Feature Story
Communities in crisis: The collapse of HIV lifelines in Eastern Europe and Central Asia
01 April 2025
01 April 2025 01 April 2025A support group session for families with children living with HIV had just ended in Dushanbe, Tajikistan, when the news broke: the US Government announced a funding freeze. The room fell silent. For many participants, this group—run by the Tajikistan Network of Women Living with HIV—was their only source of psychological and social support and a vital, trusted bridge to lifesaving medical services. As the network is funded by the US, there was fear for its continued existence.
“People are panicking,” said Tahmina Haidarova, Head of the Tajikistan Network. “They fear that if our support services shut down, women affected by HIV, families with children living with HIV and people from key populations, including those newly diagnosed, will have nowhere to turn for support.”
This fear is now rippling across Eastern Europe and Central Asia (EECA), where community-led organizations and civil society initiatives remain heavily dependent on international funding, particularly from the Global Fund to Fight AIDS, Tuberculosis and Malaria and the US Government (which also funds the Global Fund).
In the majority of EECA countries, national governments do fund antiretroviral (ARV) medicines. However, the broader ecosystem essential to ensuring access to HIV services and treatment —including community outreach, counseling, HIV prevention, peer-led support, and human rights advocacy—has historically been deprioritized by governments and has never been fully institutionalized into national health systems.
This failure to reach people with existing services has led to a devastating outcome: only half of all people living with HIV in the region are on treatment and EECA remains the only region in the world where AIDS-related deaths continue to rise.
Across the region, many people affected by HIV and members of key populations actively avoid healthcare services due to fear of criminalization, stigma, and past experiences of discrimination. Without trusted community organizations to support and guide them, they fall through the cracks. In a region where 94% of new HIV infections occur among key populations and their partners, community-led support has been—and continues to be—essential.
“These services are not optional. They are the very foundation of an effective HIV response in a region where people are routinely excluded from healthcare due to criminalization, stigma, and discrimination,” said Vera Ilyenkova, UNAIDS Adviser on Key Populations and Community Engagement for the EECA region. “The process of building sustainable community-led services through national roadmaps and social contracting has only just begun. These fragile advances are now at serious risk.”
Ukraine, once a regional leader in transitioning from donor to domestic funding, has been forced to reverse course due to the war. The country has become heavily dependent on international assistance to sustain essential medical care, including HIV services. The US Government currently supports antiretroviral therapy (ART) for more than 117,000 HIV patients and pre-exposure prophylaxis (PrEP) for more than 13,000 people at high risk of HIV exposure in Ukraine. Although ART supply continuity has been confirmed, the wider impact of reduced funding is already being felt. '100 Percent Life'—the largest network of people living with HIV in the country—expects to lose a quarter of its workforce, and a critical situation has arisen regarding the availability of PrEP medications. The supply of antiretrovirals for PrEP, funded by the US Government, has been cancelled.
In Kazakhstan, the US Government supported peer-led services, HIV prevention programs, and professional training in two regions are now under threat. In Tajikistan, US funding enabled the expansion of HIV testing, access to PrEP, and essential services provided by civil society groups to communities that would otherwise remain invisible to the healthcare system.
Although Uzbekistan did not receive direct US Government funding for HIV-related programs, critical initiatives such as civic space development, education, and HIV advocacy were supported by US assistance. With these programs now closed, organizations working on HIV-related legal reforms, anti-discrimination efforts, and rights-based healthcare access are facing increased challenges in continuing their work and advocating for policy change.
The US funding cuts have also significantly impacted regional community networks and multi-country initiatives doing regional advocacy. Collective efforts in harm reduction, HIV decriminalization, and legal reform across EECA are now struggling to survive. Several organizations that have played pivotal roles in shaping inclusive, human rights-based responses to HIV are facing critical funding cuts and may be forced to shut down entirely by mid-2025.
