

Feature Story
Sevilla Declaration on the centrality of affected communities in urban HIV responses unveiled at Fast-Track Cities 2022 conference
11 October 2022
11 October 2022 11 October 2022At a Fast-Track Cities 2022 conference reception held today in Seville, Spain, several Mayors and a Deputy Governor in attendance were joined virtually by peers from across the Fast-Track Cities network to sign their names to a declaration aimed at defining and facilitating the placement of affected communities at the center or urban HIV responses.
- The Mayors of Blantyre (Wild Ndipo), Kingston (Delroy Williams), Libreville (Issa Malam Salatou), Quezon City (Ma. Josefina Belmonte), and Sevilla (Antonio Muñoz Martínez) signed the Sevilla Declaration on the Centrality of Affected Communities in Urban HIV Responses (Sevilla Declaration) along with Johannesburg Mayor (Dada Morero), New York City Mayor Eric Adams, and other Mayors who participated via video or virtually.
- The Deputy Governor of the Bangkok Metropolitan Administration (Dr. Tavida Kamolvej) also affixed her signature to the declaration during the Sevilla ceremony, and a representative from GGD Amsterdam signed on behalf of that city’s Mayor (Femke Halsema). Multiple county and provincial officials from Fast-Track Cities in other countries also signed the declaration via video or virtually.
- Moreover, Mayors and representatives from an additional 22 Fast-Track Cities in Spain signed the declaration. Of note, the reception’s signing ceremony was witnessed by Carolina Darias, Minister of Health of Spain, in whose country more than 150 cities have joined the Fast-Track Cities network, with Sevilla having been the first Spanish city to sign the Paris Declaration on Fast-Track Cities Ending the HIV Epidemic in 2015.
According to Dr. José M. Zuniga, President/CEO of the International Association of Providers of AIDS Care and the Fast-Track Cities Institute, the Sevilla Declaration will supplement the Paris Declaration on Fast-Track Cities, which more than 400 cities and municipalities worldwide have signed since the network’s launch in 2014, thus joining the Fast-Track Cities network. The new declaration includes 10 commitments Fast-Track Cities are asked to make that range from safeguarding the dignity and rights of communities affected by HIV to meeting the United Nations goals for community-led HIV responses.
“An amorphous and overly malleable term such as ‘placing people at the center’ of the HIV response has little effect if it can be interpreted in a million different ways or worse actioned as mere tokenism that disenfranchises those whose voice at the table and leadership are critically needed,” said Dr. Zuniga. “The 10 commitments that Fast-Track Cities are making in signing the Sevilla Declaration reflect an important step forward in clearly defining, operationalizing, and facilitating what we mean by ‘placing people at the center’ of urban HIV responses at a time when it is most critical to do so.”
The Sevilla Declaration was shaped by organizations representing people living with HIV, including the Global Network of People Living with HIV (GNP+), as well as through regional listening sessions involving local communities of people living with HIV across the Fast-Track Cities network. Also providing input were the four core partners of the Fast-Track Cities initiative: IAPAC, the Joint United Nations Programme on HIV/AIDS (UNAIDS), United Nations Human Settlements Programme (UN-Habitat), and the City of Paris.
“The Sevilla Declaration provides structure for communities of people living with HIV to more formally play a leadership role in HIV responses at city and municipal levels,” said Sbongile Nkosi, Co-Executive Director of GNP+, which formally endorsed the declaration at the Fast-Track Cities 2022 conference. “We talk a lot about ‘placing people at the center of the HIV response,’ but the Sevilla Declaration does more by articulating commitments local governments and institutions must make to create the space for and empower people living with HIV and their community-based organizations to lead urban HIV responses.”
In its Global AIDS Strategy, 2021-2026, UNAIDS emphasizes the critical nature of community engagement and leadership to regain momentum against HIV that was lost during the COVID-19 pandemic. Through its advocacy on community engagement, UNAIDS has consistently stressed that the call for “nothing for us without us” must be made more than just a slogan.
“In line with the Global AIDS Strategy and the Sevilla Declaration, empowering and integrating community engagement is the cornerstone to ending AIDS and having people at the center of the response, said UNAIDS Deputy Executive Director for Programme, Eamonn Murphy.
Additional information from our partner
Related




Feature Story
Communities at the centre of an orchestrated emergency response to monkeypox in Peru
10 October 2022
10 October 2022 10 October 2022"My name is Jonathan. Today I'm not going to tell you how I got monkeypox, but how complicated it is to carry this disease", says the activist and crossdresser Jonathan Albinagorta. He is also known as Samantha Braxton, one of the influencers supporting the Ministry of Health in its video campaigning on monkeypox prevention in Peru.
