


Feature Story
Global HIV Prevention Coalition accelerates action to reduce new HIV infections
23 May 2018
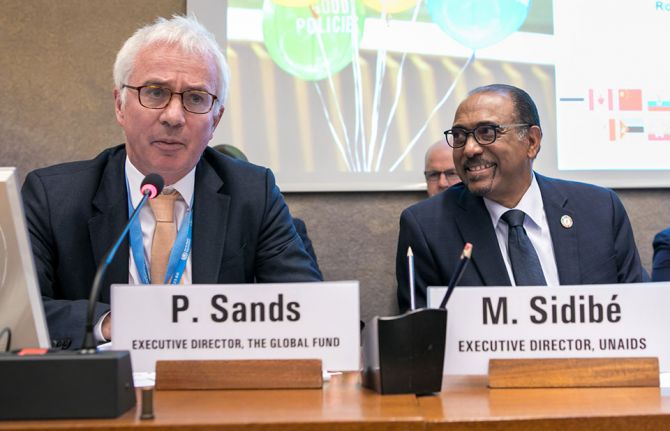
23 May 2018 23 May 2018The Global HIV Prevention Coalition has launched its first progress report.
Taking stock of the progress made in strengthening political commitment for HIV prevention and reducing new HIV infections, the report shows that significant progress has been made since the launch of the Global HIV Prevention Coalition six months ago. National prevention coalitions have been established to accelerate and better coordinate responses, new and ambitious prevention programme targets have been set in many countries and HIV strategies that focus on prevention have been launched.
“There are many promising country examples across the coalition we can learn from,” said Sicily Kariuki, the Minister of Health of Kenya.
Good programme examples highlighted at the event include strong condom programmes in some southern African countries and high voluntary medical male circumcision coverage in several eastern African countries. Strong programmes for key populations, including in India and Ukraine, and pre-exposure prophylaxis being rapidly introduced and expanded in Brazil and Mexico, as well as in South Africa and Kenya, were also noted.
However, the progress report also shows that much still needs to be done. Policies on age of consent continue to represent major barriers to adolescents accessing services. Punitive laws and law enforcement practices hinder access by key populations.
“Every day, there are 1000 new HIV infections among young women and adolescent girls. Prevention programme gaps remain huge,” said Michel Sidibé, the Executive Director of UNAIDS.
For prevention efforts to be sustainable, civil society should be meaningfully engaged in all national prevention coalitions, and their expertise and comparative advantage in implementation used. HIV prevention also needs to be adequately funded.
“Four main reasons that were holding us back were identified when we formed the coalition: gaps in political leadership, policy barriers to effective prevention, gaps in prevention financing and lack of systematic programme implementation at scale. With the adoption of the Global Prevention 2020 Road Map we committed ourselves to address these issues,” said David Parirenyatwa, the Minister of Health and Child Care of Zimbabwe.
More than 200 delegates, including 11 ministers of health from coalition countries, as well as ministers from three additional countries that newly joined the coalition—Botswana, the Islamic Republic of Iran and Myanmar—attended the launch event, held on 22 May at the 71st World Health Assembly in Geneva, Switzerland.

Feature Story
HIV transmission filmed live by French scientists
28 May 2018
28 May 2018 28 May 2018A team of French researchers has succeeded in filming HIV infecting a healthy cell. UNAIDS spoke to Morgane Bomsel, Research Team Director at the French National Center for Scientific Research (CNRS), about the feat.
What motivated you to film HIV transmission?
Morgane Bomsel: HIV transmission has not been studied much and we had no precise idea of the exact sequence of events leading to HIV infection of genital fluids during sexual intercourse. Neither did we know how immune cells are infected and what the consequences are. The vast majority of new HIV infections are acquired via the genital and rectal mucosa; however, the outer layer, the epithelium, of those tissues varies and affects how HIV enters the body.
What were the challenges?
MB: The challenges involved building an experimental model that mimicked genital mucosa infected by genital fluids suitable for live imaging. We reconstructed in vitro human male urethral mucosa based on human cells, the surface of which had been engineered to be red, and an infected white blood cell (a T lymphocyte, the main infectious element in sexual fluids) that was engineered to be fluorescent green and in turn would produce fluorescent green HIV infectious particles.