“This is not just a financial crisis,” said Ganna Dovbakh from the Eurasian Harm Reduction Association. “It is a crisis of global values and priorities. Right now, the future of our dignity, health, and human rights is uncertain. Community organizations are the first responders in this crisis—yet they’re being forced to survive without oxygen, and preferably in silence.”
Emergency mitigation measures are underway, including the reprogramming of international funds and new partnerships—such as emergency support from the Deutsche AIDS Stiftung for grassroots organizations in Ukraine and Tajikistan—but these are stopgap solutions. They cannot replace long-term, strategic investment.
“We call on donors to ensure emergency support for these organizations; on governments to integrate and co-finance community services as part of national health strategies; and on international partners to continue pushing for inclusive, rights-based responses to HIV that leave no one behind,” said Eamonn Murphy, UNAIDS Regional Director for Asia Pacific and Eastern Europe and Central Asia.
Because without communities at the center, there is no response—and no hope of ending AIDS.
Region/country
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025


Feature Story
Impact of US funding cuts on HIV programmes in East and Southern Africa
31 March 2025
31 March 2025 31 March 2025UNAIDS’ Regional Support Team for East and Southern Africa (UNAIDS RST ESA) is releasing bi-monthly updates to track the impact of US funding cuts on the HIV response in East and Southern Africa. The report outlines key challenges as well as government and UN responses. The US Government supported 15 countries in the region including: Botswana, Eswatini, Ethiopia, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, South Sudan, Tanzania, Uganda, Zambia and Zimbabwe.
The recent cuts in US funding have had a seismic impact on HIV responses across East and Southern Africa. They have led to immediate disruptions in HIV prevention, treatment and care services. While a waiver was introduced to allow implementing partners to continue providing certain services, including lifesaving HIV treatment, it did not prevent widespread service gaps. The US funding cuts have already resulted in thousands of health workers being retrenched, programs halted, reduced access to HIV prevention, unavailability of data system and other related services and the dismantling of community health systems.
The results from one survey in a high-burden country in the region found that 62% of respondents reported difficulty accessing pre-exposure prophylaxis (PrEP), 46% of people living with HIV experienced disruptions in HIV treatment and 23% of people living with HIV received smaller amounts of antiretroviral medicines (for example less than three-month supply instead of the usual three to six-month supply) from local dispensaries.
Countries across the region are adapting to the cuts, with governments, civil society organizations, and international partners exploring ways to continue providing critical HIV services.
Key Impacts
HIV prevention services
US funding via the US President’s Emergency Plan for AIDS Relief (PEPFAR) contributed an estimated $301.6 million for HIV prevention across 15 countries in the region, making it the largest single funder. The US funding represents close to 45% of total HIV prevention funding among the 15 countries which have reported expenditures data. Several high-burden countries, including Malawi (88.5%), Zimbabwe (82.7%), and Mozambique (81.8%), are almost entirely dependent on PEPFAR for their HIV prevention programs while others like South Africa, Botswana, Kenya and Namibia are below 25%.
UNAIDS’ Country Offices in East and Southern Africa reported that primary HIV prevention services, such as condom distribution, pre-exposure prophylaxis (PrEP), Volunteer Medical Male Circumcisions (VMMC) and peer outreach conducted by community-led organizations have been deeply affected by US funding cuts. PrEP services are particularly impacted due to their heavy reliance on US funding. The DREAMS programme, which targeted 2 million adolescent girls and young women in 10 countries in the region has shut down. Similarly, programming for key populations, including HIV prevention programming, has not been prioritized.
Notable examples:
- In Malawi HIV prevention education and awareness campaigns and VMMC services have been suspended or reduced. Community-based HIV prevention and outreach programmes have been disrupted. Recent efforts to develop a national programme for people who use drugs have been affected. Programs for key populations have been significantly affected, with the closure of drop-in centers.
- The DREAMS programme in all 10 countries has halted. The programme was a PEPFAR initiative that served 2 million adolescent girls and young women in sub-Saharan Africa and focused on HIV prevention, sexual and reproductive health and rights, physical and sexual violence, education and empowerment.