With more than 2300 confirmed cases of Monkeypox by the end of September, Peru had the world's highest infection rate per million people, according to Our World in Data, a collaborative online platform led by researchers at the University of Oxford.
The response to the outbreak in Peru was set up under the leadership of the national HIV strategy team, which developed a plan to raise awareness of the disease. Its public real-time data dashboard, inspired by the COVID-19 response, provided concrete evidence for the rapid of an awareness campaign. However, the same data, mainly from HIV-specialized centres, also had the unwelcome side-effect of increasing stigma and discrimination for some groups of people.
"The data created a biased sample at the beginning. Evidence showed that people living with HIV and some key populations, such as gay men, were among the most affected in Peru", recalls Andrea Boccardi, UNAIDS director for Peru, Bolivia, Ecuador and Colombia. "But these are the very people who have the culture of going to the HIV-friendly services for consultations, for periodical examinations and HIV treatment."
Referral Centers for Sexually Transmitted Infections, known as Cerits, and Periodic Health Care Units provide HIV services for Peru's most vulnerable and key populations. "These groups of people do not go to hospitals where they tend to suffer discrimination. They go to these centres, where the greatest number of monkeypox diagnoses came from at first", explains Boccardi.
Experience in dealing with the HIV pandemic shows that data must be accompanied by adequate information-sharing to the public and impacted groups in a non-stigmatizing way. An inclusive approach and the correct use of language are key to engage with communities so that they become an integral part of the response instead of being driven away.
UNAIDS supported the country in quickly setting up a strategy that included meetings between health officials and civil society representatives. Community leaders also contributed by reviewing messages coming out of the ministry of health. People also received training to act as spokespeople in media interviews.
“Often, the communication from the ministry of health ends up being very institutional or quite distant. Something that the community cannot fully digest”, says Mauricio Guitierrez, a GayLatino network activist. “We elaborated friendly visual materials for dissemination. It is important to translate and personalize the information for people and that was what we tried to do by supporting the ministry in these campaigns.”
”As well as informing and clinically diagnosing the most at-risk populations in saunas, hotels, and other sites, monkeypox working group convinced mayors to keep these establishments open and to use them as critical platforms for the dissemination of relevant information on monkeypox directing people to the information and services made available.”
In Peru, LGBTIQ+ people and people living with HIV are the most discriminated against, with 71% and 70% of them, respectively, reporting to have suffered discrimination at some level, according to the National Human Rights Survey released in 2021 by the Ministry of Justice and Ipsos Peru.
“Out of fear of stigma and of what people will say, a lot of us don’t ask and fall into the same trap of ignorance”, says Albinagorta. “It was great that the Ministry placed QR codes in LGBT establishments, for example.”
Alliances with telecom companies and social networking apps, such as Grindr, created opportunities to inform the most vulnerable populations through an estimated 40 million messages focused on monkeypox prevention and treatment. Former COVID-19 spaces were also used for the 21-day isolation period for people not able to comply with thisrequirement, including migrants and refugees.
Despite some early signs of stabilization, the Pan American Health Organization (PAHO) said recently that it is too early to proclaim victory. It called on countries "to intensify the response actions, prioritizing detection, surveillance and community engagement to reduce new cases and put an end to the outbreak in the region." The United States still accounts for more than half of cases, but rapid increases have been witnessed in Brazil, Peru, Colombia, Mexico and Chile in the past month.
The Ministry of Health of Peru is purchasing vaccines through the PAHO Strategic Fund, but the total number of vaccines available for the entire region is 100 000. The main challenges are the criteria for prioritization as the expected number of vaccines per country will be no more of 5000.
"Many people contacted me after my first video for the ministry of health in Peru. For those who are suspicious, it inspires more confidence to approach someone like me, who has had monkeypox and talks freely about it, than to go to a hospital, an institution or the ministry itself, " says Samantha. "Of course, there are also haters. Some people believe that when a gay man shares that he has had monkeypox, he is stigmatizing himself. But that's not it.”
Region/country




Feature Story
Indonesia: Helping one family at a time through Lentera Anak Pelangi’s One Child One life program
10 October 2022
10 October 2022 10 October 2022Estimates indicate that in Indonesia in 2021, only 25% of the 19,000 children living with HIV received life-saving antiretroviral therapy and 2,400 children died from AIDS-related causes.
Despite global scientific breakthroughs providing more effective treatment for adults and children, for many children living with HIV in Indonesia access to antiretroviral therapy remains elusive. Exacerbating the situation is the entrenched societal and gender inequalities that present barriers to women, adolescents and children to access quality prevention and care services.
