Feature Story
UNAIDS saddened by the death of Joe Muriuki
18 February 2022
18 February 2022 18 February 2022By David Chipanta, UNAIDS Senior Adviser, Social Protection
Joe Muriuki was a son of the African soil, born and raised in Kenya, a local, national and global advocate for the right of people living with HIV to access life-saving HIV treatment free from stigma and discrimination. In 1987, he became the first Kenyan and among the first of all people living with HIV in Africa to share publicly that he was living with HIV.
Mr Muriuki died from oesophagus cancer-related complications on 14 February 2022, having lived a healthy life with HIV for more than 36 years, thanks to his access to life-saving HIV treatment and through living his life with a sense of purpose.
Mr Muriuki fought against AIDS-related stigma and discrimination in his native Kenya at a time when an HIV diagnosis was thought to mean imminent death. He offered a testimony that a healthy life with HIV was possible. He formed the first support group of people living with HIV in Kenya, the Know AIDS Society, to encourage people living with HIV to overcome fear, stigma and discrimination and to advocate for changing policies and laws to remove AIDS-related stigma and discrimination.
After his HIV diagnosis, stigma and discrimination forced Mr Muriuki to leave his job, and he returned to his home city, Nyeri, to await his death. In Nyeri, the stigma and discrimination he experienced stopped him from opening a bank account. However, he overcame the obstacles in his path and decided to dedicate his life to a crusade against HIV. His courage and conviction to openly disclose his HIV status, and to fight AIDS-related stigma and discrimination, were heroic.
His campaigning also formed the foundation of Kenya’s national AIDS response, prompting the government to declare AIDS a national disaster before establishing the National AIDS Control Council in 1999. Mr Muriuki was also active globally, advocating for access to life-saving HIV treatment for people living with HIV in Africa and their greater involvement in the AIDS response. He served in the Network of African People Living with HIV, the Global Network of People Living with HIV, the International Treatment Preparedness Coalition and the Pan African Treatment Movement, among other organizations, advocating with candour for equitable access to HIV treatment for people living with HIV in Africa.
Although Mr Muriuki’s HIV was virally suppressed, from 2018 he struggled with cancer, eventually dying from its complications. He was worried that the AIDS response was ignoring noncommunicable diseases and in his work with Kenya’s HIV Tribunal he pushed for noncommunicable diseases to be brought to the forefront of the AIDS response.
Mr Muriuki will be sorely missed by his family, friends and colleagues in Kenya and around the world.
Watch
Region/country
Related





Feature Story
UNAIDS saddened by the death of Leonora Mathe
17 February 2022
17 February 2022 17 February 2022By Tabita Ntuli, UNAIDS Community Support Adviser, South Africa
If one word could define Leonora Nontokozo Mathe, AIDS activist and champion of key population rights, it is ubuntu—an African word with deep meaning that describes the character of people who recognize their shared humanity and humility. Born with HIV, Ms Mathe died this week after a long struggle with pneumonia.
Born and raised in Bulawayo, Zimbabwe, Ms Mathe was a phoenix who rose from the ashes after losing both of her parents at the tender age of 12 years. Ms Mathe was no ordinary person; she was an unforgettable icon who challenged HIV for the 31 years of her life. A quiet revolutionary, like still waters running deep, she was shy in her mannerisms, yet her advocacy spoke volumes. She knew how to listen attentively and was even better at speaking and expressing her mind in a way that advocated for the rights of people living with HIV.
Ms Mathe was a mother, sister and friend, a devoted advocate and champion of key population rights who was so softly spoken, loving and supportive. To know her personally meant you were exposed to her cheer and comical nature, for she was always cracking jokes and no one could hold back from laughing at some of the things she would say. She had the ability to make everything seem manageable, no matter how big or seemingly scary it was, and she spoke so candidly about her journey with HIV.
Ms Mathe travelled the world with her advocacy, visiting Namibia, Uganda, Rwanda, Morocco, Spain, the United Arab Emirates, Qatar, the Netherlands and Belgium, to name just a few of the countries she travelled to. A visionary and a leader who was starting her own organization, Hashtag InSolidarity, with the purpose of being more instrumental to key populations, she had partnered with a 14-year-old to help raise 100 000 crayons for needy kindergartens through a project called the Crayon Craze.
She wanted so much to empower women and girls through her organization and was in the implementation stages when her health became more challenging.
For the past three years, Ms Mathe was in and out of hospital, battling with pneumonia, yet she spoke which such lightness and understanding. She would say things like, “You know this body of mine has been through so many challenges due to being born with HIV, nothing shocks me any more about it, I just have to keep on fighting for my kids and my dreams to manifest before I die.”
Her dreams are as valid today as they were when she was alive. She experienced so many challenges with establishing her organization and trying to source funding and wanted to work with women living with HIV who are passionate about helping other women.
“Leonora Nontokozo Mathe was a tireless and passionate activist and leader who dedicated her life to championing the rights of people living with HIV and key populations and the empowerment of women and girls,” said Eva Kiwango, UNAIDS Country Director for South Africa. “We share in the sadness and offer condolences to her family and all who knew and loved her. She will be sadly missed.”