We had to render the system fluorescent to be able to visualize it and track HIV entry in the mucosa by live fluorescent scanning. Finally, we had to devise a system to allow the microscope lens to visualize the contact between the cells. All of this, of course, was done in an extremely secure setting and all of us were wearing two pairs of gloves and a hat, a coat, glasses and a mask.
When did you know you had a breakthrough?
MB: Our eureka moment was when we captured on film the spillage of a string of viruses, like a gun showering bullets. This lasts for a couple of hours and then, as if the infected cell has lost interest, it detaches itself and moves on.
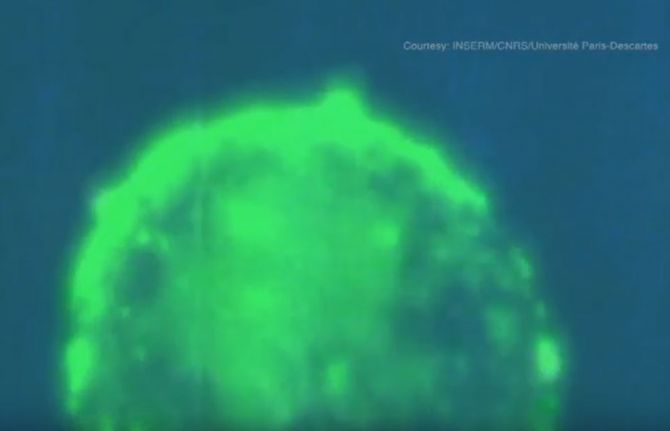
Please walk us through the video
MB: The HIV-infected cells are labelled in green and produce fluorescent viruses that appear as green dots.
What we see is the HIV-infected cell attaching itself closely to the outer layer, the epithelium, of healthy reconstructed cells of a genital tract mucosal lining.
White blood cells of the immune system, macrophages, that usually engulf foreign substances, debris or cancer cells are seen engulfing the red particles slightly moving next to the blue macrophage nucleus.
The HIV-infected cell approaches the surface of the mucosa and places itself gently on the surface. Owing to, or induced by, contact, the infected cell recruits preformed viruses towards the cell contact (the intense yellow green patches) and then starts to spit those preformed viruses as full infectious viruses that appear as green dots.
These green viruses penetrate the outer layer of the tissue by a process called transcytosis—a type of transcellular transportation. The viruses enter the cell and exit, still infectious, at the other side of the epithelial barrier. As a result, HIV penetrates the types of white blood cells responsible for detecting, engulfing and destroying foreign substances and infects them. Once inside the nucleus, the virus inserts itself in the genetic material, the DNA, and the blood cells that are meant to protect the body start to produce viruses.
Interestingly enough, the video showed that the production of viruses does not last very long. After three weeks, the infected white blood cells become dormant and a reservoir of white blood cells is formed.
What makes HIV particularly tricky to cure?
MB: Attempts to cure HIV have been very difficult because of the dormant infected white blood cells. Those cells are hard for the immune system to find and kill, and for the scientist to study. Antiretroviral medicines prevent the virus from spreading throughout the body and the immune system targets cells that are actively transcribing viral DNA. But because of the reservoir, these cells become a problem if a patient stops taking antiretroviral therapy. They can slowly awaken, allowing the virus to replicate freely.
Related links


Feature Story
Civil society builds a coalition to accelerate results in western and central Africa
15 May 2018
15 May 2018 15 May 2018Western and central Africa has faced many challenges, from conflicts and humanitarian crises to political instability and the devastating Ebola epidemics. At a time when the global response to HIV is accelerating, millions of people in the region are being left behind. Globally in 2016, 70% of all people living with HIV knew their HIV status, 53% of all people living with HIV were accessing treatment and 44% of all people living with HIV were virally suppressed. In contrast, the western and central African region lags behind, achieving only 42%, 35% and 25%, respectively, in 2016. The gap is considerable in that region: 4.0 million people living with HIV are not receiving treatment and 310 000 adults and children died from AIDS-related illnesses in 2016.
In order to share experiences, challenges and information on successful programmes, representatives of civil society organizations involved in the AIDS responses across western and central Africa gathered in Somone, Senegal, from 7 to 10 May. Technical and financial partners also took part in the discussions.
“Eighty civil society leaders from 17 countries in western and central Africa are eager to take up a central role in the implementation of the western and central Africa catch-up plan as actors of social change and political transformation,” said Patrick Brenny, the Director of the UNAIDS Regional Support Team for Western and Central Africa.
