Feature Story
“I also need to be happy”: Anna Morena’s story
25 June 2020
25 June 2020 25 June 2020Officially, she calls herself Juliana, but she also goes by the name Anna Morena and has an organization of the same name—the Anna Foundation Uganda.
The small, youth-led organization promotes sexual and reproductive health and rights, HIV prevention, advocacy, research, entrepreneurship and fundraising for the transgender community in central Uganda.
As a response to the malnutrition experienced by transgender people because of the COVID-19 outbreak, the foundation has raised US$ 1600 from a private donor to support transgender people and their dependents with food relief, which has reached more than 200 people.
Members of the foundation volunteer their time to conduct referrals for mental health and supply medical services, including deliveries of treatment and hormone therapy to transgender people who cannot currently access facilities due to the COVID-19 pandemic.
Ms Morena named herself and the foundation in memory of a friend who moved to Kampala, the capital of Uganda, at the age of 16 years. She was working as a sex worker to survive, met a man in a nightclub one night and was found dead the next day.
“I thought that maybe I could be “Anna” too, because she had a dream—to live as a normal person,” said Ms Morena wistfully.
Ms Morena doesn’t like labels, but she refers to herself as a “trans girl” because she wants people to know that she’s “not just a sex worker.”
She is open about being a sex worker so she can encourage others to come out and speak about it. She also volunteers to educate people about being transgender, which she does “out of love.” The sex work is to put food on the table.
“Most of the trans women I know are doing sex work. They are usually between the ages of 16 and 25 years, a time when hormones are high and one’s understanding of sexuality and gender identity is still developing,” she said.
Globally, transgender people are 12 times more likely to become infected with HIV than the general population. Nineteen countries worldwide, including Uganda, prosecute and/or criminalize transgender people.
In their daily lives, transgender people experience exclusion from family and society, barriers to employment and extreme forms of sexual, physical, emotional and psychological violence. According to Ms Morena, the COVID-19 pandemic is making things worse.
“COVID-19 has led to an increase in gender-based violence and a scarcity in commodities such as condoms and lubricants. Most sex workers are still doing sex work so that they can survive and we are seeing a rise in infections,” said Ms Morena.
She said prices for essentials such as mobile phone data have risen, making it harder for community-based transgender organizations to stay connected to their members.
In the absence of funding for vocational training, the only choice for transgender people who want to make a difference is to volunteer, said Ms Morena, because there is limited donor funding for transgender organizations. “Donors are very specific about what they will support, meaning there is a lot of competition for funding,” she said.
In addition, there is limited data on transgender people in the eastern and southern African region and Ms Morena believes that donors are not primarily interested in funding community-led research. But, she said, research is critical. “It is a way to help our governments understand the specific needs we have; it helps influence change and policies.”
Influencing change is something that Ms Morena does every day. During workshops run by the foundation, in partnership with other transgender and female-led community organizations, she tries to educate people about what it feels like to live in a transgender body by getting them to draw a picture of their bodies on a piece of paper they place on top of their heads.
Drawing one’s body out of sight always guarantees that it comes out a mess. This is Ms Morena’s advocacy punchline.
She holds up the drawing and tells them, “This is the pain I have to go through daily. This is how the world sees a transgender person.”
“This is not the body I want. I want to transition, but I don’t have the support of my family. I honestly love them. At times I try to do what I can to make them comfortable, but I also need to be happy,” she said.
This is the reason why the transgender community is so important, said Ms Morena. Solidarity helps.
“Trans women need safe spaces, places to stay and access to mental health services,” said Ms Morena. “The Government of Uganda is not willing to facilitate such spaces, so community-based organizations must bring these services until the fight for decriminalization has been won.”
Our work
Region/country
Related

Feature Story
Survey shows that many people lack multimonth HIV treatment in Latin America
24 June 2020
24 June 2020 24 June 2020Once the COVID-19 lockdown in her country was put in place, Marisela Mariño (not her real name), a transgender woman living with HIV, immediately contacted her treatment provider, convincing them to supply her with antiretroviral therapy to last at least two months.
