 300 pregnant and breastfeeding women living with HIV in Abidjan
08 July 2021
08 July 2021 08 July 2021Like the rest of the world, COVID-19 has hit Côte d’Ivoire hard. As soon as the first cases of COVID-19 were confirmed in March 2020, a national response plan was developed by the government. Unfortunately, the restrictive measures to protect the population had an impact on the use of health services, including those related to HIV, threatening the fragile retention in care of people living with HIV. Pregnant and lactating women living with HIV and their children, one of the most vulnerable groups, have been particularly affected, and maintaining their access to services and care was essential to avoid undoing years of effort.
The United Nations Development Programme (UNDP) and UNAIDS joined forces to help retain 333 pregnant and lactating women living with HIV in antenatal, maternity and paediatric services in Abidjan. The project will provide, over nine months, 1000 food kits and 1000 hygiene kits to help beneficiaries with food assistance and help them protect themselves against COVID-19. A food kit contains 20 kg of rice, six litres of oil, 10 pieces of soap and four boxes of children’s flour, and a hygiene kit contains two bottles of hydroalcoholic gel, two bottles of liquid soap and 50 surgical masks. The project also aimed to ensure that the women have access to the comprehensive package of services developed under Côte d’Ivoire’s prevention of mother-to-child transmission of HIV (vertical transmission) programme, to ensure that all exposed children of the project’s beneficiaries are screened early and have access to appropriate care and to document and share good practices.
One of the beneficiaries, Ouattara Maimouna, who has been living with HIV for five years and is a breastfeeding mother of three children, said, “Doctor, this gift was incredibly important to us. It has helped us a lot! This stock of food helps me feed my family. I cannot thank you enough, because I ran out of ways to sustain the small business that used to support my family.”
“About 700 hygiene kits and 700 food kits have been distributed since the project started in December 2020. The United States President’s Emergency Plan for AIDS Relief’s (PEPFAR) implementing partners unanimously indicate that the kits have contributed to the loyalty of pregnant and breastfeeding women to prevention of vertical transmission of HIV and paediatric care services, as well as to self-support groups,” said Brigitte Quenum, the UNAIDS Country Director for Côte d’Ivoire.
At this stage of implementation, some lessons learned are already emerging. The project has been very well received by the beneficiaries because of their vulnerability, which has been aggravated by the COVID-19 crisis. The support has helped to increase their compliance with appointments at the various prenatal consultations, to improve the continuity of treatment and viral load testing for pregnant and breastfeeding women and to strengthen the link between women living with HIV and the staff providing both clinical and community care. The project also emphasizes the importance of taking into account the social component in the care of women in prevention of vertical transmission of HIV services.
The distribution of food and hygiene kits will continue until the end of 2021. Pregnant and breastfeeding women living with HIV have become more vulnerable in the midst of the response to COVID-19 and assistance strategies that respond to their specific sensitivities must be designed. “The mobilization of UNDP, UNAIDS, PEPFAR implementing partners and their nongovernmental organization partners has ensured a coalition of support for advocacy and the scaling up of outreach efforts to vulnerable populations,” added Ms Quenum. “While this one-time initiative is useful, efforts should be made to integrate other activities, such as nutrition promotion and the integration of a social component in the care of women living with HIV in vertical transmission services and other care sites.”
An HIV-sensitive and inclusive social protection assessment will start in the coming months in collaboration with the key ministries involved. Mobilization of funds for social aspects related to women living with HIV and advocacy for sustainable support measures will be required.
Region/country


Feature Story
Report shows big COVID-19-related HIV prevention programme service disruptions, but highlights that HIV service innovations and adaptations are possible
01 July 2021
01 July 2021 01 July 2021The COVID-19 pandemic is threatening decades of hard-won development and public health gains. UNAIDS is committed to playing a pivotal role in ensuring that people living with and affected by HIV have the information and support they need during the COVID-19 pandemic and is promoting the development and support measures needed to ensure that access to HIV prevention and treatment services continues uninterrupted.