The participants developed innovative solutions to overcome barriers to national AIDS responses and to improve the unity and collaboration of local civil society organizations. They examined progress and setbacks in the implementation of national catch-up plans and shared experiences of violations of human rights related to HIV status and stigma and discrimination.
Consensus emerged that efforts should be focused on bridging the gaps in paediatric care and treatment, in particular in the context of the lack of social protection schemes for orphans and other children made vulnerable by AIDS. The region has seen a worrying trend in increasing mortality among adolescents living with HIV. Lack of access to comprehensive sexuality education, a high age of consent to access sexual and reproductive health information, services and treatment without parental agreement and taboos around youth sexuality were raised as some of the obstacles to be overcome.
Successful innovations and programmes with key populations and other vulnerable groups were shared. There was wide consensus about the role of community health systems to reach remote populations and vulnerable groups, while protecting confidentiality.
“It is high time that we increase investments to guarantee access to antiretroviral medicines, have better paediatric medicines, implement family testing approaches and scale up social protection programmes to protect all vulnerable mothers and children,” said Christine Kafando, Coordinator of the Hope for Tomorrow Association in Burkina Faso.
The participants will build on the progress made by organizing national dialogues around the catch-up plan for the region. The development of a regional platform for advocacy and technical support will be further discussed to enable stronger and more resilient civil society to play roles in national AIDS responses and other global health challenges.
“Each stakeholder gathered here plays a central role in their respective national AIDS response. Each brings invaluable experience to the table. We need to build on this energy to renew our commitment to work together for much needed breakthroughs for the region to bring HIV under control,” said Daouda Diouf, the Executive Director of ENDA Santé in Senegal.
Related

Feature Story
Artificial intelligence not necessarily beneficial for LGBTI community
21 May 2018
21 May 2018 21 May 2018One of the most watched events of the year got Cynthia Weber wondering: can the use by Sky News of artificial intelligence (AI) at the wedding of Prince Harry and Meghan Markle be a good thing?
For the first time in history, a news broadcaster used AI facial recognition technology during a live broadcast. Cynthia, a professor of international relations and gender studies at the University of Sussex, explained that using software to name wedding guests may be a nifty trick, but there are worries about the implications.
“Some claim that this technology can identify a person’s sexual orientation,” Cynthia said while speaking during an event for the International Day against Homophobia, Transphobia and Biphobia in Geneva at UNAIDS headquarters.
Referring to a Stanford University study that analysed more than 35 000 images on a United States dating website of white, able-bodied, 18–40-year-olds, the researchers compared their AI-generated sexual orientations against sexual orientations researchers found in dating profiles. The study claimed that AI facial recognition technology could determine a person’s sexual orientation with up to a 30% greater accuracy than people can.
Cynthia said that LGBTI advocacy organizations labelled the study junk science—the study used a skewed sampling in terms of race and age and the study equates sexual orientation with sexual activity. “The result is that the study’s artificial intelligence algorithm only finds what it was programmed to find: stereotypes about straights, gays and lesbians,” said Cynthia.
Cynthia believes that AI knowledge may generate opportunities in many fields, but sees far more risks and dangers than advantages for LGBTI people.
When AI meets facial recognition technology and a sexual orientation algorithm, at least four issues arise. First, privacy. In national and international law, a person’s face is not protected by privacy laws. That allows faces to be scanned and read by everyone, from governments to Sky News.
Secondly, accuracy. “In a world beyond the royal wedding, artificial intelligence facial recognition technology is far from perfect, even when it just tries to match names with faces, much less when it tries to match presumed sexual orientations with faces,” Cynthia said.
For Cynthia, the key issue is knowledge. How does a sexual orientation algorithm know better than an individual his or her sexuality? Cynthia considers the binary approach of code and computer-readable data not compatible with the vast gender and sexuality spectrum.
Finally, the issue of what the AI information will be used for worries Cynthia. “Let Sky News use it for wedding commentary, but what if the police use it in countries where homosexuality is outlawed?” Cynthia asked.
For Cynthia, AI and sexual orientation are not necessarily mutually beneficial. Cynthia understands that AI influences imagination and drives innovation, but believes that categorization of people usually introduces more harms than benefits.
Cynthia concluded by saying, “People have to make sure that artificial intelligence is ethically driven, not just technologically driven.”
The event was organized with the Swiss LGBTI Pride@Work association and UN Globe, a United Nations-wide LGBTI organization, and was held on 16 May.