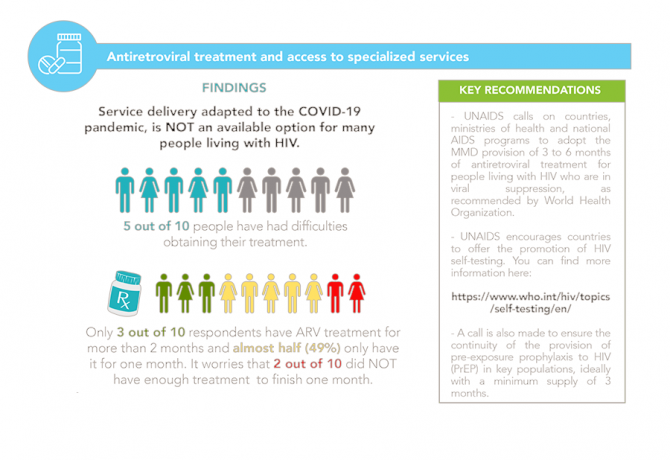
“I was saved by having the phone number of one of the health promoters at the clinic I attend,” said Ms Mariño. But now she, like seven out of 10 people who responded to a Latin American regional survey on the needs of people living with HIV during the COVID-19 pandemic, does not have enough antiretroviral medicines for a lockdown of more than 60 days.
From the online survey, which was answered by 2300 people from 28 countries in the region, it was seen that despite the communication efforts by national health authorities and the international organizations that are leading the response to COVID-19, 31% of people stated that they had not received sufficient information on preventing the transmission of the new coronavirus. More than half, 56%, expressed that they do not have sufficient personal protective equipment, while only 22% of people think that masks are a useful protection against COVID-19.
Claudia Cardenal (not her real name), another transgender woman in the region, says that the offer of services adapted to the COVID-19 pandemic is not reflected in the options for people living with HIV. Ms Cardenal only has antiretroviral treatment for one more month, despite the World Health Organization recommendation that people living with HIV have at least a three-month supply.
The survey also shows that five out of 10 people are having difficulties in obtaining their antiretroviral treatment during the pandemic and less than two out of 10 people had antiretroviral medicines delivered to their homes.
Only three out of 10 people have been offered the option of telemedicine, and four out of 10 people living with HIV in Latin America state that they need psychological support to address anxiety related to COVID-19.
Stigma and discrimination continues to be an important barrier for people living with HIV to fully access their rights. More than half of the people surveyed, 56%, believe that they could suffer physical, psychological or verbal violence due to living with HIV in the midst of the COVID-19 pandemic. Forty per cent answered that they do not know where to go or call in the event that they encounter violence or discrimination due to living with HIV and the fear of discrimination caused three out of 10 people to refrain from accessing services in the midst of lockdowns.
Confinement can increase and incentivize stigma and discrimination. For example, in countries that have rules on leaving one’s home under the lockdown based on gender, violence to people with a different gender identity or expression than that appearing on their official identification may increase.
Job loss or lack of income was a top concern in the findings of the survey. Mobility restrictions and compulsory quarantines have deprived four out of 10 people who needed to leave their homes for work of their income, which means that four out of 10 people require nutritional support and/or cash transfers.
From the results of the survey, it is clear that the response to COVID-19 should consider the realities of people’s lives and focus on removing the barriers that people face to protect themselves and their communities.
Countries, ministries of health and national AIDS programmes should ensure access to three months or more of antiretroviral therapy by all people living with HIV, including refugees and migrants. In addition, the provision of food and other social protection services, including temporary shelters for key populations, people living with HIV and other vulnerable people, must be ensured.
The provision of services and support to the populations most affected by violence, especially women and girls, also needs to be a key priority for governments.