HIV treatment and preventing vertical transmission of HIV
The US funding cuts have caused widespread fear and confusion about treatment availability, particularly among people living with HIV who access HIV related services in drop-in centers. Despite the waiver, services for pregnant women living with HIV have been affected, increasing the risk of vertical transmission during childbirth and breastfeeding.
Notable examples:
- In Kenya, some HIV treatment facilities are not yet operating optimally due to staffing challenges, which has resulted in unguided integration of HIV into outpatient services, posing a threat to patient privacy. Additionally, panic about treatment availability, particularly among young people living with HIV, has led to some young people living with HIV spacing, sharing and/or stockpiling antiretrovirals (ARVs).
- Zimbabwe has experienced disruptions in testing of pregnant women during prenatal care, early infant diagnosis, pediatric HIV treatment services and the sample transport system.
Health facility closures and disruptions in clinical services
Countries have reported closures of some sites delivering HIV treatment or other disruptions in clinical HIV services. Thousands of health workers have been retrenched leading to major service disruptions. In some cases, health workers without prior experience in HIV care have stepped in raising concerns about the quality of care.
Notable Example :
In Kenya approximately 41,000 doctors, nurses, technical and management staff and community workers were supported by the US government; in South Africa 15,000 health workers; in Mozambique more than 21,000 health workers.
- In Malawi 247 nurses, 3,513 community health workers, 206 technical and managerial staff and other 485 human resources reliant on US funding are facing contract terminations. Furthermore, HIV data management has been hugely affected; 20% of the 271 electronic medical record systems established at service sites were down during assessments in February.
- In Ethiopia, there is currently no plan by the government or partners to take in the human resource costs caused by the US funding cuts namely the jobs of 97 community adherence case managers, 194 support workers, eight pharmacy technicians and six laboratory technicians for HIV treatment services.
Community health systems
There is concern that community systems, including advocacy, service delivery, monitoring, and evidence gathering, are collapsing. In several instances, even where governments step in to fund treatment gaps, most resources are directed toward formal health systems, leaving community-based initiatives behind.
Notable examples:
- In Angola, all community outreach programmes supported by PEPFAR in four of the country’s 21 provinces have stopped.
- In Eswatini, many community-led or peer-led facilities and services, as well as services provided by local and international NGOs, have stopped functioning.
Key populations and human rights
US funding has been largely halted for projects and programmes focused on addressing stigma and discrimination and enabling legal environments. This often means that monitoring of human rights issues has stopped, intensifying fears of discrimination and human rights violations against people living with HIV and key populations and other vulnerable groups as they are forced to switch from tailored, community-supported services to government services for the general population. In resource-constrained regional settings, there is a risk that programming for key populations, including HIV prevention and care linkages, will not be prioritized.
- There are growing challenges to accessing HIV prevention and sexual and reproductive health rights services for adolescent girls and young women given the defunding of HIV prevention services including youth friendly services at community level.
- Across East and Southern Africa, funding for gender-based violence prevention and response programs are coming to a halt.
Research and trials
In South Africa, US government-supported research on the HIV vaccine and long-acting PrEP has come to a halt. A large tuberculosis (TB) research study was also stopped leading to fears of disruptions of TB service delivery, reductions in treatment adherence and increases in TB transmission and mortality. In Ethiopia, the US government supported Cab-La pilot has halted. Thisnew HIV prevention technology would especially benefit adolescent girls and young women who face inequalities that create barriers to accessing sexual and reproductive health services.
Government responses
Countries in the region are responding to the impact of the funding cuts on their HIV response. Many countries conducted UNAIDS-supported rapid surveys to assess the impact of the cuts on recipients of HIV services and have put in place short and long-term mitigation measures. Kenya and Rwanda are among the list of countries that have reported that domestic resources are being mobilized to maintain priority HIV programmes previously funded by the US. Countries have committed to ensuring continuity of treatment for people living with HIV and are discussing future budgetary allocations for antiretroviral treatment to ensure there are no disruptions in ARV medications.