Ms Mathe was exceptional, phenomenal, wonderful, gifted and talented. A fiery soul whose light burned so brightly, particularly on key population matters, on which she unapologetically spoke about issues that needed urgent attention and addressing.
A light that burned so beautifully shall never be forgotten—her legacy lives on.
Region/country
Related




Feature Story
Networks led by young people in Asia and the Pacific find ways to adapt to COVID-19 and deal with uncertain futures
09 February 2022
09 February 2022 09 February 2022Health systems and communities have been pushed to the breaking point by the COVID-19 pandemic, a pandemic that the world was woefully unprepared for. Two years on, networks of key populations and people living with HIV are still at the forefront of the COVID-19 response, working to ensure that communities have access to timely and undisrupted HIV services. Among them is Youth LEAD, the network of young key populations in Asia and the Pacific, which in 2020 established the YKP COVID-19 Emergency Relief Fund to support initiatives led by young people in Asia and the Pacific.
One of the beneficiaries is Ya_All, an organization for young lesbian, gay, bisexual, transgender and intersex (LGBTI) people based in Manipur, India. “The second COVID-19 wave hit north-east India really hard, as it did across the country. We saw health-care systems collapse in front of our eyes. This greatly affected our work as we saw more and more young key populations experience delays in accessing HIV prevention services and saw an increase in mental health issues,” said Sadam Hanjabam, the founder and Chief Functionary of Ya_All. Thanks to the YKP COVID-19 Emergency Relief Fund, Ya_All supported 300 young LGBTI people and members of other key populations to access telecounselling services in five districts to help them with depression and other mental health issues.
Since the outset of the COVID-19 pandemic, the YKP COVID-19 Emergency Relief Fund has helped organizations led by and serving young people implement programmes that ensured young key populations and people living with HIV were not left behind in the HIV and COVID-19 responses. This included providing essential food and supplies of personal protective equipment, information on HIV and COVID-19 prevention and continued access to HIV prevention and treatment services, including mental health services. It also included establishing harm reduction programmes, distributing seed funding for businesses led by transgender people, providing housing and supporting digital and peer-led initiatives.
Funded through the Robert Carr Fund, the AIDS Health Care Foundation and the UNAIDS Regional Support Team for Asia and the Pacific, the YKP COVID-19 Emergency Relief Fund has supported more than 20 projects from 15 organizations led by young people across the region, and has made a considerable difference to the lives of young key populations.
The Viet Nam Young Key Populations Network is one of the beneficiaries of the fund in Viet Nam. Even though the country was in complete lockdown for a substantial period, with a seed grant the network managed to produce HIV and sexual and reproductive health and rights digital educational content for young people at risk of HIV, distributing harm reduction materials to 15 provinces across the country.
Similarly, YPEER Pilipinas, another beneficiary of the fund, trained 1000 young people on HIV combination prevention strategies and screened more than 900 young people for HIV. With a small grant, they were able to scale up the #GetCondomPH Programme, which resulted in successfully distributing more than 11 000 condoms across the Philippines.
In Cambodia, KHANA has given mental health support training to more than 70 LGBTI leaders. The training accelerated ongoing mental health peer support to key affected populations who were experiencing mental health issues. “Online counselling sessions on how to cope with mental health issues were incredibly helpful. The YKP COVID-19 Emergency Relief Fund was an effective mechanism that allowed us to provide timely support to young people in need of HIV prevention and other health services,” said Phorng Chanthorn, Senior Coordinator at KHANA.
These few examples out of the many show that young people, communities and civil society play a crucial role in pandemic responses, helping HIV programmes rebound and adapt to COVID-19 rapidly. Still, these efforts have not been easy. “Youth networks are trying to find ways to recover, adapt and effectively lead in this new funding landscape that has resulted in greater competition for donor funding. Many programmes, including this one, showcase the impact and necessity of supporting youth-led HIV programmes and initiatives. However, it’s not enough,” said Vanessa Monley, Programme Officer at Youth LEAD.
In 2020, young people accounted for 26% of new HIV infections in Asia and the Pacific. In some countries, close to half of new HIV infections were among young people, and one in three members of young key populations do not know their HIV status.
“It is critical to find innovative ways to continue to scale up access to HIV services for young key populations in the context of COVID-19, ensuring that we do not give up achieved gains, and to respond to the additional issues that have come with the pandemic, such as mental health and social support issues. UNAIDS is fully committed to supporting responses led by young people and ensuring their sustainability as we work collectively to end AIDS by 2030,” said Taoufik Bakkali, Director, a.i., of the UNAIDS Regional Support Team for Asia and the Pacific.
Our work
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa




Feature Story
Fostering creativity to recover better from COVID-19
08 February 2022
08 February 2022 08 February 2022“Throughout the COVID-19 pandemic, I started seeing people around me getting laid off and many struggled to find new jobs. Many people, myself included, started to consider starting our own businesses to sustain our livelihoods in this challenging time,” said Abraham, who is a member of a young key population community in Jakarta, Indonesia.