“This evidence has been shared with Cosponsors, national AIDS programmes and civil society organizations. I urge them to push for multimonth dispensing of antiretroviral therapy, social protection measures focusing on key populations and people living with HIV and support for mental health initiatives,” said César Núñez, Director of the UNAIDS Regional Support Team for Latin America and the Caribbean.
Related


Press Release
COVID-19 could affect the availability and cost of antiretroviral medicines, but the risks can be mitigated
22 June 2020 22 June 2020UNAIDS study shows that the impact on production and logistics caused by COVID-19 could have a significant effect on antiretroviral therapy supply worldwide, but steps taken now could lessen the damage done
GENEVA, 22 June 2020— A new analysis by UNAIDS has revealed the potential impacts that the COVID-19 pandemic could have in low- and middle-income countries around the world on supplies of the generic antiretroviral medicines used to treat HIV.
The UNAIDS survey discovered that the lockdowns and border closures imposed to stop COVID-19 are impacting both the production of medicines and their distribution, potentially leading to increases in their cost and to supply issues, including stock-outs over the next two months.
“It is vital that countries urgently make plans now to mitigate the possibility and impacts of higher costs and reduced availability of antiretroviral medicines,” said Winnie Byanyima, Executive Director of UNAIDS. “I call on countries and buyers of HIV medicines to act swiftly in order to ensure that everyone who is currently on treatment continues to be on it, saving lives and stopping new HIV infections.”
Since 24.5 million people were on antiretroviral therapy at the end of June 2019, millions of people could be at risk of harm—both to themselves and others owing to an increased risk of HIV transmission—if they cannot continue to access their treatment. A recent modelling exercise estimated that a six-month disruption of antiretroviral therapy in sub-Saharan Africa alone could lead to 500 000 additional AIDS-related deaths.
The production of antiretroviral medicines has been affected by several factors. Air and sea transport is being severely curtailed, hampering the distribution of the raw materials and other products, such as packaging material, that pharmaceutical companies need to manufacture the medicines. Physical distancing and lockdowns are also restricting the levels of human resources available in manufacturing facilities. The combined result of shortages of materials and workforces could lead to supply issues and pressure on prices in the coming months, with some of the regimens for first-line treatment and those for children projected to be the severest hit.
An array of circumstances are conspiring to add pressure on the overall cost of finished antiretroviral medicines. Increased overhead and transport costs, the need for alternative sourcing of key starting materials and active pharmaceutical ingredients and currency fluctuations caused by the forecasted economic shock are combining to push up the cost of some antiretroviral regimens. It has been estimated that a 10–25% increase in these could result in an annual increase in the final cost of exported antiretroviral medicines from India alone of between US$ 100 million and US$ 225 million. Considering that in 2018 there was an HIV financing shortfall of more than US$ 7 billion, the world cannot afford an added burden on investments in the AIDS response.
UNAIDS and partners are working to mitigate the impact. The Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) is providing immediate funding of up to US$ 1 billion to help countries to respond to COVID-19 and is expanding the use of its procurement platform to non-Global Fund recipients. The United States President’s Emergency Plan for AIDS Relief is promoting continuity of HIV care, implementing new strategies, such as telemedicine, and allowing some programme flexibility in reporting requirements, staffing and funding re-allocation. The World Health Organization is compiling, exchanging and analysing information on HIV services that have been impacted and is liaising with manufacturers of antiretroviral medicines for emergency supply and with countries to switch to available quality alternative products and on possible mitigation measures. UNAIDS has been coordinating efforts to address the procurement and supply management challenges of antiretroviral therapy caused by the COVID-19 response.
However, a series of policy recommendations on the coordinated action that should be taken by governments and suppliers in order to resolve these issues map out how to minimize the impacts on supply chains and prices. By managing effectively current and future stocks of antiretroviral medicines, supply can be continued for all who need treatment.