With many competing priorities, national and local commitment of resources to scale-up efforts to eliminate vertical transmission of HIV and increase ARV coverage among children living with HIV remain limited. This has resulted in insufficient investment in community-based services for women, adolescents and children living with HIV.
To reduce AIDS-related deaths among children, and ensure children and adolescents living with HIV have access to high quality comprehensive care and support, Indonesia must expand community-based services and community-led programmes tailored to the needs of these very vulnerable yet often left-out groups.
Lentara Anak Pelangi (LAP), an organization that provides HIV services, including psychosocial support, for children and adolescents living with HIV in Jakarta has seen some successes through their One Child One Life program.
“We want these adolescents to be the next generation of positive leaders and influencers who inspire other teens living with HIV” said Prof. Irwanto, founder of Lentera Anak Pelangi.
The One Child One Life program provides disclosure and post-disclosure support, mental health assessment and care as well as education.
“Lentera Anak Pelangi has supported my daughter since she was very young. LAP’s in-person and online activities have been very helpful for her. Through Sekolah LAP, my daughter has started to learn how to build her self-confidence and open her mind to learn more things. I also learned the meaning of this illness and find friends facing the same struggle and fight to continue to be healthy,” Explained the mother of one LAP beneficiary.
“My son and I have been greatly helped by LAP’s education support. During the pandemic, we often received sembako (staple foods). My son loves to be part of LAP because he gets to meets other teens who share similar circumstances. We also receive information on how to provide care for our family,” another mother said.
Through the One Child One Life program, children living with HIV have been supported to suppress their HIV viral load, return to school and participate in youth support groups. LAP also supports children with special needs and supplemental nutritional support when required. However, their coverage remains small due to funding and human resource constraints.
“Science has made it possible to diagnose and treat HIV. We have come a really long way in 40 years. In Indonesia, we must eliminate vertical transmission of HIV and ensure that all children living with HIV access life-saving antiretroviral therapy and quality care including psychosocial support when needed.” said Krittayawan Boonto, the UNAIDS Country Director for Indonesia.”
UNAIDS Indonesia together with Lentera Anak Pelangi and other implementing partners continue to call for optimized investments in community-based services and community-led programmes for women, adolescents and children living with HIV.
Region/country




Feature Story
PrEParing for the next chapter of HIV prevention in Myanmar
19 September 2022
19 September 2022 19 September 2022Two young men are sitting on a couch scrolling on their phones when May Oo, a famous makeup artist and lesbian, gay, bisexual, transgender, and queer (LGBTQ) activist in Myanmar, joins them wearing a face mask and carrying a bag of drinks. He announces that a friend who works at an HIV clinic in Yangon told him that pre-exposure prophylaxis, or PrEP, is now available in Myanmar. As one friend is unaware of PrEP, May Oo shares his knowledge, also informing anyone else wo would like to listen in.
This scene, from a video shared on the Facebook pages of implementing partners of the USAID HIV/AIDS Flagship (UHF) Project, is one of several to raise awareness and demand PrEP as a prevention tool for men who have sex with men and transgender women in Myanmar. In these videos by celebrated members of the LGBTQ community and other educational posts, questions covered include what PrEP is, why it should be taken, and where to get it. As May Oo’s friend in the video puts it, ‘PrEP is a drug that can prevent HIV.’
Since 2016, PrEP has been included as a priority intervention in Myanmar’s National Strategic Plan on HIV/AIDS following recommendation by the World Health Organization that it be used as an essential part of HIV prevention services. It was also an objective of the UHF Project to introduce PrEP in Myanmar and integrate it into existing HIV services, since the project’s inception in August 2017.
The UHF Project, overseen by UNAIDS Myanmar and the non-governmental organisation Community Partners International, aims to develop, implement, and scale up innovative, cost-effective approaches to the HIV care cascade in Myanmar. As one of the innovative HIV prevention activities under the National Strategic Plan IV (2020-2025), the initial 18-month PrEP demonstration project began in July 2020 at three clinics in Yangon for men who have sex with men and transgender people.
Along with the pilot was a plan to expand the project for people who inject drugs in Kachin State since the UHF Project’s overarching goal is to foster interventions such as PrEP for Myanmar’s four key populations at highest risk for HIV—people who inject drugs, men who have sex with men, transgender people, and female sex workers in the five states and regions with the highest burden of HIV—Kachin and Shan States and Mandalay, Sagaing, and Yangon.