People in vulnerable groups have been facing huge hardships during the COVID-19 pandemic. According to a survey conducted by the Crisis Response Mechanism Consortium in 2021, 79% of lesbian, gay, bisexual, transgender and intersex respondents were not working owing to the COVID-19 pandemic.
As an effort to support the livelihoods of people living with HIV and key populations, the International Labour Organization (ILO) and the UNAIDS Country Office for Indonesia partnered to conduct a training programme for more than 40 participants on fashion design and production and entrepreneurship from July to November 2021.
“As soon as I heard about this training, I was immediately intrigued because I am interested in fashion and I’m always open to try new things,” said Abraham, who was one of the participants of the training, which was facilitated by the Yayasan Rame Rame Jakarta and Kami Latu Initiative nongovernmental organizations. Classes, both online and face to face, were given on colour theory, pattern development, product development, strategic marketing, financial management, product story-making and product-making.
“I was very excited to be a part of the training and I had a lot of fun! The lessons were very useful for someone like me who is interested in starting my own small business, especially through e-commerce platforms. I gained business skills that are vital to entrepreneurship, such as marketing, calculating profits and understanding our products,” reflected Abraham. “And I also enjoyed that there were some practical sessions where we learned how to use the sewing machine to make accessories and to be creative in refurbishing traditional fabrics or plain old materials to create new improved fashion items.”
During the training programme, Abraham made earrings, bracelets and clothes alongside other enthusiastic participants. The camaraderie of the participants was strong, especially as they gathered for a fashion show and photo shoots to display their creations. Abraham stressed that these kinds of trainings are beneficial for key population communities and that, “While such training isn’t exclusively needed for key populations, it isn’t always the case where trainings provide a safe space to express oneself freely without fear of judgement.”
In addition to participants from communities of people living with HIV and key populations, workshops were also held for women in two villages in East Nusa Tenggara, namely Nggela and Manggarai Barat. The workshops provided them with skills that complement their traditional cloth (tenun) weaving, such as design skills to develop fashionable products using Indonesia’s traditional fabric and entrepreneurship skills, in an effort to improve their incomes and livelihoods.
Krittayawan Boonto, the UNAIDS Country Director for Indonesia, said, “As we enter the third year of the COVID-19 pandemic, vulnerable communities, such as people living with HIV and key populations, still need continued support and assistance to recover from economic hardships.”
In 2022, UNAIDS and the Yayasan Kusuma Buana nongovernmental organization will work together to ensure the participation of people living with HIV and key populations in the entrepreneurship trainings. Ms Boonto continued, “The entrepreneurship trainings offered through this joint United Nations project provide opportunities for vulnerable populations to apply their talents and find creative solutions to overcome challenges.”
The training programme is part of the activities under the United Nations COVID-19 Response and Recovery Fund for Employment and Livelihood, implemented jointly in Indonesia by ILO, UNAIDS, the United Nations Development Programme and the Office of the United Nations High Commissioner for Refugees.
Region/country




Feature Story
UNAIDS Solidarity Fund helps female sex workers in Ghana
04 February 2022
04 February 2022 04 February 2022Growing up in Jamestown, one of the oldest districts of Accra, Ghana, Susana Dartey saw the daily abuse and exploitation faced by female sex workers, which inspired her to set up the Women of Dignity Alliance (WODA) to empower female sex workers and fight the inequalities they face.
“Since sex work is illegal in Ghana, our members have been faced with a lot of abuse and cannot report this due to the fear of being arrested,” says Mrs Dartey, who serves as the Executive Director of WODA. WODA has grown from one member in 2016 to a team of 16 staff members, comprised of current and former female sex workers. “Belonging to the same neighbourhood, I found my voice through theatre and realized that I could use the same methodology or technique to give a voice to these women,” she added.
In Ghana, there are two categories of female sex workers—so-called roamers and seaters. Roamers are mobile and travel to clients, whereas seaters are stationary and work out of their homes or brothels. In 2020, HIV prevalence among female sex workers in Ghana was estimated to be 6.9%.
The COVID-19 pandemic has been challenging for sex workers in Ghana, with lockdown restrictions hampered their ability to work. Sex workers in the country have also reported feeling left out of the official support being given to society as a whole during the pandemic.
In the face of these obstacles, Mrs Dartey is determined to empower female sex workers to become role models for women in their community through the Women Empowered Through Social Entrepreneurship project, which is supported by the UNAIDS Solidarity Fund.
To address the socioeconomic problems brought about by the COVID-19 pandemic, WODA is nurturing promising social enterprises that are established, led, sustained and scaled up by the sex workers themselves, with the aim of empowering up to 400 sex workers, either directly or indirectly.
The three areas addressed by the programme are training on sustainable income generation, facilitation of COVID-19 prevention among sex workers and creating an opportunity for sex workers to be agents of change within their communities.