The UNAIDS analysis collected information from the eight generic manufacturers of antiretroviral medicines in India that together account for more than 80% of generic antiretroviral medicine production worldwide. Government departments in seven other countries that produce generic antiretroviral medicines and that account for most of the production of generic antiretroviral medicines in low- and middle-income countries domestically were also surveyed.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Our work
Documents
The impact of the COVID-19 response on the supply chain, availability and cost of generic antiretroviral medicines for HIV in low- and middle-income countries
22 June 2020
The objective of this report is to assess the situational landscape during mid-May 2020 surrounding the value chain of the production and distribution of generic antiretroviral medicines in low- and-middle-income countries and to provide recommendations on mitigating the risks of potential disruptions.




Feature Story
Local skills and knowledge help Senegalese community-led organizations deliver
18 June 2020
18 June 2020 18 June 2020Face masks, sanitizers and soap. Food packages and money to pay the rent. Information about how to protect yourself and your loved ones from the virus—the list goes on.
The necessities of life during the COVID-19 pandemic can be hard to come by, but communities are organizing and delivering services and much needed commodities to the people that need them the most. And communities with experience of responding to other epidemics are turning their lessons learned to COVID-19.
“Organizations led by and for people living with HIV and key populations are now spearheading urgently needed programmes to combat COVID-19 and secure the health and well-being of their communities,” said Demba Kone, the UNAIDS Country Director for Senegal.
Like in many other countries around the world, face masks and other personal protective equipment are in short supply in Senegal. However, the Enda Santé nongovernmental organization had a quick and efficient solution—the many local tailors and dressmakers, who are highly skilled and had a ready access to supplies of fabric. Responding to the call of “come work with us”, the tailors and dressmakers produced thousands of high-quality masks in a record time, and at a very low cost. And the local production meant that the money stayed in the local economy, which had been badly affected by the pandemic.
Enda Santé has also begun negotiating with donors that fund HIV programmes. Funds that had been allocated to HIV-related activities that could not be carried out in the current context have been re-allocated to support COVID-19-related activities in the most-affected communities.
Focusing the right resources at the right place is crucial when responding to outbreaks that are travelling fast through communities. Enda Santé therefore went to work to identify the communities that were the most vulnerable and in the greatest need.
Drawing on statistics generated by the government, as well as their own knowledge about the demography and availability and accessibility of health services, Enda Santé looked at poverty levels among communities, the neighbourhoods where overcrowding was the worst and where people had difficulty in accessing health care. It was clear that the people who were the most vulnerable to HIV were also now very vulnerable to COVID-19.
Enda Santé focused on those communities, distributing prevention materials and mobilizing young and female leaders from the community, training them to go door to door explaining how people could protect themselves, how to identify cases and how to get people into treatment centres.
It was obvious that many of the people affected by HIV that Enda Santé worked closely with—people living with HIV, sex workers, people who inject drugs and young women and adolescent girls—had lost their incomes because of the lockdown and were now struggling with the triple impact of HIV, COVID-19 and poverty. In response, Enda Santé organized the delivery of food and cash transfers.
Daouda Diouf, the Executive Director of Enda Santé, reflected on the process. “We had already learned how to do all of this work in the context of HIV, so we were transferring the skills we learned in responding to HIV for 25 years, and we moved to apply them to COVID-19. The speed of action, engaging community members and putting them at the centre of the work, the door-to-door approach, pre-empting the risk of transmission, delivering prevention packages, and so on. We were able to act very quickly.”
Our work
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
UNAIDS highlights six critical actions to put gender equality at the centre of COVID-19 responses
15 June 2020
15 June 2020 15 June 2020The AIDS response has taught the world the importance of protecting human rights and promoting gender equality when fighting a disease. COVID-19 has amplified that lesson.
Since the start of the COVID-19 pandemic, UNAIDS has repeated the call that governments must protect human rights and prevent and address gender-based violence—an issue that is even more vital now that lockdowns are putting women and girls at an even higher risk of intimate partner and sexual violence. Equally, UNAIDS has made it clear that sexual and reproductive health services should be recognized as the essential services they are.