Launched in 2017, the Global HIV Prevention Coalition aims to bring fresh momentum and clarity to HIV prevention programmes, focusing on 28 countries carrying the highest burden of the HIV epidemic. The Global HIV Prevention Coalition has published a new report, Preventing HIV infections at the time of a new pandemic: a synthesis report on programme disruptions and adaptations during the COVID-19 pandemic in 2020, which provides a synthesis of the status of HIV prevention programming during the COVID-19 pandemic, identifies critical vulnerabilities, risks and major service disruptions and documents responses in a range of settings. The report places a significant focus on gathering information on programme innovations at the community level.
“The COVID-19 pandemic risks reversing the hard-won gains made in HIV prevention, including the 23% reduction in new infections since 2010. And this is at a time when much more still needs to be done to drastically reduce new HIV infections. Gaps and threats to progress show great inequalities, and HIV prevention services and societal barriers for the people most left behind, such as key populations and adolescent girls and young women, have been disproportionately impacted by COVID-19,” said Shannon Hader, the UNAIDS Deputy Executive Director for Programmes.
Inevitably, significant disruptions on HIV prevention services have been observed, and supply chains for crucial HIV prevention commodities, including condoms, lubricants and antiretroviral and other medicines, have been stretched. The report reflects on the early dips observed in the monthly numbers of people served by critical HIV prevention programmes, including huge drops in the number of voluntary medical male circumcisions performed compared to previous corresponding months.
At the same time, while it has vividly exposed and widened inequalities and health inequities, COVID-19 has also shown how to make health systems and other public institutions fairer, more inclusive and better able to meet the challenges of ending the AIDS epidemic. Health-service providers and community organizations have responded to the crisis by changing how they provide HIV prevention services and minimizing disruptions of essential services.
The report highlights COVID-19 impact mitigation innovations and adaptations of HIV services, including multimonth dispensing of condoms, lubricants, needles, syringes and pre-exposure prophylaxis (PrEP), differentiated service delivery and self-testing approaches, alternative access points for prevention commodities such as condoms and PrEP, take-home dosages of opioid substitution therapy for people who inject drugs, the safe continuation of outreach services for key populations and adolescent girls and young women and virtual platforms for prevention interventions—and calls for their scale-up even beyond the COVID-19 pandemic. The report further highlights how the COVID-19 pandemic response has drawn from HIV experts and communities and has taken early decisive action to address critical vulnerabilities, maintain health services and build synergies between the colliding pandemics.
“In over 30 years of developing effective prevention approaches, we have gained substantial knowledge and experience that decision-makers and health programme implementers can use in low- and middle-income countries to make the best possible choices in preventing SARS-CoV-2,” said Dr Hader. “The most pressing needs we hear from communities are the protection of livelihoods: how do people eat, live, care for themselves and survive COVID-19. UNAIDS can help broker services for people,” she added.
The report will support all stakeholders in their preparation of Global Fund to Fight AIDS, Tuberculosis and Malaria COVID-19 Response Mechanism applications, ensuring that proposal writing teams identify key HIV prevention innovations and adaptations that could be supported and scaled-up to regain global HIV prevention momentum and mitigate the impact of the COVID-19 pandemic on HIV services.


Feature Story
Addressing the impact of the COVID-19 pandemic on the AIDS response
10 June 2021
10 June 2021 10 June 2021A panel that met on the sidelines of the United Nations High-Level Meeting on AIDS, Addressing the Impact of the COVID-19 Pandemic on the AIDS Response and Building Back Better for Pandemic Preparedness, examined how the responses to HIV and COVID-19 can contribute to building multisectoral preparedness and response systems through providing concrete examples of innovations and policy and structural changes introduced in the context of COVID-19.