Notable examples:
- Ethiopia’s parliament has introduced a new payroll tax as part of measures to fill the financial gap left by the USAID funding pause. The new bill has been forwarded to a parliamentary committee for deliberation. The funds collected will go to a new Ethiopian Disaster Risk Response Fund to pay for projects previously funded by USAID including HIV medication.
- In Lesotho, a task team has proposed mitigation measures based on a mapping of US-funded projects, including government payment of salaries for affected staff, task shifting, recalling of staff on leave, and integration of HIV services.
- Botswana and South Africa are among those countries working with organizations that have lost US funding to refer their clients to government facilities for essential services.
- Malawi's government is working with partners, including UNAIDS, to ensure the continuation of HIV services and plans to lead service delivery planning and management going forward, with partners supporting where gaps are identified.
Critical gaps
The recent US funding cuts have created critical gaps in the HIV response across East and Southern Africa. The gaps, unless filled, will have severe public health consequences, reversing the gains made thus far in the HIV response.
Key areas affected:
HIV prevention & treatment commodities: Reduced access to ART, HIV test kits, PrEP and condoms, increasing the risk of HIV transmission and HIV treatment interruptions.
Human resources for health: Workforce shortages due to salary cuts and hiring freezes which is putting a service delivery and patient care.
TB Ccmmodities: Limited availability of diagnostic tools and TB medications, delaying detection and treatment, which could lead to drug resistance.
Data monitoring & management systems: Weakened tracking of disease trends, leading to gaps in evidence-based HIV response planning.
Community systems: Closing of community-led health initiatives, outreach programs and peer support has disrupted community systems that are vital to the success of the HIV response.
UNAIDS response
- Monitoring and communication: UNAIDS regional team is actively monitoring the impact on the response in the region and supporting organization wide efforts to collect data and information on the impact in real time. The regional team is maintaining communication and collaboration with communities, networks and partners.
- Collaborative assessments: UNAIDS regional team has been supporting UNAIDS Country Offices as they work with governments to assess the impact of the HIV response and to put in short- and long-term mitigation measures.
Collaborations with communities: UNAIDS is collaborating with the Athena Network on assessing the impact of the funding cuts on girls and young women. UNAIDS is also working with the Global Network of People Living with HIV (GNP+) to develop a comprehensive survey to document the impact on community systems across the region.
- Collaboration with regional co-sponsors: UNAIDS, UNICEF and WHO are in discussions about the impact of the US funding cuts on supply chain constraints and collaborating on potential solutions for the region. UNAIDS and WHO are engaging with national AIDS commissions to assess the impact and discuss fundraising modalities to continue ongoing HIV related activities. Through the 2gether4SRHR program, collaborations between UNICEF, UNFPA, WHO and UNAIDS at both country and regional level are reviewing plans to be more responsive to the current crisis. Efforts are underway to collect data, identify effective integration models and establish a minimum HIV service package for humanitarian settings.
- Support for transitioning to national ownership: The UNAIDS regional team is working in collaboration with the SADC Secretariat and member states on the sustainability roadmaps. UNAIDS is working with UNAIDS Country Directors to advance HIV Sustainability Roadmap Part B with support from Gates Foundation and Global Fund in Namibia, Botswana, Malawi, Kenya, Zambia and Zimbabwe. UNAIDS also socialized UNAIDS Country Directors on the RAFT Tool, which helps countries assess PEPFAR investments and prioritize necessary actions to address these. The tool has been piloted in Uganda and Rwanda and is now being rolled out more broadly.


Feature Story
Impact of US funding cuts on HIV programmes in Latin America and the Caribbean
19 March 2025
19 March 2025 19 March 2025Current Situation
Prevention of HIV and other sexually transmitted infections among key populations in Latin America and the Caribbean is heavily reliant on US funding. Recent decisions by the United States Government indicate that efforts to support prevention among key populations will not receive funding resources. This has led to significant disruptions in and challenges for HIV services in the region.