To drive those messages to decision-making tables and to the front lines of the response, a new UNAIDS report shows how governments can confront the gendered and discriminatory impacts of COVID-19. Presenting six areas as imperatives to address the needs, and protect the rights, of women and girls during the pandemic, the report highlights the needs of women and girls in all their diversity, particularly the most marginalized, and the importance of access to essential health services. The neglected epidemic of gender-based violence, the misuse of criminal and punitive laws, the importance of education, health and well-being and the value of women’s work and making unpaid care work everybody’s work are also showcased.
“Just as HIV has held up a mirror to inequalities and injustices, the COVID-19 pandemic has put a spotlight on the discrimination that women and girls battle against every day of their lives,” said Winnie Byanyima, Executive Director of UNAIDS. “Many of the drivers of inequality in the HIV epidemic are the same as those driving inequality and injustice in the COVID-19 pandemic—both epidemics can only be successfully fought by putting gender equality at the centre of the response.”
The report underscores that sexual and reproductive health and rights are often the first to be sacrificed during epidemics and that the gains of the past decade must be protected. The report also makes it clear that scarce resources must be focused on the most marginalized women and girls, including sex workers, gender diverse people, women in prison and migrants and others without proof of employment or residence.
A selection of practical steps that UNAIDS has been taking with partners in countries to maintain essential health-care services, mobilize emergency legal protection and support populations facing human rights violations during the COVID-19 outbreak are presented.
For example, in Nigeria and Côte d’Ivoire UNAIDS is partnering with the International Community of Women Living with HIV to facilitate women living with HIV to work as community pharmacists, who help with the collection and home delivery of antiretroviral therapy and other medicines for people who were unable to access their treatment owing to COVID-19 restrictions.
In Latin America, the United Nations Population Fund and UNAIDS are offering contraceptives and HIV testing, as well as hygiene kits and information on gender-based violence and HIV, to women who are in compulsory quarantine after fleeing the Bolivarian Republic of Venezuela because of COVID-19.
In Morocco, UNAIDS, in partnership with the Ministry of Health, the Global Fund to Fight AIDS, Tuberculosis and Malaria and civil society, is mobilizing self-help groups, medical and psychosocial support and family mediation services for populations at higher risk of HIV. Collaborations between the government and civil society have helped to ensure continued access to antiretroviral therapy, opioid substitution therapy and food aid during the pandemic.
Above all, the report has the message that health, safety, dignity and rights, especially for women and girls, in all their diversity, must not be compromised and women should lead the call for change.
“Get out there and fight, use your voice to demand and take action for your communities,” added Ms Byanyima.
Six concrete measures to support women and girls in all their diversity in the context of the COVID-19 pandemic
Our work
Documents
Report of the UNAIDS Executive Director — Opening of the 46th meeting of the UNAIDS Programme Coordinating Board
23 June 2020
2020 is a critical year for our Joint Programme as we collectively define the path to getting back on track to ending the AIDS epidemic by 2030. Our revised timelines for adoption of the next strategy are highly ambitious. We need the full support of all the tremendously dedicated people in UNAIDS-within our staff, our board and all our stakeholders to make this happen.


Feature Story
New online resource for mental health services for key populations in Kazakhstan
15 June 2020
15 June 2020 15 June 2020The lockdowns and self-isolations imposed to fight the COVID-19 pandemic have affected everyone, key populations and people living with HIV included. Prolonged isolation and limited contact with family and friends have increased anxiety and depression and impacted quality of life, increasing the need for mental health services.
To respond to this need, an online platform that offers psychological services and support for people from key populations has been launched in Kazakhstan. On it, people can get answers to questions related to different aspects of mental health, request professional consultations with psychologists or psychotherapists and receive broader information about health and well-being.
“Anxiety, uncertainty, worries—these feelings are consequences of the quarantine and self-isolation during the coronavirus pandemic. For many people, the time spent in quarantine was difficult. Today, we see a greater need for psychological help and support. It was for this purpose that this platform was created for key populations,” said Nikolay Negay, Director-General of the Republican Scientific and Practical Center for Mental Health of the Kazakhstan Ministry of Health.