Formative assessments conducted prior to the inception of these PrEP services indicated that PrEP awareness in Myanmar was very low. Fewer than a quarter of focus group participants—comprised of men who have sex with men, transgender women, and people who inject drugs—had heard of PrEP prior to the assessment. Service providers interviewed as part of the assessments also described low PrEP awareness among their clients.
Once educated about PrEP, however, most study participants agreed that PrEP would benefit their communities and that people at risk would be interested and willing to take PrEP. Awareness raising and community education have been one of the UHF Project’s focuses to increase PrEP uptake in Myanmar.
That is where videos such as May Oo’s are important. By using celebrities, private chat groups, and informational posts alongside interactive follow up by service providers for recruitment of PrEP clients, implementing partners not only educate people at risk for HIV on PrEP as a prevention option but also address the stigma around it.
Respondents to a midterm analysis conducted one year into the PrEP project reported that Facebook was the primary source of PrEP information and education, as the potentially more effective approach of fully-fledged in-person outreach is not feasible in the country’s current situation.
‘There are many in rural areas who do not have access to or use social media platforms,’ reports Ma Shin Thant, a PrEP client and activist currently based in Mandalay for her work with transgender women. As PrEP is currently only available in Yangon, Ma Shin Thant is fortunate that she can afford access to required testing and PrEP delivery in Mandalay.
‘The next chapter of PrEP in Myanmar calls for greater political commitment, more resources, a decentralised and simplified delivery system, and innovative community-centred approaches to ensure access by populations who need PrEP,’ concurs Rangaiyan Gurumurthy, UNAIDS Myanmar Country Director. ‘Moving from the demonstration phase to reaching scale with epidemic impact is now necessary.’
Region/country


Feature Story
Nigeria calls for a successful 7th Global Fund Replenishment
12 September 2022
12 September 2022 12 September 2022Nigeria has hosted a meeting of key stakeholders in the country’s HIV and wider health response to call for a successful 7th Global Fund Replenishment meeting. The meeting took place in Abuja and included ambassadors of key donor and recipient countries and heads of United Nations agencies, including UNAIDS.
During the event, the Minister of State for Health, Ekumankama Joseph Nkama, expressed his appreciation for Nigeria’s partnership with the Global Fund to Fight AIDS, tuberculosis and malaria. He said Nigeria included one of the Global Fund’s most important recipients of Global Fund disbursements over the last 20 years and reiterated Nigeria’s commitment to increase domestic funding for health.
‘I applaud countries who have already made their pledges to the Global Fund including the United States, Germany, Japan and Luxemburg,” said Mr Nkama.” I encourage other countries to rise up to this noble call by increasing their pledge by at least 30% to enable the Global Fund to meet its target.” he concluded.
David Green, the United States chargé d’affaires commended the partnership with the Nigeria that had he said enabled an incredible acceleration of HIV treatment coverage, registering the largest treatment growth in the history of the HIV programme, despite the COVID 19 pandemic. This was made possible through national surge and alignment efforts that saw the aligning of technical and financial resources behind a single national programme for intensified case-finding, allowing rapid expansion of access to antiretroviral treatment.
‘Sustaining this success depends upon contributions to the Global Fund and all of us standing in solidarity to fight for what counts. We are close to the finish line, but with Nigeria still accounting for one out of seven children born globally with HIV, the race is not yet over,’ said Mr Green.
For the Global Fund, Linda Mafu, highlighted the importance of Nigeria.
“Nigeria is one of our most important portfolios at the Global Fund and achievement of our ambitious targets is critical both for the health of the people of Nigeria and the ability of the Fund to raise additional funding and make an impact at the global level in saving lives,” she said.
Leo Zekeng, UNAIDS country director reiterated the importance of the Global Fund in the collective global response to end AIDS as a public health threat by 2030 and called on countries to stand in solidarity for a successful 7th Global Fund Replenishment. ‘Investing in global health is not only the right thing to do but the smart thing to do as it guarantees a good return of investment. Every $1 invested in fighting AIDS, TB and malaria yields $31 in health and economic returns,” he added.
The Global Fund investment case of the 7th Replenishment conference was presented to those attending the meeting, highlighting the achievements of the investments and the remaining gaps in reducing the burden of HIV, tuberculosis and malaria. The 7th Global Fund Replenishment conference seeks to raise at least US$ 18 billion to save 20 million lives, reduce deaths associated with HIV, TB and Malaria by 65% and strengthen systems for health to build a healthier, more equitable world.