Mrs Dartey explained how the sex workers are undergoing training in skills as diverse as beauty treatment, soap-making, confectionery production, breadmaking and floral decoration. The beneficiaries of the project are educated in the operating practices of social enterprises and are given opportunities to learn entrepreneurial skills from experts.
“As a roamer for eight years, I have never experienced the kind of hardship COVID-19 has brought to my work. Before COVID-19 set in, I could make up to 230 Ghana cedis daily, but these days it’s very difficult to even make 50 Ghana cedis. When Susana informed me about the UNAIDS Solidarity Fund supported initiative, I was so glad. I love to make ladies look good, so I am eagerly looking forward to acquiring skills in pedicure, manicure and make-up artistry to earn a livelihood,” said one of the beneficiaries.
A part of enabling key populations and vulnerable communities to survive the hardships brought about by the COVID-19 pandemic is to support sustainable income-generating solutions that emerge from those communities. The UNAIDS Solidarity Fund was established to highlight the ingenuity of key populations by enabling access to finance for establishing sustainable social enterprises.
“My hope is to bring these women together to set up a goal for themselves. This project is looking at their future and at the end of the project the sex workers will have set up social enterprises that belong to them,” said Mrs Dartey when asked about her hopes for the project.
A beneficiary of the project who aspires to establish a make-up studio said, “I met Susana in the early part of 2021 and that was the beginning of a new me. Through WODA, I can now boast of some skills in make-up artistry and wig cap-making.” She also calls for sex work to be legalized. “I want sex work to be made legal so that the police will stop arresting and abusing us,” she added.
Region/country
Related
 Impact of US funding cuts on HIV programmes in Ghana
Impact of US funding cuts on HIV programmes in Ghana

08 April 2025

Feature Story
Consultation calls for the global AIDS response to build on emergency adaptations to COVID-19, tackle structural barriers and ensure that country programmes fully recover from COVID-19 disruptions and end AIDS
03 February 2022
03 February 2022 03 February 2022As the Omicron variant surges through communities and health systems already stretched to the breaking point by two years of COVID-19, HIV programme managers and community representatives gathered virtually to review efforts to keep the AIDS response on track and propose ways to better overcome the challenges caused by two clashing pandemics.
“The COVID-19 pandemic has disrupted health services worldwide, at different times and in different ways, and it continues to do so,” UNAIDS Deputy Executive Director, Programme, a.i., Eamonn Murphy said at the opening of the consultation. “But at the same time we’re hearing great successes. Stories and data of impressive resilience and programmatic rebound are increasingly being documented and researched.”
The participants identified the most effective innovations that have allowed HIV services to continue to reach those who need them the most and proposed follow-up research and actions that can help guard against future waves of COVID-19 infections.
“We have learned so much over the past two years of the COVID-19 pandemic. Anticipating the worst, countries and communities rallied effectively to adapt and maintain most HIV services. These global efforts have meant that although there have been gaps and disruptions to services, and some catch-up will be needed, most people living with HIV continued successfully on treatment,” said Meg Doherty, the World Health Organization (WHO) Director of Global HIV, Hepatitis and STI Programmes.
Networks of people living with HIV and key populations at higher risk of HIV infection warned that the often life-saving adaptations made to HIV services have not addressed the stigma, discrimination and structural barriers they face in their day-to-day lives. In addition, COVID-19 has left many even more vulnerable to depression, violence and other harms.
“People are working hard to ensure that treatment is still available and accessible, but people have also lost livelihoods during COVID-19, and they have taken on additional community and family responsibilities,” said Florence Anam, a Programme Manager at the Global Network of People Living with HIV (GNP+). “Strengthening of community systems of health, and the integration of mental health and psychosocial support is more important now than ever. We need to focus on reducing inequities and ensuring that people are economically empowered enough to meet their basic needs as much as possible.”
Country data collected by UNAIDS, WHO, the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and the United States President’s Emergency Plan for AIDS Relief (PEPFAR) show that HIV service disruptions were most severe during the first lockdowns that many countries put in place in early to mid-2020. A combination of movement restrictions and health systems overwhelmed by COVID-19 cases cut off many people living with HIV from the daily medicines they need to stay healthy. HIV testing, the enrolment of people newly diagnosed onto treatment and the provision of HIV prevention tools such as condoms and pre-exposure prophylaxis nearly ground to a halt. Voluntary medical male circumcision, health services for transgender people and other elective medical procedures were suspended altogether in many countries.
Prolonged service interruptions could have led to a wave of AIDS-related illnesses and deaths, undermining decades of efforts to contain the HIV virus. Programmes across the world scrambled to find new ways to reach people living with HIV and the key populations who are at highest risk of HIV infection.
These measures included working with affected communities to deliver antiretroviral medicines door to door and to increase the quantity of medicines provided during each visit in order to reduce the frequency of medical appointments. This multimonth dispensing of antiretroviral medicines has been recommended by WHO since 2016, as it is easier for the patient and reduces the workload of the health system.
Most HIV treatment programmes quickly rebounded after adaptations were put in place.