The platform was developed with the participation of people from community organizations, representatives of key populations and activists.
“During isolation, we supported each other as best we could through social networks, communication by phone, Skype, but there was a need for qualified professional help. We are glad that such assistance has become available, and for free. The resource is informative and answers many questions,” said Oksana Ibragimova, the acting President of the ALE Kazakhstan Union of People Living with HIV.
“An anonymous rapid needs assessment conducted by UNAIDS in Kazakhstan among people living with HIV and key populations found that around 60% of respondents needed psychosocial support during the COVID-19 lockdown. It was therefore decided to find a way to provide reliable information, advice and professional assistance to those who may need it,” said Gabriela Ionascu, UNAIDS Strategic Information Adviser for Central Asia.
The platform was created as an initiate of the Republican Scientific and Practical Center for Mental Health of the Kazakhstan Ministry of Health, with financial support from UNAIDS and technical assistance from the Kazakh Scientific Institute of Dermatology and Infectious Diseases of the Kazakhstan Ministry of Health.
Our work
Region/country
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025


Feature Story
New HIV community group in Guinea fighting COVID-19
12 June 2020
12 June 2020 12 June 2020Communities have always played an important role in the fight against epidemics in Africa. In the response to HIV, community involvement has been illustrated by a key principle: nothing for us without us. Since the beginning of the AIDS response, civil society has been on the front line, demanding access to treatment, calling for respect for human rights and supporting community-led HIV services.
In Guinea, community engagement has resulted in the continuous improvement of HIV programmes and to considerable progress in testing, prevention, treatment adherence and psychosocial support. The promotion and defence of human rights is also central to communities, and community engagement has contributed to tackling stigma and discrimination and to monitoring the quality of services and addressing challenges.
From the lessons learned from the 2013–2016 Ebola outbreak in the country, the need for the active participation of communities, alongside the public, in the COVID-19 response is clear. This is why the National Platform of Civil Society Organizations on HIV and TB (PNOSC-HIV/TB) was recently set up. Established with technical and financial support from UNAIDS and bringing together 28 associations, PNOSC-HIV/TB played a central role in the development of the Ministry of Health’s contingency plan to reduce the impact of COVID-19 on health services, particularly HIV services.
Focusing on populations that include prisoners, people in refugee camps and solidarity cities— places where people with disabilities live—PNOSC-HIV/TB is active in helping to prevent COVID-19, raising awareness about the importance of physical distancing through community mediators, local artists, the media and door-to-door outreach.
Psychosocial help is being given through a hotline run by two networks of people living with HIV, one of which is focusing on key populations. PNOSC-HIV/TB is also working to promote and scale up nationwide the multimonth dispensing strategy for antiretroviral therapy.
“PNOSC-HIV/TB will enable us to speak with one voice, to assert ourselves even more, to organize and strengthen our contribution to defeating COVID-19 and to the elimination of AIDS in Guinea by 2030,” said Mahawa Diallo Sylla, President of PNOSC-HIV/TB.
PNOSC-HIV/TB also participates in the Community Treatment Observatory, which monitors respect for human rights in the context of COVID-19 and reports violations to the government and the National Institute of Human Rights.
“I am impressed by PNOSC-HIV/TB’s willingness to close the gap in terms of their participation in the national response to HIV. I am confident that the momentum and energy generated since its establishment will have a lasting impact on the responses to HIV and COVID-19 in Guinea,” said Dado Sy Kagnassy, UNAIDS Country Director for Guinea.
Our work
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Five UNAIDS country directors taking the lead in the COVID-19 response
11 June 2020
11 June 2020 11 June 2020The experience of the UNAIDS Country Director for El Salvador, Celina Miranda, a trained medical doctor, has been very useful during the COVID-19 outbreak. When the United Nations Resident Coordinator nominated her to be the COVID-19 response team leader within the United Nations in the country, she was honoured.