Partner
International Day against Homophobia, Transphobia and Biphobia

Feature Story
Ending double jeopardy for women with HIV
18 May 2018
18 May 2018 18 May 2018A new US$ 30 million partnership to help end cervical cancer led by the United States President’s Emergency Plan for AIDS Relief (PEPFAR), the George W. Bush Institute and UNAIDS will accelerate life-saving efforts in eight African countries.
Studies show that women living with HIV are four to five times more likely to develop invasive cervical cancer. However, the disease is preventable through screening and early treatment of precancerous lesions. Early detection and treatment of cervical cancer can dramatically increase a woman’s chance of survival—women with preinvasive lesions have a five-year survival rate of nearly 100%.
Because of the high prevalence of HIV in sub-Saharan Africa, and because women in sub-Saharan Africa are not screened or treated as early or frequently as women in other parts of the world, cervical cancer remains the number one cancer killer of women in the region.
To address the disproportionate risk of cervical cancer among women living with HIV and the need for increased rates of screening and treatment in sub-Saharan Africa, PEPFAR the George W. Bush Institute and UNAIDS recently announced a new partnership—the Partnership to End AIDS and Cervical Cancer—designed to effectively eliminate cervical cancer deaths among women living with HIV in sub-Saharan Africa within a generation. The partnership will build on successful efforts over the past seven years of the Pink Ribbon Red Ribbon initiative and, pending Congressional approval, will be supported by an initial investment of US$ 30 million from PEPFAR.
“When we confront suffering—when we save lives—we breath hope into devastated populations, strengthen and stabilize society, and make our country and the world safer,” said President George W. Bush. “This week, we are announcing the next phase of our partnership with the United States President’s Emergency Plan for AIDS Relief and UNAIDS: a plan to effectively eliminate cervical cancer amongst HIV-positive women within a generation.”
The partnership will focus its work in eight sub-Saharan African countries where the burdens of HIV and cervical cancer are high—Botswana, Lesotho, Malawi, Mozambique, Namibia, Swaziland, Zambia and Zimbabwe. There are about 6 million women living with HIV in those eight countries. More than 100 000 women are diagnosed annually with cervical cancer in sub-Saharan Africa.
“The partnership will allow us to screen for, and treat, precancerous lesions among women living with HIV like never before,” said Michel Sidibé, the Executive Director of UNAIDS. “The partnership’s new strategy, which includes cervical cancer screening every two years for women living with HIV over the age of 30 years, aims to reduce cervical cancer incidence by 95% among this population in eight sub-Saharan African countries.”
The partnership will engage with governments in each of the countries to ensure that women and girls living with HIV are a priority in national cervical cancer prevention and control programmes. It will also leverage the powerful advocacy of first ladies, ministers, civil society, global health leaders and funders to improve implementation efforts and speed progress against the goal of eliminating cervical cancer.
“Thanks to the generosity of the American people, the United States President’s Emergency Plan for AIDS Relief has saved the lives of millions of HIV-positive women around the world,” said Deborah Birx, United States Global AIDS Coordinator and Special Representative for Global Health Diplomacy. “We must ensure these same women—mothers, daughters, aunts, and grandmothers—who are living with HIV and thriving do not succumb to cervical cancer.”
The new partnership builds on the successful efforts of the Pink Ribbon Red Ribbon initiative. Since its inception in 2011, Pink Ribbon Red Ribbon and its partners have screened more than half a million women for cervical cancer in Botswana, Ethiopia, the United Republic of Tanzania and Zambia, treated almost 32 000 women for precancerous lesions and vaccinated almost 150 000 girls aged 9–13 years against human papillomavirus type 2.
Partner






Feature Story
Health is made at home, hospitals are for repairs
22 May 2018
22 May 2018 22 May 2018Calls to increase the number of trained and paid community health workers and reach more people with primary health care have been made for decades. However, countries are still struggling to expand the number of health workers serving in their own communities. This is despite overwhelming evidence of the gains made through such programmes in improving overall health, particularly maternal health and child health.
Rwanda’s investment in a combination of community-based insurance and community health workers led to the lowest maternal mortality in history for the country, showing that investments save lives.
“Africa bears 25% of the global disease burden, but has barely 3% of all health workers,” said Michel Sidibé, Executive Director of UNAIDS. “We need a shift in perspective to invest in community health workers to ensure healthy families and health security and to reach the people left behind.”