“The data show that most national HIV treatment programmes in low- and middle-income countries responded with extraordinary resilience to protect 20 years of hard-earned gains through rapid adoption of COVID-19 adaptations,” said Siobhan Crowley, Head of HIV at the Global Fund. “The strong HIV services platform and highly engaged HIV civil society are well poised to serve as an important foundation for integrated services to tackle COVID-19 and other public health threats, but increased investment from all stakeholders is needed to sustain and build on these impressive achievements.”
Irum Zaidi, the Deputy Coordinator at the Office of the United States Global AIDS Coordinator, stressed that the strengthening of health information systems and the adoption of people-centred approaches in the years before COVID-19 was critical to the rapid reaction to the challenges created by the new pandemic.
“Over the past four years, PEPFAR and partner country governments collaborated to implement WHO policies and adaptations for providing people-centred clinical HIV services,” Ms Zaidi said. “These adaptations were rapidly scaled during COVID-19, establishing a flexible service delivery environment to keep individuals on lifelong antiretroviral therapy during COVID-19 surges. Granular real-time data along with PEPFAR’s commitment provided a path forward to support governments and beneficiaries during this unprecedented time.”
Efforts to expand access to a relatively new and promising HIV prevention option—antiretroviral medicines pre-emptively taken by people at higher risk of infection, known as pre-exposure prophylaxis, or PrEP—were also rapidly adjusted to overcome COVID-19 challenges. Those adaptations have included the shifting of clinical consultations to telemedicine and outdoor settings, the use of social media for virtual adherence support and home delivery of PrEP pills. Expansion of self-testing for HIV has helped to maintain the expansion of both PrEP and HIV treatment.
“We need to keep building the resilience that HIV services have shown by prioritizing person-centred differentiated service delivery in response to challenges posed by COVID-19,” said Adeeba Kamarulzaman, the President of the International AIDS Society.
The consultation looked ahead to a future where the COVID-19 response transitions from an acute pandemic phase to a more sustained control programme, similar to the responses to HIV, tuberculosis and other infectious diseases.
The participants agreed that, even within a best-case scenario, it will be important to build on emergency adaptations by establishing a more enabling environment for the populations who currently struggle to access services, and to ensure that HIV programmes can fully recover from COVID-19 shocks and reach the global goal of ending the AIDS pandemic by 2030.
“Perhaps one of the silver linings of the COVID-19 pandemic is how it sparked innovation and inspired their rapid adoption by countries and communities. These will have not only a positive and durable effect on the HIV response but offer models for others to adapt in tackling other health challenges,” said Wafaa El-Sadr, the founder and Director of ICAP.
The consultation, held on 1 and 2 February, was co-organized by UNAIDS, WHO, the Global Fund, PEPFAR, the International AIDS Society and ICAP at Columbia University.


Feature Story
The importance of engagement of community organizations to ensure the sustainability of HIV services in eastern Europe and central Asia
02 February 2022
02 February 2022 02 February 2022Participants from 21 countries in central and eastern Europe and central Asia and the Balkans met in December 2021 in Istanbul, Turkey, for the International Health Sustainability Forum: HIV and COVID-19 in Eastern Europe and Central Asia.
The participants discussed the most efficient means to ensure the sustainability of AIDS programmes and the role of community organizations in providing uninterrupted HIV services during the COVID-19 pandemic in the region.
The results of a three-year project implemented by the Alliance for Public Health in a consortium with 100% Life (formerly the All-Ukrainian Network of People Living with HIV), the Central Asian Association of People Living with HIV and the Eurasian Key Populations Coalition, with the participation of a wide range of partners, were also presented and reviewed. The project was funded by the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and was supported by UNAIDS.
Addressing the forum, Peter Sands, the Executive Director of the Global Fund, highlighted the key elements of successful AIDS programmes in the region, among them “systems, not project-based interventions,” the meaningful engagement of communities and their ownership of the HIV response and removing human rights barriers.
“Increasing public funding of HIV services through social contracting mechanisms, which was a rare case a few years ago, has now become an important component of a systemic response to the HIV epidemic in many countries of the region,” said Andriy Klepikov, the Executive Director of the Alliance for Public Health. He noted that over the past three years public funding of HIV services through social contracting mechanisms in the region amounted to more than US$ 30 million. “This is one of the most important achievements of the joint efforts of community organizations and governments in the region.”
However, as the participants noted, to sustain this success an appropriate legal framework, the support of governments and the strengthening of initiatives made by communities are needed.
Several cities across the region have produced impressive results due to the leadership of local governments that have not only taken responsibility for developing and funding municipal AIDS programmes, including services for key populations, but also through the involvement of community organizations in their implementation.
Thus, systematic work by the city government in close cooperation with community organizations saw Odesa, Ukraine, achieve the 90–90–90 targets. “Odesa has managed to change the strategy for HIV testing and treatment. Our experience has already received recognition from the international community. And we are ready to share our best practices and successes,” said Gennadiy Trukhanov, the Mayor of the city.