Region/country


Feature Story
People living with HIV speak loudly and clearly at World Council of Churches Assembly
07 September 2022
07 September 2022 07 September 2022The 11th Assembly of the World Council of Churches (WCC) is meeting in Karlsruhe, Germany, from August 31 to September 8, 2022. The WCC brings together delegates and participants from 345 denominations from around the world, representing more than 500 million Christians.
Faith leaders and activists living with HIV expressed huge concerns for the future of the HIV response. Young people continue to be exposed to HIV; women are experiencing violence in all forms. Governments are moving away from HIV and many ecumenical organizations too.
What we need is a continued engagement with people with HIV and those at risk.
My country depends on international aid, what if we stop having that support?”, said one faith leader.
Another said, “Adolescents and children are not staying on medication, they are getting sick and some of them are dying”. Time is running out for the HIV response, we have to help people to live and stay safe and healthy.
People with HIV in the WCC Assembly are speakers and are leading plenaries, workshops and ecumenical conversations. They are bringing attention to the role of the church and the ecumenical movement to continue responding to the HIV epidemic; not only in relation to HIV stigma, but also in advocacy for a sustainable response to HIV, gender justice, human sexuality and the work on HIV related intersectionality and inequalities. This is a matter of justice, love and reconciliation.
The third thematic plenary Affirming the wholeness of life, included input from Canon Gideon Byamugisha from Uganda. He spoke about the realities of young people exposed to HIV and the consequences of unequal access to COVID-19 vaccines, because of unfair patent systems. He shared his experience of receiving support from Bishop Samuel Ssekkadde in 1998 who was leading the Anglican Church in Uganda and how that support saved his life when he was about to die without access to HIV medications. For many people with HIV, that continues to be a reality today.
Canon Gideon Byamugisha is one of the founders of INERELA+ (International Network of Religious Leaders Openly Living or Affected by HIV). He asked the Assembly participants to adopt the targets of the Global AIDS Strategy: the 95-95-95 strategy, which means that 95% of people living with HIV should be tested, 95% of those, should be on treatment and 95% of those, should have undetectable viral load, meaning that they can no longer transmit HIV and can stay healthy.
On September 2, five faith leaders openly living with HIV shared local experiences of churches responding to HIV stigma. In Argentina, some churches are taking care of transgender, indigenous women living with HIV; in Ghana, other churches are promoting the message of undetectable HIV = untransmitable HIV. In the United States, faith based organizations are providing affordable housing for people living with HIV who are transitioning out from rehabilitation or from the penitentiary system. Churches in Kenya are caring for children orphaned by HIV and they provide care and accompaniment for women who experienced sexual violence.
The workshop presented the results of a six-month case study recently completed by the WCC and Emory University. “We emphasize stigma because we know that it is a major driver of the HIV epidemic,” said Dr. David Barstow, one of the workshop organizers. “And we emphasize the role of local churches because of the influence they have on their members and on the rest of society. Local churches, indeed local communities of all faith traditions, are key to eliminating stigma and are therefore key to ending the epidemic.”
Some of the preliminary findings of the study refer to the role of people living with HIV who have a deeper understanding of stigma because of their lived experience. According to Professor John Blevins, who led the case study team, “…in the case study, when people living with HIV talk about stigma, they describe complexities that are often not apparent to people who do not live with HIV”
One faith leader said that “…despite my congregation’s commitment to stigma reduction, many people with HIV still feel uncomfortable disclosing our status.” The stigma was perceived as something that comes from those “on top” in the church. Another faith leader said, “Every time one of them dies, I die a little bit myself.”
The church and faith communities have much work to do in relation to HIV stigma. “We should be part of the healing hands of God to the world,” said Gracia Violeta Ross, a woman openly living with HIV, who is now leading the Ecumenical HIV & AIDS Initiatives and Advocacy in WCC. Canon Gideon Byamugisha said “…zero percent of our members should feel stigmatized. Surely, we want that going to church should be good for your health!”