The panellists, comprising leaders, experts and representatives of community organizations and networks of affected people, addressed how to improve pandemic preparedness and response, and health-care systems more broadly, in the pursuit of the Sustainable Development Goals.
The speakers shared ideas and recommendations to help mobilize political leadership, solidarity and support for ending AIDS by 2030 and for stronger pandemic preparedness for the future. They went on to look at how innovation and technology can address the bottlenecks to achieving Sustainable Development Goal 3 (good health and well-being) through digital health infrastructure and agile, differentiated delivery models. The panellists also addressed the importance of community-led responses in delivering health for all, and reflected on the importance of across- and within-country solidarity in ensuring equitable access to health and socioeconomic support.
Quotes
“HIV setbacks because of COVID-19 would not have happened with more effective protective policies and laws. National sovereignty should not be used against populations in need, but laws should be applied to protect communities.”
“Adaptable institutions like the United States President’s Emergency Plan for AIDS Relief can provide important foundations to protect against future shocks. Countries around the world have been investing in their health systems—looking to future pandemics, we need to focus on prevention as well as preparedness to respond.”
“We need to explore new institutional arrangements to encourage effective multilateralism. All countries need to respond more effectively to best practices, and, for example, learn from the impact of community engagement and leadership in HIV responses.”
“Men who have sex with men, sex workers, transgender people, people who inject drugs and prisoners are particularly vulnerable to HIV and frequently lack adequate access to HIV services. In the context of COVID-19, we must make an extra effort to ensure they access all of the HIV services they need.”
“Pandemic preparedness must be a priority for the African continent. Africa has the largest HIV burden in the world and the pandemic in Africa has disrupted essential services and these disruptions could indirectly kill more than COVID-19 itself.”
Our work
Related


Feature Story
What responses to HIV and COVID-19 in Asia and the Pacific led by civil society can teach us
11 June 2021
11 June 2021 11 June 2021COVID-19 continues to threaten the gains made in the HIV response and has brought inequalities to the forefront, but civil society and community-based organizations in Asia and the Pacific have been quick to respond to the pandemic. From the start, networks of people living with HIV and key populations responded to the global health crisis by coming up with innovative courses of action.
A side event organized on the margins of the United Nations High-Level Meeting on AIDS showcased best practices of community-led responses to COVID-19 and HIV prevention in Asia and the Pacific.
It was noted that, since the onset of the COVID-19 pandemic, key population networks have rapidly mobilized volunteers and partners to assist people affected by COVID-19, ensured the continuity of HIV services and found new ways to adapt to the new normal with online-based interventions.
For example, the Asia Pacific Network of Sex Workers responded to the pandemic by modifying its existing programmes to meet the urgent needs of the sex worker community, such as by reallocating funds to subsidize transport costs for sex workers living with HIV to ensure their access to HIV treatment services.
Other regional networks, such as the Asia Pacific Transgender Network, the Asia Pacific Network of People Living with HIV and Youth LEAD, established emergency relief funds to provide emergency food supplies, housing and rent, transport, protective gear, including personal protective equipment, masks, sanitizer and sanitary products for the most affected communities.
In several countries, community-led organizations of people who use drugs delivered door-to-door provisions of antiretroviral therapy and harm reduction services, including opioid substitution therapy and sterile needles and syringes. These experiences have been compiled by the Asia Pacific Network of People who Use Drugs in a best practice report to advocate for the full and equal participation of people who use drugs within the HIV response.
The panellists also heard about the Australian Federation of AIDS Organisations, which in its national and community-led responses has been supporting community-based HIV testing, working directly with clinics run by the community for the community. Also, APCOM, a regional network for gay men and other men who have sex with men based in Bangkok, Thailand, implemented a condom promotion campaign during the COVID-19 pandemic, known as #PartyPacks, where key populations can order online (for free) packages containing condoms, lubricant and information on harm reduction.
The speakers agreed that service delivery needs to be modernized, domestic investment should be increased and services led by key populations should be integrated into national health systems.