The experience of the Republic of Moldova was presented by Fadei Nagachevsk, the Vice-Mayor of Chisinau, and Ruslan Poverga, from Initiative Positiva, who demonstrated the importance of close interactions between city governments and community organizations to ensure the accessibility of services for key populations. Mr Poverga also noted that the integration of peer consultants and social workers in public institutions helps to ensure the sustainability of services.
The best practices of municipal responses to the HIV and COVID-19 epidemics of Kyiv, Ukraine, Osh, Kyrgyzstan, Podgorica, Montenegro, Kragujevac, Serbia, Bern, Switzerland, Prague, Czechia, and Istanbul, Turkey, were also presented.
According to Sergiy Dmitriev, an international expert on public health, civil society organizations have also played a leading role in reducing the prices of antiretroviral medicines by monitoring the procurement cycle and budget and attracting generic suppliers. The price of an annual course of first-line antiretroviral therapy has decreased to US$ 131—the average cost of first-line antiretroviral therapy in nine countries in the region was US$ 192 in 2017. Most of the savings on purchases, about US$ 119 million, remained within AIDS programmes.
Another critical area where community organizations have been playing an increasingly important role in the region is community-led monitoring of human rights violations. The results of work on the REAct system (a human rights violation monitoring system) were presented: during 2020 and 2021, more than 6000 cases of human rights violations and cases of stigma and discrimination were registered in seven countries.
Among the most frequent offences in the region are violence by law enforcement officials, denial of access to medical services, disclosure of medical data and stigma in health-care settings, as well as physical violence against women by their partners and relatives. Based on an analysis of all cases, civil society organizations, together with lawyers and governmental partners, developed recommendations for countries that will form the basis for further advocacy.
“Community-led organizations have become leaders in providing people-centred, human rights-based HIV services in the majority of countries in eastern Europe and central Asia,” said Alexander Goliusov, Director, a.i., UNAIDS Regional Support Team for Eastern Europe and Central Asia. “Their meaningful engagement in decision-making processes and financial sustainability provided by government funding are the key for an effective response to HIV and COVID-19 and for future pandemics.”
The forum video is available: in Russian and English
https://www.youtube.com/watch?v=gCVqVUKAJmo
https://www.facebook.com/AlliancePublicHealth/videos/4581620981957116
Region/country
- Eastern Europe and Central Asia
- Albania
- Armenia
- Azerbaijan
- Belarus
- Bosnia and Herzegovina
- Bulgaria
- Croatia
- Cyprus
- Czechia
- Estonia
- Georgia
- Hungary
- Kazakhstan
- Kyrgyzstan
- Latvia
- Lithuania
- Montenegro
- Poland
- Republic of Moldova
- Romania
- Russian Federation
- Serbia
- Slovakia
- Slovenia
- Tajikistan
- North Macedonia
- Türkiye
- Turkmenistan
- Ukraine
- Uzbekistan
Related


Feature Story
New report highlights vital role of community-led organizations in pandemic response and preparedness
28 January 2022
28 January 2022 28 January 2022In a new UNAIDS report, Holding the line: communities as first responders to COVID-19 and emerging health threats, organizations led by and for people living with HIV and key populations detail their efforts to respond to the colliding pandemics of COVID-19 and HIV. Drawing on qualitative survey data spanning 225 community-led organizations across 72 countries, the report provides a snapshot of the organizations’ work during early 2020 to sustain the HIV response while supporting their communities through the COVID-19 pandemic. The report also illuminates the high-priority actions that are still urgently needed to ensure the continuity of HIV-related services, as well as the sustainability of the community-led organizations providing them.
In community members’ own words, the report tells a story of the phenomenal resourcefulness of community-led organizations to mobilize when and where governments could not. Their stories show that organizations led by and for people living with HIV and key populations, including women and young people, have leveraged in-depth HIV knowledge into broader pandemic expertise. In the face of service interruptions, health commodity shortages, curfews and severe funding gaps, the organizations adapted rapidly to continue providing HIV-related services.
Community-led organizations reported becoming more involved in distributing antiretroviral medicines and self-testing kits, negotiating with government officials to ensure that medicines would be accessible and personally delivering them to beneficiaries. Many organizations also reported shifting their services online, as well as relying on telephone and email contact for personal counselling and monitoring of health status, with some even making home visits in urgent circumstances. Material support, including food packages and income supplements, was mobilized and distributed to those in greatest need.
Organizations also undertook COVID-19-related service provision. They began outreach to community members and the broader public to raise awareness about COVID-19 and share information about how people could protect themselves. They detected and responded to rising levels of gender-based violence, providing assistance and support to survivors. They also distributed masks, soap and hand sanitizer, and constructed handwashing facilities. When the cost and availability of masks and soap became an issue, many community-led organizations reported finding innovative ways to produce these items themselves.
However, the majority of these organizations were distressed that their absence—especially from planning and decision-making processes—was resulting in the failure of national COVID-19 responses to address the needs of their communities. They repeatedly expressed deep concern about the economic impact of lockdowns and travel restrictions on their beneficiaries. They also highlighted continuing difficulties in obtaining personal protective equipment and travel approval, public transport or private vehicles for their staff.