Our work

Feature Story
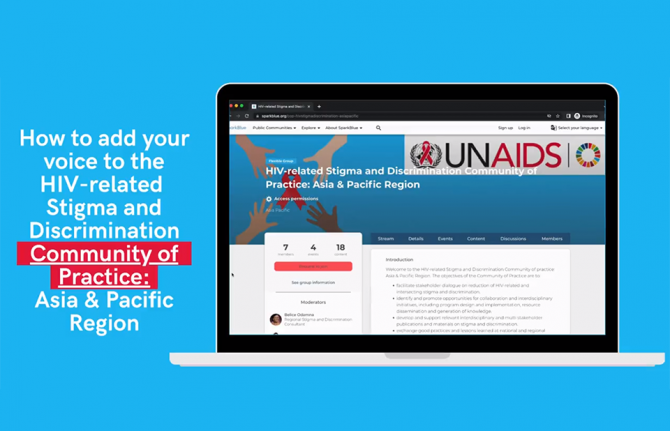
UNAIDS launches new platform on ending HIV-related stigma and discrimination in the Asia and Pacific region
07 September 2022
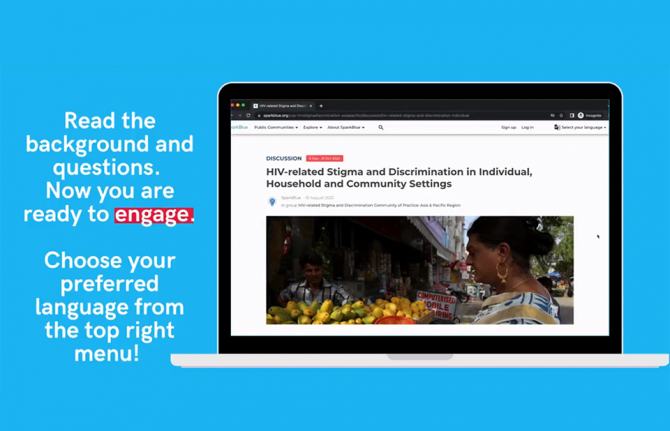
07 September 2022 07 September 2022Despite decades of advances in prevention and treatment, stigma and discrimination towards people living with HIV and key populations are a persistent barrier to addressing the epidemic. To encourage innovative approaches to address HIV-related stigma and discrimination in the region, UNAIDS has launched a new tool: the HIV-Related Stigma and Discrimination Community of Practice: Asia and Pacific Region.
HIV-related stigma and discrimination significantly impacts the health, lives and well-being of people living with or at risk of HIV, especially key populations. The Global AIDS Strategy 2021-2026 has prioritized the realization of human rights and elimination of stigma and discrimination by including new global targets that UN Member States have committed to as part of the 2021 Political Declaration. Yet, people living with HIV and key populations continue to face unfair treatment, rejection, abuse and even violence in various settings, including in their communities, healthcare, workplace, justice and education systems.
In Asia and the Pacific, which is the world’s most populous region, there were 6 million people living with HIV in 2021 and 86% of people living with HIV knew their status. Furthermore, amongst young people almost all new HIV infections are among key populations (gay men and other men who have sex with men, transgender people, sex workers, people who use drugs) and their sex partners who face many barriers in accessing HIV prevention and treatment services.
The online community of practice platform will capture and disseminate knowledge, experiences and innovative ideas and approaches to inform programming to reduce stigma and discrimination across the region.
“Relevant stakeholders working in the HIV response in Asia and the Pacific region are welcome to join the interactive platform and engage on the issues,” said Taoufik Bakkali, UNAIDS Regional Director for Asia and the Pacific. “Academics and researchers, communities of people living with or affected by HIV and of key populations, representatives of government ministries and other relevant government agencies, and civil society groups working on the HIV response are all encouraged to join and shape the conversation.”
The initiative is expected to foster south-south stakeholder dialogue and collaboration on interdisciplinary initiatives on programme design and implementation, the development and knowledge management of HIV-related stigma and discrimination and the creation of opportunities for peer learning and exchange of good practices and lessons learned.
“This platform provides an opportunity for all stakeholders to engage and shape responses to HIV-related stigma and discrimination while engaging communities in the process,” noted Harry Prabowo, the APN+ Program Manager. “This is an opportunity to link the science and evidence to innovative programming.”
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa




Feature Story
Justice is never given, it is won: How Eastern Caribbean activists developed the successful strategy to defeat the laws which criminalised LGBT people.
31 August 2022
31 August 2022 31 August 2022For almost 150 years, to be gay in St. Kitts and Nevis was to be criminalised. What the colonial authorities inhumanely labelled “the abominable crime of buggery” has been part of law, with the effect of punishing, stigmatising, discriminating against and excluding LGBT people for who they are.
This week the Caribbean nation’s High Court ruled that provisions which criminalize private sexual acts between same-sex partners were unconstitutional; that criminalisation became, immediately, null and void.
Attorney Nadia Chiesa noted that the St. Kitts and Nevis case set out several constitutional rights contravened by the criminal provisions: the rights to privacy, personal liberty, freedom from discrimination and freedom of expression.
“The evidence dealt not just with the legal arguments, but the myriad of ways in which the continued existence of these laws affects persons in the community in all of aspects of their lives,” Ms. Chiesa explained.