Immediate risks and disruptions
- Humanitarian assistance: Transnational projects aimed at migrant populations have been suspended. Despite a waiver announced on February 1 allowing continued provision of some HIV services, resumption of humanitarian services has been hindered due to the absence of PEPFAR and USAID staff.
- Service delivery: The suspension of US funding has affected the delivery of various HIV services, including those provided by civil society organizations, government entities, and United Nations agencies. NGOs are particularly vulnerable to the US funding cuts.
- Impact on key populations: The US funding cuts have led to stress, depression, anxiety, and uncertainty among people living with HIV and key populations. There is a significant concern about the risk of being left without antiretroviral treatment, access to PrEP, and other essential services.
- Funds allocated for non-contingency humanitarian assistance were primarily focused on the humanitarian crises in Haiti and Venezuela, Colombia's post-conflict challenges, and the Northern Triangle crisis (Guatemala, Honduras, El Salvador). Although these funds were not intended for a direct response to HIV, their absence deepens the structural vulnerability of migrant and other vulnerable populations—including people affected by conflict in Colombia—and puts them at risk of exploitation, human trafficking and survival sex, all of which increase vulnerability to HIV.
Politically relevant updates
- Emergence of extreme positions: In many countries in the region, outbursts of homophobia, transphobia and discrimination against people living with HIV have intensified. Many parliamentarians in the region have taken advantage of the situation to gain political leverage by attacking key populations.
- Media Representation: Actions targeting societal enablers are being shown in the media as examples of waste of money and corruption.
Civil society impact and resilience:
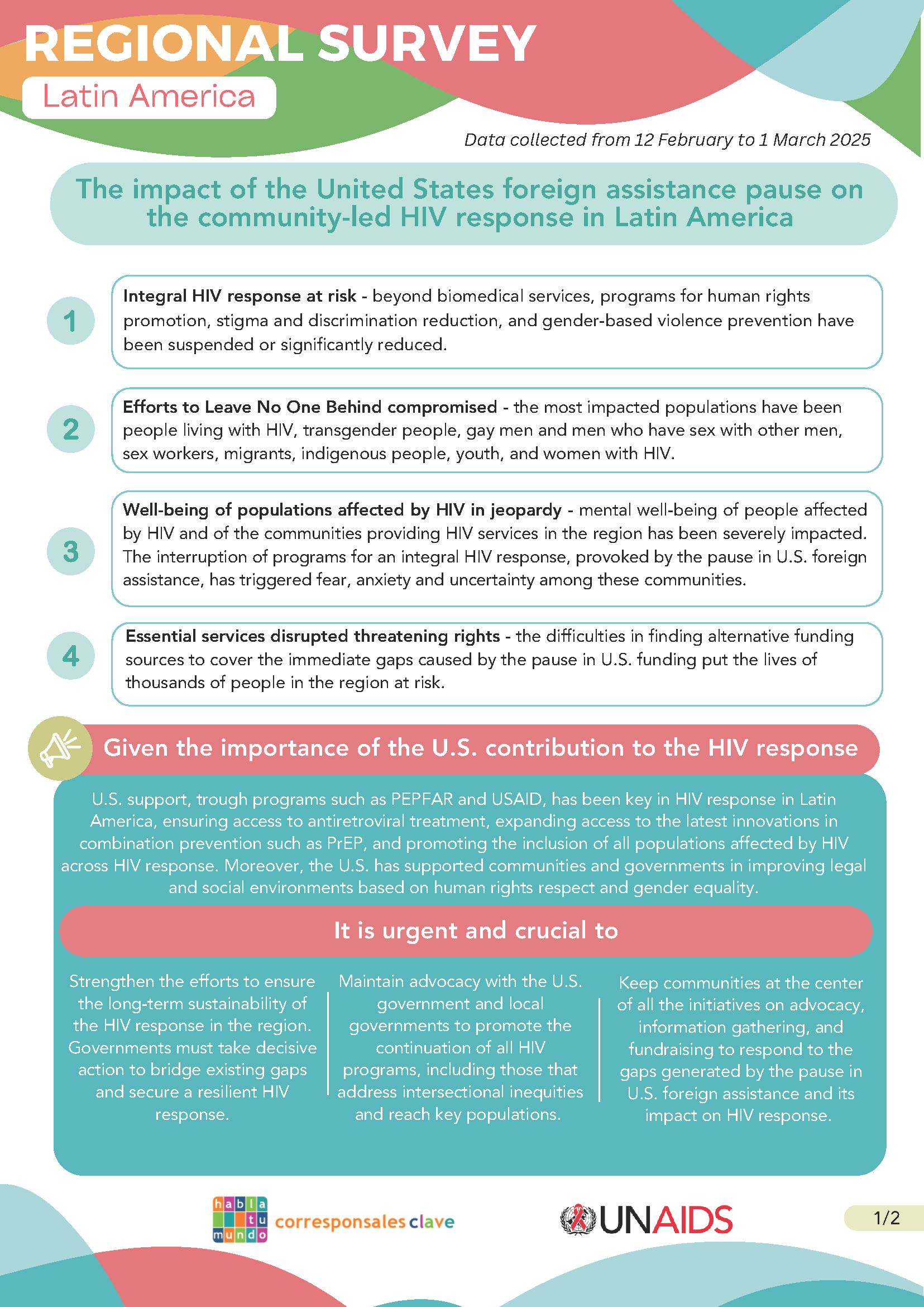
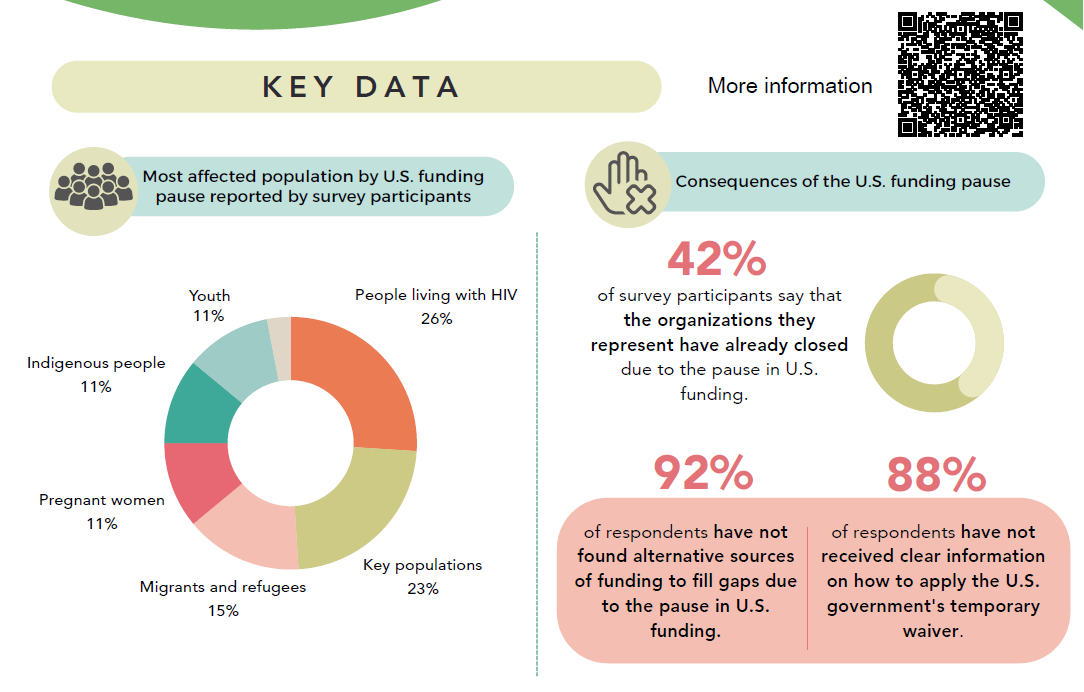
- Survey Findings: A survey conducted by the civil society organization "Corresponsales Clave" (Key Correspondents) with 49 organizations from various countries in the region revealed that US funding cuts have led to significant disruption of services for key populations and emotional distress among people living with HIV and key populations.