Organizations reported shouldering extremely heavy burdens with little external support. Intense funding gaps left staff in these organizations exhausted and working nights and weekends to fundraise, usually unsuccessfully, with some even turning to their own personal salaries and savings to help their communities.
Community-led organizations are at the heart of a people-centered, human rights-based public health response. UNAIDS has repeatedly called for support and funding for community-led infrastructure, emphasizing that communities urgently need the space and the resources to lead.
“Community-led organizations have guided us through two pandemics, first the AIDS pandemic and now COVID-19,” said Winnie Byanyima, Executive Director of UNAIDS. “Their central and critical role in providing services at the heart of communities, reaching the most vulnerable, must be recognized and valued. Collectively, we must do more to support them financially, engage them meaningfully in decision-making processes and ensure they have all the resources they need to continue their work in responding to HIV and COVID-19 and for future pandemics.”
Where public health systems have engaged community-led networks and organizations and empowered those most affected by pandemics, they have been more successful at countering disinformation, ensuring the continuity of health services and protecting the rights and livelihoods of the most vulnerable. This is what it means to put people at the centre of pandemic responses.
In order to ensure the sustainability of a community-led HIV response, the report calls for five measures to be adopted as a matter of urgency:
- Community-led organizations must be fully included and integrated into national pandemic responses, including the continuing COVID-19 responses. This cannot be limited to consultation and should take place at the level of policy development, planning, design and evaluation of interventions.
- Short-term emergency funding must be mobilized and made readily available to community-led organizations.
- A stable, long-term funding base must be established to enable community-led organizations to function effectively.
- The information base on the work of community-led organizations must be expanded and deepened through systematic documentation, identification of good practices and information-sharing.
- Continuity of HIV-related services must be guaranteed, including through expanding funding to community-led organizations and establishing collaborative arrangements between community-led organizations and medical facilities to ensure sustainability of the HIV response through COVID-19 and future pandemics.




Feature Story
Love and condoms: broadcast on the importance of condoms in eastern Europe and central Asia
05 January 2022
05 January 2022 05 January 2022On the eve of World AIDS Day, the Russian language social media network OK.RU hosted a live broadcast, Telling the Truth, as part of an education project that has been run by UNAIDS and the United Nations Educational, Scientific and Cultural Organization since 2015. The show was organized in collaboration with a popular magazine, Domashniy Ochag, and was devoted to the use of condoms and the link to the HIV epidemic in eastern Europe and central Asia.
During the broadcast, which was watched by more than 1 million people, experts and celebrities discussed the most common myths, misconceptions, difficulties and fears connected to condom use.
Before the broadcast, an online survey of 1050 people aged 18 to 60 years was conducted on what Russian Internet users think about protection against sexually transmitted infections and what they consider to be safer sex. The study found that 87% of respondents had had sex without a condom, with older respondents reporting higher rates of sex without a condom.
“HIV has already reached the general population in this region. Almost 70% of all new HIV infections have been linked to heterosexual sex in recent years. At-risk people include single women aged more than 35 years and men and women who no longer worry about contraception and therefore do not use a condom,” said Natalya Ladnaya, Senior Researcher at the Central Research Institute of Epidemiology, Rospotrebnadzor.
Among the reasons for unprotected sex, the respondents most often named “awkwardness of discussing it with a partner”, which was reported by 41% of the respondents. In addition, “trust in a partner” (35%), “discomfort during intercourse” (20%), “fear of spoiling romance” (31%) and “fear of being misunderstood by a partner” (19%) were listed among the reasons for not using a condom.
Appearing on the broadcast was Masha Godlevskaya, who has been living with HIV for 22 years. She works as a peer consultant for the EVA Association, which provides HIV services. She explained that many women who go to the EVA Association for a consultation are embarrassed to carry condoms because of the stereotype that having a condom available means that they are available and ready for sex.
“Both women and men are victims of this story,” said Ms Godlevskaya. “If a man insists on having sex without a condom, the woman should be ready to say: “I don’t want to. I don’t want to offend you, but no sex without a condom.””
“We help women believe in themselves, work with a psychologist, fight back against their abusers, build new relationships where they can discuss everything frankly. I want our women to be able to defend their bodies, their rights, and be able to take their lives into their own hands,” she added.
Vera Brezhneva, UNAIDS Goodwill Ambassador for Eastern Europe and Central Asia, noted that many women vulnerable to HIV were born in the time of the Soviet Union, when there was no promotion of safer sex. “I didn’t know about HIV at all. Most of us at that time were afraid of pregnancy only. We believed in love as if love protects you from everything. We were not told that a condom is not protection against men or women but protection against infections.”
Ms Godlevskaya shared her story of becoming infected with HIV. “I was 16 years old. He was my first love, and, as it seemed to me then, the last one. It was a serious relationship, there was trust and we knew nothing about the need to use a condom.”
Marina Travkova, a family psychologist and sex therapist, noted that adolescents are vulnerable to HIV and other sexually transmitted infections. “They need help. There is nowhere to get reliable information. I am in favour of compulsory sex education in high school and for condoms to be available in school toilets. I always remind my sons before they go out: wallet, phone, brain, condom,” she said.