The claimants’ evidence spoke to issues commonly affecting members of the LGBT community in St. Kitts and Nevis. At the top of the list was “a tendency to avoid sexual health services, including being tested for HIV, for fear of being stigmatized by the health care providers or wider society”.
“We have had a situation where although HIV programs ought to be focused on key populations including men who have sex with men, there has been either a policy by certain governments not to pursue those approaches, or de facto non action on the part of state authorities responsible for providing services to these communities. That bit of evidence was very important in the case to buttress the legal arguments around discrimination,” explained Veronica Cenac, a St. Lucian attorney and one of the initiative’s leading strategists.
Now, with the law changed, comes the opportunity to improve a whole range of services. The legal change will save and change lives.
As activists celebrate, they are also highlighting the importance of reflecting and learning on how success was won, to help inform the efforts of others and to provide insights on the next steps needed in the journey to end stigma and discrimination.
The strategy that would finally topple the 19th century law was birthed seven years ago. Through this initiative, there was also a successful challenge of the “buggery” law in Antigua and Barbuda last month. Similar cases have been launched in Barbados, Grenada and St. Lucia.
The approach was inspired by recent Caribbean examples of using judicial review to overturn laws which criminalized lesbian, gay, bisexual and transgender (LGBT) people in Belize, Guyana and Trinidad and Tobago. But, led by the Eastern Caribbean Alliance for Diversity and Equality (ECADE), a consortium of attorneys, civil society groups and human rights trusts refined a distinct plan for taking aim at discriminatory laws in the Eastern Caribbean.
The ECADE process had three key features.
First, rather than focus on creating a high profile for the cases in the news, communication efforts were focused on raising awareness and harnessing the wisdom within communities. The team worked to identify strengths and allies, while planning to address potential pitfalls.
Secondly, the strategy was fundamentally based on institutional strengthening.
“It was not just about launching cases,” said ECADE Executive Director, Kenita Placide. “It was about building community.”
One of the claimants in the case was the non-governmental organization St. Kitts and Nevis Alliance for Equality (SKNAFE). SKNAFE Chair, Tynetta McKoy, revealed that the organization is poised to support the next stage of the work: increased public engagement.
“The majority of community members… know this is a first step and there is a lot of work still to be done around education and public awareness. Coming from the community level, this is a steppingstone. We are ready to keep on going,” she said.
The third prong of the strategy was the security of litigants and the wider community. ECADE noted the importance of thinking about claimants beyond the case and ensuring they could navigate their regular lives safely, particularly when their names and faces were circulating in the media.
ECADE highlighted their appreciation for inputs from the Human Dignity Trust, Kaleidoscope Trust, Canadian HIV/AIDS Legal Network, University of the West Indies Rights Advocacy Project (URAP) and Caribbean Vulnerable Communities (CVC) Coalition, amongst others, for contributing in various ways. These included supporting foundational research and offering strategic guidance.
Ms. Cenac noted that a subsequent phase of the strategy would be focused on encouraging governments to enact protective legislation. This would ensure that the LGBT community and other vulnerable groups are covered by the legal safeguards put in place for other citizens.
Lead attorney, E. Anthony Ross Q.C., called for Caribbean governments to act proactively to ensure their laws uphold citizens’ constitutionally guaranteed rights.
“Nothing new was created here [in this legal judgement ]. The constitution specifically gives those rights. Attorneys-General should take note. It’s time to look over all laws and bring these discriminatory laws in line.”
Our work




Feature Story
Successfully expanding the rollout of PrEP in Indonesia
01 September 2022
01 September 2022 01 September 2022While the number of new HIV infections in Indonesia decreased by 3.6% in 2021 to around 27 000, the country remains one of the countries with the highest number of new infections in the Asia and the Pacific region. Pre-exposure prophylaxis or PrEP is a medication that is highly effective at preventing HIV infection so making it available to groups of people most vulnerable is a key priority.
“In the past, I independently searched for information about PrEP because a client asked about it. I am glad there is a PrEP training that allows me to receive comprehensive information that I can then share with other people,” said Temmy a community outreach worker who participated in a training course in Bekasi.
PrEP was rolled out in Indonesia in 2021 as a pilot project to provide a new HIV prevention option which may be more convenient for people at risk of HIV, and to reduce new HIV infections among key populations such as sex workers and gay men and other men who have sex with men. It began in 12 districts, before expanding to 21 districts in 2022, with the aim of getting 7000 people on to PrEP.