- Community Response: Despite the challenges, civil society organizations and community leaders are working to ensure the sustainability of the HIV response by optimizing health services.
- UN Response: The offices of the UN Resident Coordinators are intensifying the search for non-traditional donors and making bilateral approaches with embassies to identify funding opportunities. UNAIDS and PAHO are working together to deliver technical assistance to optimize health services in three areas: integration of HIV services in primary health care, optimization of service delivery models, and facilitation of community response to HIV.
- UNAIDS is carrying out joint analyses with the Global Fund to align the resources of national grants destined to the strengthening and resilience of health e-services with the principles mentioned above.
Additional Insights
- Regional Progress: The Caribbean has made substantial progress against HIV since 2010, with a 22% decrease in new HIV infections and a 57% decrease in AIDS-related deaths. Latin America is the most autonomous region of the Global South in terms of national funding for HIV treatment, but there are still major gaps in prevention and social enablers. Therefore, continued funding is a necessary strategy for a smooth transition towards full sustainability of the HIV response in the region.
- Funding Challenges: The critical impact of the US funding cuts has exacerbated existing challenges in the HIV response across Latin America and the Caribbean.
Related resources
Related

Feature Story
The impact of the United States foreign assistance pause on the community-led HIV response in Latin America
03 March 2025
03 March 2025 03 March 2025



Feature Story
The critical impact of the PEPFAR funding freeze for HIV across Latin America and the Caribbean
19 February 2025
19 February 2025 19 February 2025The U.S. decision in January to freeze all funding for U.S. foreign assistance, including for the U.S. President's Emergency Plan for AIDS Relief (PEPFAR), has had a critical impact on several countries in Latin America and the Caribbean, exacerbating existing challenges in the HIV response. More than 20 countries in the region rely on these funds to deliver HIV treatment, prevention, and care services, including community-led services focused on the most discriminated and marginalized communities.
Following the decision to freeze all U.S. funding for foreign assistance, the U.S. Government issued a waiver allowing some funding to support lifesaving services. However, confusion about which services may be supported and a lack of support for some services means the situation remains critical, posing a serious risk of setbacks in the AIDS response in the region. While some key treatment services and prevention of vertical transmission have been gradually coming back into operation, most countries have been facing disruptions in their HIV treatment programs.
The lack of funding has led to a significant decrease in community-led HIV prevention efforts, a reduction in treatment adherence, counseling, and social support and monitoring activities. Consequently, there are increased risks of new HIV infections, of higher mortality rates, and a deterioration in the quality of care for people living with HIV, directly impacting their capacity to access treatment and to achieve viral suppression – crucial steps towards the global target of eliminating AIDS as a public health challenge by 2030.
In Colombia and Peru, the freeze has severely affected migrants and refugees, who are estimated to have an HIV prevalence two times higher than the general population. Approximately 4,000 migrants and refugees are receiving antiretroviral treatment (ART) in Colombia thanks to the government efforts and cooperation funds, but the withdrawal of such resources is directly impacting this vulnerable group and the country's capacity to include them in the health system. One community-led organization supporting HIV services among migrant and LGBT communities had to end contracts for 40 out of 70 team members, significantly reducing their capacity to provide essential services to reach such populations.