The panellists highlighted that dealing with the colliding pandemics of HIV and COVID-19 requires working in unison and solidarity.
Quotes
“While the journey has not been smooth, one of Australia’s key learnings is that the voices of the community are essential. Communities of people living with HIV and those populations at high risks and young people—communities who, if we are to really make a difference, must have a central role in sharing the view of those most affected by HIV with national governments.”
“Thailand’s effort on HIV/AIDS is one area where civil society plays a particularly vibrant role in our country. We recognized that the collaboration of different sectors, especially civil society and the network of people living with HIV, is one of the most important factors in Thailand’s success in controlling the spread of HIV and AIDS.”
“The valuable experiences of communities reflect their long-standing active participation in the response to the HIV epidemic. This is exhibited in the way they continue to innovate at the forefront of the response to HIV and, most recently, address the intersectionality that emerged out of having to respond to the impact of COVID-19 as well.”
“Key populations are widely recognized as the pioneers and leaders of the HIV response. Since the emergence of HIV, key populations have led the way in pioneering effective prevention responses, sharing their knowledge and skills with the community as well as providing essential care and support.”
“Community-led organizations are the most effective way to reach sex workers during emergencies as they are capable of providing therapy assessment, identifying priority areas and allocating the resources for various types of relief for sex workers. This is facilitated by an established peer-to-peer model that is led by the trust and knowledge of peer outreach programmes, which is also able to deliver emergency aid to the most in need.”
Our work
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa


Feature Story
Science, HIV and COVID-19—where are we headed?
08 June 2021
08 June 2021 08 June 2021A side event at the United Nations High-Level Meeting on AIDS, being held in New York and online from 8 to 10 June, has highlighted the science relevant to the new UNAIDS global strategy and targets and the changing scientific environment that will take the world to 2030, the Sustainable Development Goal target date for ending AIDS.
At the event, Science, HIV and COVID-19—Where are we Headed?, Jon Cohen, a leading science journalist, moderated a panel discussion that included Anthony Fauci, the Chief Medical Adviser to the President of the United States of America, Loyce Maturu, an activist working for Zvandiri in Zimbabwe, Soumya Swaminathan, the Chief Scientist at the World Health Organization, and other leading HIV scientists.
In the complexity and multidimensional nature of the global AIDS response, science has been a constant force, moulding and adapting how the world reacted. A similar role for science has been seen in the other ongoing pandemic—COVID-19. The side event was an opportunity to discuss the role of science and to review major and emerging scientific themes that will influence the trajectory of the HIV pandemic in the approach to 2030.
Mr Fauci emphasized the importance of long-term engagement and investment in surveillance and basic sciences to increase preparedness for future pandemics, noting that we must focus on building trust in science and explaining how knowledge evolves through the accumulation of reliable data that can alter clinical and public health guidance. The COVID-19 pandemic has taught us lessons in efficiency and in accelerating the translation of basic science into effective interventions, he said. However, we must address the challenges of access, intervention pricing and social biases that limit our global impact. He concluded that both the HIV pandemic and the COVID-19 pandemic have the power to strengthen the global community, and he committed the United States to being a global leader and reliable partner in those efforts.
Greg Millett celebrated the amazing fall in new HIV infections in several places, such as London, Denmark and Australia, where pre-exposure prophylaxis (PrEP) and effective testing and treatment is really working for gay men and other men who have sex with men. He highlighted the importance of recent scientific advances that have led to new technologies, such as HIV self-tests and new PrEP modalities.
A major theme was around equity. For both COVID-19 and HIV, the participants noted that we must ensure that all people in all countries reap the benefits of science. Commentators in the audience reiterated that this is even more important given the participation of so many people across so many countries as the altruistic participants in the research that has led to the exciting new tools for HIV prevention and vaccines for COVID-19. And Mr Millet pointed out that we are all interrelated and interconnected. HIV infections and other diseases are, of course, in no way limited to national boundaries.