“I accepted the challenge, since the experience of working at UNAIDS on HIV has given me the skills needed to handle these types of situations,” she said.
To date, she has handled six confirmed COVID-19 cases of United Nations personnel from different agencies. “Some went to hospital, while others self-quarantined, and all are already emerging from the acute stage,” Ms Miranda said.
A main task for COVID-19 coordinators is to determine whether local hospitals could admit and treat United Nations personnel and their dependents. El Salvador was not ready for the pandemic, she said, which added to the pressure.
Ms Miranda, along with four other UNAIDS country directors, has been nominated by the United Nations Country Teams as COVID-19 coordinators in their respective countries.
Vladanka Andreeva in Cambodia, Yafflo Ouattara in Chad, Job Sagbohan in Burkina Faso and Medhin Tsehaiu in Kenya have all felt honoured to take on such a responsibility.
Ms Andreeva explained how in early March the United Nations in Cambodia set up a United Nations Internal COVID-19 Preparedness and Response Team, and she was asked to lead the efforts in ensuring that more than 2500 United Nations staff and their dependents have access to the latest COVID-19 information, treatment, care and support. She developed a contingency plan for the United Nations family and supported the establishment of a medical evacuations process and mental health support services for staff.
Mr Sagbohan, a trained medical epidemiologist who has worked for the World Health Organization during Ebola and yellow fever outbreaks, said he spent a lot of time reassuring employees in order to overcome stress and fear. “Staff were scared, so during the lockdown period I got up to 300 calls a week despite the regular virtual town hall briefings for staff across Burkina Faso.”
He explained that despite UNAIDS’ size and lack of resources compared to other agencies, knowing about infectious diseases has helped greatly. He quickly requested focal points from different organizations and set up a United Nations taskforce against COVID-19. “I have been able to tap into a solid group of motivated people to help me and it has made all the difference.”
For Yafflo Ouattara, the COVID-19 coordinator role suits UNAIDS country directors perfectly. “We are used to getting buy-in from our Cosponsors, so joint teamwork is part of our DNA,” he said. His main task in Chad has been expanding intensive care units and setting up a strong referral system for the management of severe cases. Nearly 7000 United Nations employees and dependents are spread out across the country, some in places where there is no overnight care.
Like others, he also helped out with the national COVID-19 contingency plan to ensure that people living with HIV have access to treatment and care.
He said that the pandemic highlighted gaping holes in the country’s health system. “Not only were key investments in intensive care never made, some of the basics, like gloves, masks, soap, have been missing all along.”
Living in a COVID-19 world means a lot of readjustments. “We have an opportunity to step in and make our voices heard to overhaul systems,” Mr Ouattara said.
Medhin Tsehaiu agrees. She has been proud to see UNAIDS be part of the greater discussion.
“We are present and we are very actively and willingly doing our share,” she said. But she believes that COVID-19 has forever changed how people work.
All the virtual meetings and no travel has meant that people were much more available, so there was non-stop communication, but it was very time-consuming, she explained. “The crisis brought us together, whether we like it or not, and that has required a lot of collaboration,” Ms Tsehaiu said.
Aside from her long list of tasks as a COVID-19 coordinator, she and a few others started the United Nations Kenya solidarity fund. After much back and forth, they opened a bank account where staff can choose to contribute money during a three-month period that will be dispatched to people in need.
“It’s a way for employees to show empathy and support to the Kenyan people during these difficult times,” she said.
Speaking of solidarity, Ms Andreeva said that the pandemic really tested United Nations reform at the country level, not just in terms of responding to the pandemic but also regarding duty-of-care issues. According to a survey in May, 90% of the staff in Cambodia said that the United Nations leadership at the country level is making the right decisions managing the crisis.
During a virtual town hall meeting of 300 United Nations staff members in El Salvador recently, there was also positive feedback. Ms Miranda said she doesn’t ask for accolades or additional thanks. “I just enjoy helping people and seeing them recover, living their lives fully.”