For a significant part of the population, especially young people, the cost of condoms is too high, noted Ms Ladnaya. “We are discussing these issues with partners, and we hope that there will be government programmes to support the production of condoms. There are nongovernmental organizations that provide condoms for free, but I believe that they should be available at every step,” she said.
Discussing the perception that sex with a condom is worse than sex without one, the reason that people often do not use condoms, the panellists noted that comfort might be related to the quality and size of a condom, as well as insufficient knowledge of how to use a condom and lubricant correctly.
Grisha Tumanov, a journalist and blogger and author of the Man, Where Are You Going? podcast, commented on a viewer’s question: “Is a condom needed if it’s love, which presupposes mutual trust.” He noted that, “We don't have a culture of speaking on sensitive topics, what you expect from relationships, including sexual relationships. And love does not absolve one of responsibility. This does not happen in adulthood. You are responsible for each other.”
Our work
Region/country
- Eastern Europe and Central Asia
- Albania
- Armenia
- Azerbaijan
- Belarus
- Bosnia and Herzegovina
- Bulgaria
- Croatia
- Cyprus
- Czechia
- Estonia
- Georgia
- Hungary
- Kazakhstan
- Kyrgyzstan
- Latvia
- Lithuania
- Montenegro
- Poland
- Republic of Moldova
- Romania
- Russian Federation
- Serbia
- Slovakia
- Slovenia
- Tajikistan
- North Macedonia
- Türkiye
- Turkmenistan
- Ukraine
- Uzbekistan
Related

Feature Story
New indicators added to Key Populations Atlas
06 January 2022
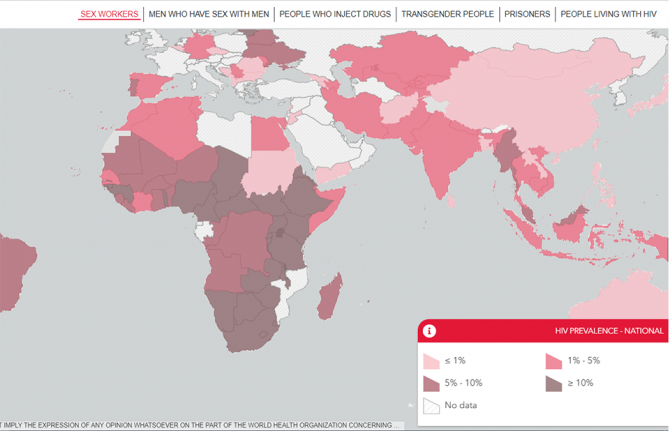
06 January 2022 06 January 2022The UNAIDS Key Populations Atlas is an online tool that provides a range of information about members of key populations—sex workers, gay men and other men who have sex with men, people who inject drugs, transgender people and prisoners—worldwide, together with information about people living with HIV.
Information about gay men and other men who have sex with men has been expanded with the inclusion of 11 new indicators from the EMIS and LAMIS projects. Under funding from the European Commission, EMIS-2017 collected data from gay men and other men who have sex with men in 50 countries between October 2017 and January 2018. LAMIS is the Latin American version of EMIS and finished data collection across 18 additional countries in May 2018.
The 11 new indicators shown in the Key Population Atlas—on syphilis, symptomatic syphilis, gonorrhoea, symptomatic gonorrhoea, chlamydia, symptomatic chlamydia, sexually transmitted infections testing, syphilis partner notification, gonorrhoea partner notification and hepatitis A and B vaccination—were chosen because of their high relevance to the communities.
Community-led and community-based infrastructure is essential for addressing the inequalities that drive pandemics such as the AIDS and COVID-19 pandemics, as well as for ensuring the continuity of health services and protecting the rights and livelihoods of the most vulnerable. The EMIS and LAMIS findings will be important for informing civil society organizations working on sexual health, HIV prevention and sexual minority rights and for policymakers, non-community prevention planners, epidemiologists and modellers.
“To leave no one behind, we need people-centred data collection that spotlights the inequalities that are hampering access to services. It is critical to understand who are the most affected and unable to access services. This will enable the European Commission, European Union Member States and civil society and community organization alike to address the specific needs of gay men and other men who have sex with men,” said Jantine Jacobi, the UNAIDS representative to the European Union.
Civil society and community-based organizations, especially those led by key populations, can complement traditional health systems’ pandemic responses, but this requires that they be treated as full partners—involved in governing, designing, planning and budgeting pandemic responses––with the technical and financial support to do so effectively.
The findings of the new indicators will help to increase the role of partnerships and communities across each country and will serve as the basis for decision-making and policy planning. For example, in Ireland, the EMIS-2017 National Report acknowledges that, “there has been an increase in HIV and STI testing compared to previous surveys and this is in some part due to the positive interventions carried out by stakeholders and the MSM [men who have sex with men] community in response to findings from previous surveys. Some of these positive interventions in relation to HIV testing can also be attributed to the increased availability of community testing.”