Forty years after the Declaration of Alma-Ata, which identified primary health care as the key to attaining health for all, global health leaders came together at an event to promote the effectiveness of community health workers by sharing their experiences and looking at ways of advancing the agenda on a global scale.
The event, convened by Ecuador and Ethiopia, was held on the sidelines of the 71st World Health Assembly in Geneva, Switzerland, on 21 May and joined together community health workers, ministers of health, programme managers, the Director-General of the World Health Organization, Tedros Adhanom Ghebreyesus, Graça Machel, a co-founder of the Elders, and Mr Sidibé.
Sunil Kumar, a community health worker in India, gave his account of how important medical services are to people in remote communities. He explained how he managed to reach a pregnant woman in a remote area of India in the rainy season. Despite a dangerously overflowing river, he and his colleague went the extra mile to ensure that her baby was delivered safely—a stark reminder of the unique added value of community health workers.
The Ministers of Health of Ecuador, Ethiopia and Namibia and the Permanent Secretary of the United Republic of Tanzania talked about the successes and challenges they are facing in trying to expand the number of community health workers in their countries.
The State Minister of Health of Ethiopia shared a successful model that has been scaled up in the country. Ethiopia now has more than 38 000 paid and trained health extension workers following the 2004 launch of the health extension programme, financed by a mix of government and international donor funds. The programme has made significant contributions to declines in maternal mortality, improvements in hygiene and sanitation and a reduction in major communicable diseases.
“We are seeing momentum for universal health coverage,” said Mr Tedros. “Primary health care is both promotion and prevention and community health workers are the backbone.”
In July 2017, the African Union Commission launched an initiative to recruit, train and deploy 2 million community health workers by 2020, an initiative championed by UNAIDS. UNAIDS, in close collaboration with the World Health Organization and the United Nations Children’s Fund (UNICEF), recently supported the African Union Commission to undertake the first stocktaking exercise on the status of community health workers across the whole of Africa. The findings and recommendations will be submitted to heads of state during the African Union Summit in June 2018. UNAIDS is supporting countries to implement this important initiative.
Although positive steps have been made, many countries are still struggling to scale up. “In Namibia, we adopted the Ethiopian model, as it has been so successful,” said the Minister of Health of Namibia. “We trained 2000 people, which is small for a population of 2.3 million, and not all have been deployed due to budget cuts, inefficiencies and fraudulent use of resources.”
Other challenges cited by the speakers include transport issues, a lack of technology and communications support, such as smart phones, and political leadership at the very top levels.
“Health systems need to be built from the bottom up,” said Bent Høie, Norwegian Minister of Health and Care Services. “And that starts with community health workers.”
Stefan Swartling Peterson, Chief of Health at UNICEF, embodied the sentiment of the meeting by sharing a saying his professor, Francis Omaswa, former Minister of Health of Uganda, often reminded him of, “Health is made at home, hospitals are for repairs,” and stressed that community health workers cannot be alone, that systems, supply chains and data management are needed to make the programmes a true success.
Urging for a global movement with every country making a commitment to increase the number of trained and paid community health workers, Graça Machel concluded by saying, “Let us not come back in 2030 and say we promised but we failed … it is not allowed.”




Feature Story
Women living with HIV in Rajasthan push for social protection and economic opportunities
17 May 2018
17 May 2018 17 May 2018Women living with HIV in Rajasthan, India, have come together to lobby the State Government of Rajasthan for improved provision of social protection services. The Global Alliance for Human Rights and the Rajasthan Network of People Living with HIV organized an advocacy session in Jaipur on 15 May with more than 100 women living with HIV during which they presented their needs, including dairy booths for income generation and schooling for adolescents living with HIV.
In addition to the importance of access to social protection and economic opportunities, discussions were also held around the global 90–90–90 targets, the elimination of mother-to-child transmission of HIV by 2020 and ending AIDS by 2030. The Indian HIV/AIDS Act 2017 and its importance in protecting against discrimination and opening access to the law in the event of human rights violations against people living with and affected by HIV in India were also discussed.
The women living with HIV presented some heartening real-life stories on their struggle to look after their families. A widow with three children said, “I am facing stigma and discrimination in my family and I am fighting hard to ensure that my rights to property are protected so that I can continue to provide good care to my children. I am under a lot of pressure to withdraw, but I will not give up the fight.”