As part of the expansion, a second round of training sessions was conducted in August across nine cities in Indonesia: Bogor City, Bogor Regency, Depok, Bekasi, Tangerang, Batam, Balikpapan, Samarinda, and Sidoarjo. Over 120 services providers from 24 hospitals and 47 outreach workers from local communities took part.
The PrEP training for health providers and community outreach workers was conducted by the Ministry of Health of Indonesia in partnership with Kerti Praja Foundation, Padjajaran University, and the national MSM-TG Network (GWL-INA). It was supported by donors, including the Global Fund to Fight AIDS, Tuberculosis and Malaria, USAID-PEPFAR and the Government of Australia’s Department of Foreign Affairs and Trade (DFAT).
"With less than a decade to go before our goal of ending AIDS by 2030, we must prioritize efforts to scale up combination prevention programmes, such as PrEP. The piloting of PrEP is critical to kickstart policy and programme development on PrEP in Indonesia. The conduct of training for service providers and community outreach workers is an integral part of the pilot implementation to ensure adequate capacities to provide PrEP services to communities in need,” said Krittayawan Boonto, the UNAIDS Country Director for Indonesia.
The PrEP training sessions are held over two days and include discussions between service providers and outreach workers. The aim is to equip and improve the capacity of the service providers and outreach workers to provide good quality PrEP services.
“This PrEP training has increased my knowledge of the alternative methods to prevent HIV. After this training, our health service office can now offer this new method of HIV prevention to our clients. We hope that this will contribute to the reduction of new infection risk. Thanks to this training, I have become more confident in providing PrEP services in the future,” said Doctor Elly from Lambuk Baja, Batam Province.
Unlike the first series of training sessions, the second was conducted in person and engagement was much higher. The enthusiasm also led to more active follow up after the training. One of the health centres in Bogor City started to provide PrEP services a couple of days after the end of the course. They also directly approached communities about the benefits of PrEP and within a month PrEP uptake had increased by 15%.
“As with all aspects of the HIV response, communities play a key role in the success of PrEP implementation. Contribution from the community is especially vital in the context of the pilot implementation in Indonesia, as communities of key populations with a substantial risk of HIV infection are the main beneficiaries of the programme,” said Muhammad Slamet, National Coordinator of the MSM-TG network (GWL Ina).
Region/country


Feature Story
UNAIDS responds to EU approval of a long acting HIV treatment option: “To end AIDS, share technology.”
23 August 2022
23 August 2022 23 August 2022Responding to the news that the European Commission has approved an HIV treatment option designed for twice-yearly dosing, UNAIDS Executive Director Winnie Byanyima said:
‘It is great news that a range of long-acting HIV treatment options are set to come on stream. A range of options for long-acting treatments, received every few months, could enable more people to get on treatment or offer better clinical options for patients showing resistance to current regimens, therefore staying longer on treatment, and prevent many AIDS-related deaths – if they become available for all who need them. The evidence is clear: monopoly production cannot ensure global availability and affordability. Worldwide availability of affordable long-acting treatments will require the transfer of technology to enable generic production.’
Progress in long-acting treatments follows progress in long acting prevention. The recent decision by ViiV to share its long-acting HIV prevention technology to enable generic production has demonstrated that sharing is possible for companies to do. UNAIDS welcomed that decision and is urging an expansion of the number of countries included. Currently, many upper middle-income countries do not have access to these technologies. Achieving global targets to end AIDS would require countries around the world have access to newer technologies. As a range of companies advance their development of long-acting HIV treatments, they should build on ViiV’s precedent, expanding the number of countries, and learn from it by not waiting until after launch to transfer the technology.
Ms Byanyima said:
‘Delays in the transfer of technology of innovative health products cost lives. The process of sharing of long-acting treatment technology, of the intellectual property rights and “recipes”, should not wait for after long-acting HIV treatment medicines are made available to people in rich countries. That process should begin at the early stages of the Research and Development (R&D) cycle. Sharing technology now, to help producers prepare, will save lives and help end the AIDS pandemic. The transfer of pandemic-ending technologies to low- and middle- income countries is not only the right thing to do, it is in the self-interest of rich countries too. We can only end AIDS by ending AIDS everywhere. To end AIDS, share technology. Now.’
Note
UNAIDS statement follows the announcement of EU approval detailed in this link: https://www.gilead.com/news-and-press/press-room/press-releases/2022/8/gilead-announces-first-global-regulatory-approval-of-sunlenca-lenacapavir-the-only-twiceyearly-hiv-treatment-option. UNAIDS statement is not a commentary on any individual medicine but on the advances being made in long-acting technologies and the need for such technology to be shared.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.



