In the Dominican Republic, even though the government guarantees access to antiretroviral treatment, the pause in PEPFAR funding has left thousands without access to essential HIV services. PEPFAR supports around a third of HIV care services, including PrEP services, health human resources, and laboratory networks. The reduction in community assistance has made it difficult for people to access their medications, especially those who live far from care. The quality of services offered by the Comprehensive Care Services (known by the acronym SAI in Spanish) in the Dominican Republic has been highly compromised, with many staff and services entirely dependent on PEPFAR funds.
El Salvador has also been impacted, with PEPFAR projects supporting comprehensive HIV care clinics now suspended. This has caused a slowdown in care, and the opportunity for new diagnoses and early initiations of antiretroviral treatment is likely lost.
In Guatemala, the HIV epidemic is mainly concentrated among key populations such as transgender individuals, gay men and other men who have sex with men, and sex workers. The distribution of PrEP for these groups has been severely disrupted, with many organizations that rely on U.S. Government funding suspending their work. The reduction of personnel, including medical staff as well as outreach workers that were funded through PEPFAR has resulted in people being unable to access HIV prevention and treatment services.
Haiti has seen a significant impact on its HIV response, with PEPFAR covering around 60% of the national response. The stop-to-work order has thrown the response into disarray, causing anxiety for the 127,000 Haitians living with HIV who are on treatment. In the context of the humanitarian crisis and gang violence, more than 1 million people are now internally displaced in Haiti, many of them displaced multiple times– among them women, girls and children. Escalating violence has also led to the closure of 39% of health facilities, including two of the capital’s three major hospitals. Access to healthcare has never been more limited. The quality-of-service delivery of medicines has also been affected, with approximately 5,000 health workers receiving directives to stop working.
In Jamaica, 70% of HIV resources come from external sources – with PEPFAR covering around 50% of services. The pause in funding has raised concerns about the delivery of HIV prevention services for at risk populations delivered via civil society organizations. Civil society groups have reported that their institutional stability and survival are at risk, with many unable to guarantee the continuous employment of their field staff in charge of liaising with the most discriminated and affected populations who need HIV services.
In Panama, the suspension of a study on recent HIV diagnoses and the halt in laboratory sample transportation have further limited essential diagnostic and monitoring services. The country had already been facing significant disruptions, particularly among the indigenous Ngäbe-Buglé population, who are expected to face increased obstacles to accessing HIV services. In 2023, despite representing only 5% of Panama's population, the territory, which is home to approximately 225,000 residents, accounted for 30% of the nation's AIDS-related deaths among individuals aged 29 or younger, as reported by the Panama Ministry of Health.
In Brazil, on the other hand, the Unified Health System (SUS) guarantees uninterrupted universal and free access to health services, including HIV diagnosis, treatment and prevention for all people living in Brazil. The “A hora é agora” project, carried out in five capital cities with PEPFAR resources, worked to provide specific services such as doctors, reception and delivery of antiretroviral drugs and PrEP in addition to public health services, so the national response to HIV was not impacted by the cut in resources.
Latin America is one of the three regions in the world where new HIV infections have increased since 2010, with a rise of 9%, which highlights the urgency of addressing these disruptions. The Caribbean region has made significant progress in reducing new HIV infections and increasing access to treatment. Still, the freeze on PEPFAR funds threatens to reverse these gains and the ongoing process of creating sustainability roadmaps to increase national funding for the HIV response.
UNAIDS continues to work with various partners to help mitigate the impact and find the best solutions and calls for the continuity of all essential HIV services in the region.
"United States support through PEPFAR has been a cornerstone of the HIV response in our region, including a key driver for strengthening the sustainability and resilience of national responses. The recent humanitarian waiver reflects the commitment of the American people to save lives and maintain momentum to end AIDS by 2030," says Luisa Cabal, UNAIDS Regional Director for Latin America and the Caribbean. "UNAIDS will continue to convene communities, civil society organizations, governments, and partners to advocate for continued support and critical HIV services supported by PEPFAR. It is also time for the governments of the region to play a leadership role in guaranteeing the right to health of their most marginalized populations."