Many commitments were made during the session. “We commit ourselves to look for legal clearance in support of the allocation of dairy booths for 1000 women living with HIV in Rajasthan,” said Devi Singh Bhatti, a politician and former member of the Rajasthan Legislative Assembly.
Brijesh Dubey, of the Global Alliance for Human Rights and Rajasthan Network of People Living with HIV, concluded the event with a strong message to the officials of the Government of Rajasthan and other stakeholders present. “The Rajasthan Network of People Living with HIV will continue to focus its efforts on two major areas—firstly, the roll-out of the HIV/AIDS Act 2017 through the establishment of legal clinics and, secondly, ensuring access to quality livelihood options for people living with HIV, especially women and adolescents living with HIV.”
Region/country




Feature Story
Addressing the detrimental health and human rights impacts of criminal laws
08 May 2018
08 May 2018 08 May 2018People have a fundamental human right to make decisions about their lives and bodies. These rights relate to personal choices on, among other things, health care and treatment. For sexual and reproductive rights, key issues include the right of people to decide when, whether and with whom to have sex, to have children and to get married and their ability to express their gender and sexuality.
Leading legal experts from around the world recently met to lay the foundations for a set of principles to address the misuse and abuse of criminal laws that affect basic human rights and impact on health and equality. The principles will be developed in the coming months and will guide civil society and policy-makers in the development and use of laws that guarantee human rights and protect public health.
Tim Martineau, UNAIDS Deputy Executive Director, Programme, a.i., noted at the outset of the meeting that, “While there is significant progress in HIV prevention, treatment and care, there is a big discrepancy in HIV prevention in relation to key populations, who are more vulnerable to HIV infection in many respects because of a lack of legal protection and the unjust criminalization of their behaviour.”
The legal experts focused on criminalization related to sexuality, reproduction, personal drug use and the overly broad criminalization of HIV nondisclosure, exposure and transmission. Around the world, same-sex sexual practices are criminalized in 73 countries, with 13 states imposing the death penalty. Sex work is criminalized in approximatively 116 countries globally and some 72 countries criminalize HIV non-disclosure, exposure or transmission. Criminal laws often increase stigma against already marginalized and excluded groups and have been linked to discrimination and the denial of critical health services. Criminalization also creates an environment in which people are less likely to seek police assistance when their rights have been violated.
Kate Gilmore, the United Nations Deputy High Commissioner for Human Rights, emphasized that the criminal law plays an essential role in the recognition, protection and enforcement of rights, including by tackling impunity for violations of those rights. “Our purpose here is to raise the shield of criminal law by lowering its sword, ensuring better protection through criminal law by reducing the abuse of it.”
Sam Zarifi, the Secretary General of the International Commission of Jurists, said, “The misuse of the criminal law affects the most marginalized people and, in particular, the dispossessed and disenfranchised.”
The meeting was held on 3 and 4 May and was led by the International Commission of Jurists, in partnership with UNAIDS and the Office of the United Nations High Commissioner for Human Rights.
Related



Feature Story
What needs to be done to Fast-Track social protection to end AIDS?
09 May 2018
09 May 2018 09 May 2018In 2016, Member States agreed a set of targets at the United Nations High-Level Meeting on Ending AIDS to be met to put the world on course to end the AIDS epidemic by 2030. One of those targets was to strengthen national social and child protection systems to ensure that, by 2020, 75% of people living with, at risk of or affected by HIV benefit from HIV-sensitive social protection. The target is human rights-based. It feeds into and benefits from promoting, protecting and fulfilling all human rights and the dignity of all people living with, at risk of or affected by HIV.
Evidence of how social protection programmes meet the needs of people who are poor and excluded and benefit people living with, at risk of or affected by HIV is increasing. The question is not whether the AIDS response should increase attention to social protection, but how best to leverage resources and partnerships of movements working on ending poverty and inequality to work effectively towards ending AIDS.
Of 127 countries reporting in the UNAIDS National Composite Policy Index in 2017, 109 (86%) stated that they had an approved social protection strategy, policy or framework in 2016, and 99 of those countries (78%) were implementing those programmes. A total of 85 countries stated that their strategies were HIV-sensitive to at least some extent. More than half (47) of the 87 countries with a coordinating mechanism for their social protection strategy have included their national AIDS programme in that structure. However, only 12 countries reported that their social protection strategies were fully HIV-sensitive.