Loyce Maturu reminded everyone that young people are central to the HIV response. Young people are often left behind and treated as end users of services that are not specifically designed to suit their lifestyles. She acknowledged that science was the reason that she was with us, healthy, beautiful and empowered after falling sick with HIV-related illnesses as a child and witnessing the death of both her mother and brother from HIV. Young people need to be central to science and brought to the tables that set the research priorities.
Quarraisha Abdool Karim, and others, exhorted political leaders not to “drop the ball” for HIV. We need to finish the job and not allow the huge challenges of dealing with it deflect us.
All the participants pushed for HIV programmes to be based firmly on scientific evidence, and Wafaa El Sadr noted that the evidence base comes not only from biomedical laboratories and large clinical trials, but also from implementation and the social sciences. The Co-Chairs of the upcoming International AIDS Society Science Conference, in July 2021, Adeeba Kamarulzaman and Hendrik Streeck, hoped that the high-level meeting would be a boost for stronger engagement with science—registrations for the conference are as high as ever, despite the COVID-19 restrictions. Mr Streeck called for a massive effort to bring thousands of HIV vaccine scientists together in one huge effort, similar to the collaboration around the Large Hadron Collider or even the Manhattan Project.
In an optimistic conclusion, Ms Swaminathan hoped that the proven success of the scientific collaboration that has produced multiple COVID-19 vaccines so quickly should be a stimulus for greater enthusiasm and investment in collaborations to end not just AIDS but also other major public health challenges, such as tuberculosis, malaria and noncommunicable diseases.
Quotes
“We must ensure that we reach all sectors of our local and global communities, in particular those that are sceptical, disadvantaged or historically exploited.”
“Please make sure that young people and adolescents are seen as decision-makers, and not just as end users. We need a bottom-up approach to ensure that research and science are driven by communities to deliver what everyone needs.”
Related


Feature Story
UNAIDS supports the Partnership for Accelerated COVID-19 Testing in Ghana
25 May 2021
25 May 2021 25 May 2021The UNAIDS Country Office for Ghana is supporting the Millennium Promise Alliance, the Network of People Living with HIV and the Young Health Advocates Ghana in a partnership to strengthen community engagement in the COVID-19 response.
Aimed at reducing the community spread of COVID-19 and minimizing its effects on reaching the national HIV targets, the Partnership for Accelerated COVID-19 Testing (PACT) in Ghana will encourage the adoption of COVID-19 preventive behaviours, such as physical distancing, wearing face coverings and hand hygiene, reduce COVID-19-related stigma, promote vaccine uptake and strengthen the capacities of communities.
The PACT initiative in Ghana targets the two regions with the heaviest COVID-19 burden: the Ashanti and Greater Accra regions. Launching the project, the Director-General of the Ghana Health Service, Patrick Aboagye, commended the initiative and highlighted the urgent need for an all-hands-on-deck approach to end the COVID-19 pandemic.
The UNAIDS Country Director for Ghana, Angela Trenton-Mbonde, emphasized the importance of galvanizing HIV civil society to strengthen community engagement in the fight against COVID-19. “PACT will generate evidence for advocacy from communities, including people living with HIV, women’s groups and other vulnerable populations, to identify and inform health authorities of any disruption of essential health services, particularly HIV-related services at the community level, and will mobilize for greater uptake of those services,” she said.
The PACT initiative, launched by the Africa Centres for Disease Control and Prevention in April 2020, aims to conduct 10 million COVID-19 tests on the African continent. PACT has three pillars: test, trace and treat, which cover the procurement and distribution of COVID-19 test kits, the deployment and training of one million community health-care workers to support contact tracing and monitoring, and COVID-19 sensitization measures.
Our work
Region/country
Related
 Impact of US funding cuts on HIV programmes in Ghana
Impact of US funding cuts on HIV programmes in Ghana

08 April 2025