To step up efforts to get social protection on the Fast-Track, UNAIDS recently held a conference at which the participants heard about how to strengthen national social and child protection systems. The conference focused on three objectives: strengthening the links with social and other movements for ending poverty and inequality; intensifying action on social protection; and reinvigorating programming for HIV, food security and nutrition.
“Stronger linkages are required across health, education and community systems to reduce the vulnerability of people living with, at risk of and affected by HIV through social protection services,” said Tim Martineau, UNAIDS Deputy Executive Director, Programme, a.i.
The event also saw the launch of a new UNAIDS report, Social protection: a Fast-Track commitment to end AIDS. The report provides guidance on how to scale up what works in the context of different HIV epidemics and for different populations. It also provides guidance to governments, people living with or affected by HIV, policy-makers and other stakeholders on how to intensify the integration of HIV with social protection and other programmes for ending poverty and inequality towards ending AIDS.
“We must remember that without improving the material and emotional well-being of people, we cannot end the AIDS epidemic,” said Denys Dmytriiev, from the All Ukrainian Network of People Living with HIV.
The International Conference on Fast-Tracking Social Protection to End AIDS was held in Geneva, Switzerland, on 25 and 26 April.
Related







Feature Story
UNAIDS Executive Director puts the spotlight on the HIV response in Lesotho, South Africa and Zambia during five-day visit
11 May 2018
11 May 2018 11 May 2018The UNAIDS Executive Director, Michel Sidibé, has completed a five-day visit to three countries in southern Africa. The mission included high-level political discussions, the launch of the Lesotho HIV health and situation room and a frank and open dialogue with women activists about how to address sexual harassment and abuse.
Beginning in Lesotho, Mr Sidibé attended the launch of the HIV health and situation room with the Deputy Prime Minister, Monyane Moleleki. Special guest Naomi Campbell was invited by UNAIDS to join the two-day country visit to learn more about the HIV response.
The Lesotho HIV and health situation room shows real-time service delivery data, producing a comprehensive picture and understanding of Lesotho’s HIV epidemic. It enables quick feedback on results at the national and community levels and identifies bottlenecks in access to health-care services.
“The launch of the Lesotho HIV and health situation room gives us access to data to shape impactful and efficient health programmes. These are the kind of innovations that will bring services to those who need them most and ensure that no one is left behind by the AIDS response,” said Michel Sidibé, the UNAIDS Executive Director.
On the eve of the launch, Mr Sidibé and Ms Campbell visited the Queen II Hospital in Maseru, Lesotho, and met with young women living with HIV and others affected by the epidemic.
“I commend the Government of Lesotho and its partners for the progress made in the AIDS response. But the work is far from done. The reality is that we are not reaching adolescent girls and young women. I leave Lesotho today empowered, inspired, encouraged and determined to do all I can to highlight this critical issue,” said Ms Campbell.
In South Africa, Mr Sidibé addressed the Pan African Parliament and underlined the importance of integrated health approaches that were people-centred. He urged parliamentarians to commit more domestic funding for health services to increase the sustainability of the AIDS response and to put in place more preventative measures to improve people’s health. In addition, he called for laws to protect women and vulnerable groups.
Mr Sidibé left the parliamentary session to meet civil society activists concerned by UNAIDS' response to allegations of sexual harassment and abuse in the organization.
At a follow-up meeting the next day, Mr Sidibé and women activists met to discuss their concerns.
Mr Sidibé agreed with activists to issue a statement following the meeting. The statement begins:
‘During my recent visit to South Africa, I listened carefully to you, I heard you. The HIV epidemic is inextricably linked to sexual and gender-based violence and the two can never be separated. We need the passion of advocates to move issues forward.`
During his visit to South Africa, Mr Sidibé held separate meetings with the President, Cyril Ramaphosa, the Deputy President and South African National AIDS Council Chair, David Mabuza, and the Minister of Health, Aaron Motsoaledi. They discussed plans to increase the number of people on treatment by 2 million by 2020 and the need to empower local and provincial authorities to bring treatment and prevention services closer to vulnerable communities.
The last leg of Mr Sidibé’s visit saw him arrive in Lusaka, Zambia, to confer the 2018 UNAIDS Leadership Award upon Kenneth Kaunda for his efforts in strengthening the AIDS response.


















